Introduction
Ankle sprains are a common reason for presentation to the emergency department, accounting for approximately 7% to 10% of visits and up to 40% of all sports injuries.[1] The majority of ankle injuries are sports-related and involve the lateral ankle compartment. The lateral ankle ligaments consist of the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL). Differentiating between ATFL-superimposed CFL injuries vs. isolated CFL injuries are challenging as clinical exams yield low sensitivities; however, it is commonly accepted that the ATFL is largely involved in the majority of ankle sprains, accounting for two-thirds of lateral ankle injuries.[2] While there is limited literature available for isolated CFL injuries, combined ATFL and CFL involvement are the second most common injury pattern of the lateral ankle.[3] As such, discussions about CFL injuries in the literature are largely embedded in lateral ankle injuries. This article will discuss the shared characteristics of lateral ankle injuries and identify the unique qualities of CFL injuries.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Sports activities account for a large percentage of lateral ankle injuries. Specifically, indoor and court sports sustain the highest risk for an ankle injury.[4]
Epidemiology
Isolated CFL injuries are rare as reported incidences are commonly classified under lateral ligament injuries. Thirty thousand ankle sprains occur each day, accounting for 25% to 40% of sports injuries. The lateral ligament compartment is involved in 85% of ankle injuries, with a daily incidence of one in 10,000.[1][5][6]
Pathophysiology
The CFL measures approximately 20 mm long with a diameter of 6 to 8 mm, originating at the anterior lateral malleolus and attaching to the posterior lateral tubercle of the calcaneus.[3] The fibularis brevis and longus tendons and their sheaths cross over the CFL ligament. The CFL is reinforced by either the lateral talocalcaneal ligament or anterior talocalcaneal ligament, in 35% and 42% of cases, respectively.[7] The CFL resists inversion in both plantarflexion and dorsiflexion and stabilizes the subtalar joint during plantarflexion. While combined inversion and supination is the mechanism of injury to the lateral ankle, an isolated CFL injury occurs from inversion in extreme dorsiflexion.[3][6] The CFL can sustain a loading force of 109 plus or minus 28 N, and while working with ATFL stretch during high-grade ankle sprains, it can withstand a force of 345 N.[1]
History and Physical
History and physical examination are important in triaging injuries for proper interventions. Patients may endorse cracking sound, swelling, redness, pain, and cessation of activities. As such, physical examination should focus on inspection, palpation, and special maneuvers such as anterior drawer test, and talar tilt test.[8] The anterior drawer test involves a patient with the foot in a neutral position while the examiner places anterior force onto the ankle. Laxity of the injured ankle in comparison to the unaffected foot is positive for anterior drawer test.[9] Similarly, the talar tilt test can be performed with the patient’s foot in a neutral position as the examiner exerts a tilting force to invert the ankle. The injured ankle is compared to the unaffected side for laxity. [10] As such, the anterior drawer and talar tilt test can be subjective. Following the initial assessment, physical findings of ecchymosis with localized pain on palpation 4 to 5 days post-trauma carry a 90% chance of lateral ligament rupture.[8] Patients with tenderness to palpation over the CFL have a 72% risk of ligament injury.[3] The Ottawa ankle rule on initial assessment for radiographic stewardship utilizes palpation of four locations of pain (posterior edge or tip of either malleolus, navicular bone, or base of fifth metatarsal bone) and the ability to bear weight. This assessment tool has a sensitivity of 96.4% to 99.6%, which makes it valuable in excluding ankle fractures.[11]
Evaluation
Patients with positive findings on the Ottawa ankle test should be referred for X-ray of the ankle. It is important to note that the prevalence of ankle fractures occur in less than 15% of cases.[11] Ultrasonography offers an advantage with dynamic imaging, and MRI can be implemented in cases with high suspicion for ligament injury. The accuracy of ultrasound is dependent on the technique and expertise of the clinician. It has a sensitivity and specificity of (92%) and (64 %) for detecting ligamentous injury.[8] Given high clinical suspicion for fracture, clinicians can implement MRI as this imaging modality has high sensitivity (93% to 96%) and specificity (100%).[12]
Following physical examination, lateral ankle injury is classified into three grades:
- Grade I injuries are due to the stretching of the ligament.
- Grade II is a moderate sprain.
- Grade III involves severe sprain full ligament lesions.
The increased grade indicates the severity of the injury, and as such, each grade assists clinicians with appropriate treatment, prognosis, and anticipated complications.[8]
Treatment / Management
Conservative management is often effective in treating CFL injuries. The progression of healing following initial injury has three distinct phases: inflammatory (1 to 10 days), proliferative (4 to 8 weeks), and remodeling phase (up to one year).[13] As such, each biological phase offers a unique therapeutic window for intervention.(A1)
During the initial inflammatory response, RICE (rest, ice, compression, and elevation) is implemented in the first 4 to 5 days. Immobilization with cast or boots can be applied in the first week to reduce swelling and pain, after which, brace or taping can be provided for a return to activity.[8] Immobilization during the proliferative stage is not encouraged since functional stress helps to promote remodeling. Ankle support with semi-rigid ankle brace is used for grade I to II injuries, while a cast immobilization followed by a semi-rigid orthosis can be used for grade III.[13] Over the counter, oral agents such as NSAIDs can be used to assist with pain.(A1)
Most lateral ankle injuries are managed non-operatively, while surgical interventions are allocated to patients with chronic instability.[8] Rigby et al. described two cases of isolated calcaneofibular ligament injury with one undergoing surgical intervention while another patient had conservative management with immobilization and physical therapy. Both patients had optimal outcomes. Surgical intervention must be analyzed on an individualized base, and in some patients, surgery can decrease recurrence rate and ankle instability; however, the overall clinical outcome is similar in conservative vs. surgical intervention.[8][13](A1)
Differential Diagnosis
CFL injury often involves the ATFL, and as such, isolated ATFL should be considered on the differential. Importantly, other differentials to consider are osteochondral injury, fibularis tendon injury, ankle fractures, Achilles rupture, and tendon dislocation. Lastly, injuries of the subtalar joint should be considered as CFL injuries can involve this joint.[14]
Prognosis
Return to play or work is an important discussion at the time of diagnosis, given that 25% of patients are expected to miss school or work.[15] Much more, patients may experience long term instability or pain. Four years after inciting injury, approximately 74% of patients continue to experience chronic symptoms of either pain, swelling, weakness, or instability. Additionally, 32% of patients have reported symptoms up to 7 years from the original injury.[15] A systematic review by Thompson et al. found that characteristics such as pain intensity, weight-bearing status, and range of motion to be an inconsistent prognostic factor due to bias with individual studies. However, these clinical findings can be used with caution to assist patients with anticipated recovery.
Complications
Lateral ankle injuries are not a sentinel event but have long term sequelae. Reinjury of the lateral compartment is a common occurrence in low-grade ankle sprains.[16] Patients can experience instability and pain which inhibits functional mobility. Chronic joint instability can progress to post-traumatic ankle joint osteoarthritis.[4]
Postoperative and Rehabilitation Care
Rehabilitation with early mobilization consisting of daily exercise programs is beneficial in functional recovery and mobilization. [17] A systematic review by Doherty et al. on exercise therapy for acute ankle sprain demonstrated unanimous support with self-reported functional improvement.[17] The average hours dedicated to rehabilitation varied from 3.5 to 21 hours. There are no reported protocols for exercise therapy standards; however, patients are tasked with working on strength and balance. [18] Early therapy within the first week of injury have been applied to diminished arthrogenic muscle inhibition from edema and pain. In effect, patients can achieve early reactivation of ankle musculature and functionality. [17] Ankle support with brace or taping can be provided for pain relief and secondary prevention during rehabilitation.
Deterrence and Patient Education
Calcaneofibular ligament injuries are rarely discussed as isolated cases in the literature. As such, much of our understanding is derived from lateral ankle injuries. The physical examination can assist clinicians in triaging patients for further evaluation and imaging modalities. Patients should be educated on the expected length of recovery and prognosis of the injury. Much more, patients should be advised to rehab their ankles as a premature return to activity appropriately may aggravate CFL injury. Weight-bearing status should be implemented base on individual cases with varying grades of injury.
Enhancing Healthcare Team Outcomes
Interdisciplinary efforts are essential to optimize care. Patients should be educated on disease progression and recovery stages. The recovery process occurs in three distinct phases, which can help guide intervention. Physical therapy, along with home exercise programs, may help promote functional recovery, and if warranted, surgical consultation for individualized cases can be pursued.
Media
(Click Image to Enlarge)
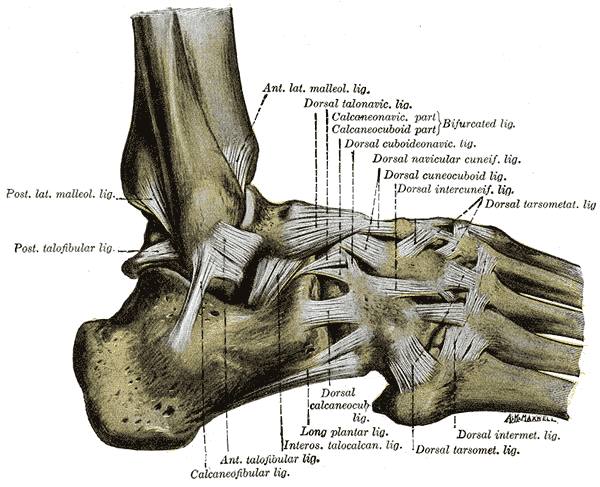
The Ligaments of the Foot; Lateral Aspect, Posterior lateral Malleolus Ligament, Posterior Talofibular Ligament, Anterior Lateral Malleolus Ligament, Dorsal Talonavicular Ligament, Calcaneonavicular Ligament, Calcaneofibular Ligament, Anterior Talofibular Ligament, Interosseous Talocalcaneal Ligament, Dorsal Tarsometatarsal Ligament, Dorsal Intermetatarsal Ligament, Dorsal Cuneocuboid Ligament, Dorsal Intercuneiform Ligament
Henry Vandyke Carter, Public domain, via Wikimedia Commons
References
Hunt KJ, Pereira H, Kelley J, Anderson N, Fuld R, Baldini T, Kumparatana P, D'Hooghe P. The Role of Calcaneofibular Ligament Injury in Ankle Instability: Implications for Surgical Management. The American journal of sports medicine. 2019 Feb:47(2):431-437. doi: 10.1177/0363546518815160. Epub 2018 Dec 20 [PubMed PMID: 30571138]
Fujii T, Luo ZP, Kitaoka HB, An KN. The manual stress test may not be sufficient to differentiate ankle ligament injuries. Clinical biomechanics (Bristol, Avon). 2000 Oct:15(8):619-23 [PubMed PMID: 10936435]
Rigby R, Cottom JM, Rozin R. Isolated calcaneofibular ligament injury: a report of two cases. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2015 May-Jun:54(3):487-9. doi: 10.1053/j.jfas.2014.08.017. Epub 2014 Oct 16 [PubMed PMID: 25441852]
Level 3 (low-level) evidenceDoherty C,Delahunt E,Caulfield B,Hertel J,Ryan J,Bleakley C, The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports medicine (Auckland, N.Z.). 2014 Jan; [PubMed PMID: 24105612]
Level 1 (high-level) evidenceDimmick S, Kennedy D, Daunt N. Evaluation of thickness and appearance of anterior talofibular and calcaneofibular ligaments in normal versus abnormal ankles with MRI. Journal of medical imaging and radiation oncology. 2008 Dec:52(6):559-63. doi: 10.1111/j.1440-1673.2008.02018.x. Epub [PubMed PMID: 19178629]
Struijs PA, Kerkhoffs GM. Ankle sprain. BMJ clinical evidence. 2010 May 13:2010():. pii: 1115. Epub 2010 May 13 [PubMed PMID: 21718566]
Level 1 (high-level) evidenceGolanó P, Vega J, de Leeuw PA, Malagelada F, Manzanares MC, Götzens V, van Dijk CN. Anatomy of the ankle ligaments: a pictorial essay. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2010 May:18(5):557-69. doi: 10.1007/s00167-010-1100-x. Epub 2010 Mar 23 [PubMed PMID: 20309522]
van den Bekerom MP, Kerkhoffs GM, McCollum GA, Calder JD, van Dijk CN. Management of acute lateral ankle ligament injury in the athlete. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2013 Jun:21(6):1390-5. doi: 10.1007/s00167-012-2252-7. Epub 2012 Oct 30 [PubMed PMID: 23108678]
Kovaleski JE, Norrell PM, Heitman RJ, Hollis JM, Pearsall AW. Knee and ankle position, anterior drawer laxity, and stiffness of the ankle complex. Journal of athletic training. 2008 May-Jun:43(3):242-8. doi: 10.4085/1062-6050-43.3.242. Epub [PubMed PMID: 18523573]
Hubbard TJ, Hicks-Little CA. Ankle ligament healing after an acute ankle sprain: an evidence-based approach. Journal of athletic training. 2008 Sep-Oct:43(5):523-9. doi: 10.4085/1062-6050-43.5.523. Epub [PubMed PMID: 18833315]
Level 1 (high-level) evidenceBachmann LM, Kolb E, Koller MT, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ (Clinical research ed.). 2003 Feb 22:326(7386):417 [PubMed PMID: 12595378]
Level 1 (high-level) evidenceVuurberg G, Hoorntje A, Wink LM, van der Doelen BFW, van den Bekerom MP, Dekker R, van Dijk CN, Krips R, Loogman MCM, Ridderikhof ML, Smithuis FF, Stufkens SAS, Verhagen EALM, de Bie RA, Kerkhoffs GMMJ. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. British journal of sports medicine. 2018 Aug:52(15):956. doi: 10.1136/bjsports-2017-098106. Epub 2018 Mar 7 [PubMed PMID: 29514819]
Petersen W, Rembitzki IV, Koppenburg AG, Ellermann A, Liebau C, Brüggemann GP, Best R. Treatment of acute ankle ligament injuries: a systematic review. Archives of orthopaedic and trauma surgery. 2013 Aug:133(8):1129-41. doi: 10.1007/s00402-013-1742-5. Epub 2013 May 28 [PubMed PMID: 23712708]
Level 1 (high-level) evidenceSugimoto K, Samoto N, Takaoka T, Takakura Y, Tamai S. Subtalar arthrography in acute injuries of the calcaneofibular ligament. The Journal of bone and joint surgery. British volume. 1998 Sep:80(5):785-90 [PubMed PMID: 9768887]
Thompson JY, Byrne C, Williams MA, Keene DJ, Schlussel MM, Lamb SE. Prognostic factors for recovery following acute lateral ankle ligament sprain: a systematic review. BMC musculoskeletal disorders. 2017 Oct 23:18(1):421. doi: 10.1186/s12891-017-1777-9. Epub 2017 Oct 23 [PubMed PMID: 29061135]
Level 1 (high-level) evidenceMalliaropoulos N, Ntessalen M, Papacostas E, Longo UG, Maffulli N. Reinjury after acute lateral ankle sprains in elite track and field athletes. The American journal of sports medicine. 2009 Sep:37(9):1755-61. doi: 10.1177/0363546509338107. Epub 2009 Jul 17 [PubMed PMID: 19617530]
Level 2 (mid-level) evidenceBleakley CM, O'Connor SR, Tully MA, Rocke LG, Macauley DC, Bradbury I, Keegan S, McDonough SM. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. BMJ (Clinical research ed.). 2010 May 10:340():c1964. doi: 10.1136/bmj.c1964. Epub 2010 May 10 [PubMed PMID: 20457737]
Level 1 (high-level) evidenceBleakley CM, Taylor JB, Dischiavi SL, Doherty C, Delahunt E. Rehabilitation Exercises Reduce Reinjury Post Ankle Sprain, But the Content and Parameters of an Optimal Exercise Program Have Yet to Be Established: A Systematic Review and Meta-analysis. Archives of physical medicine and rehabilitation. 2019 Jul:100(7):1367-1375. doi: 10.1016/j.apmr.2018.10.005. Epub 2018 Oct 26 [PubMed PMID: 30612980]
Level 1 (high-level) evidence