Introduction
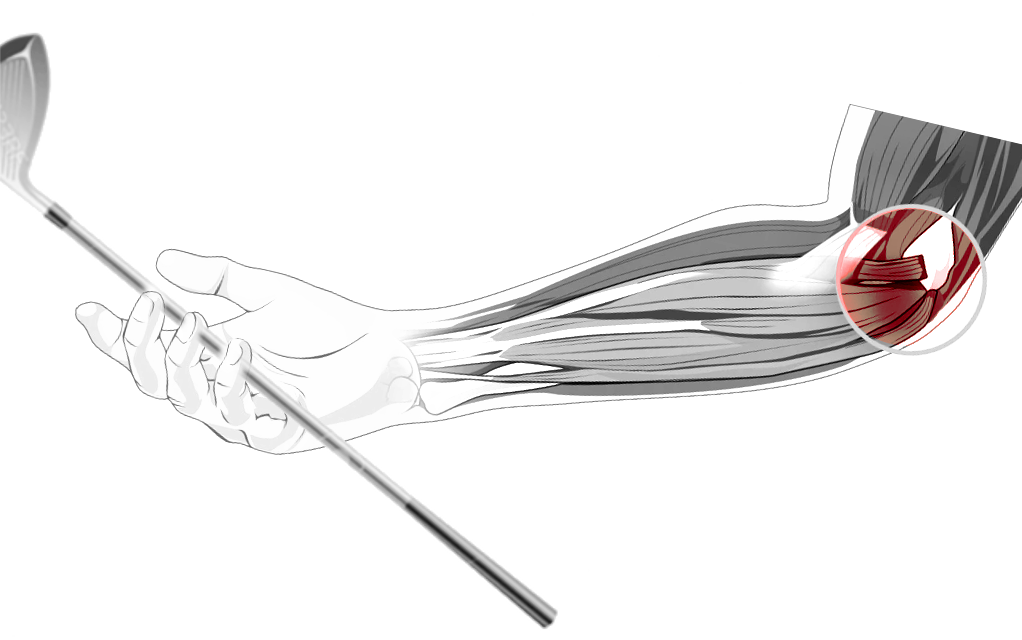
Tendinosis is a frequent cause of elbow pain both in athletes and the general population and is a result of overuse. Medial epicondylitis, commonly known as golfer’s elbow or little leaguer's elbow, represents tendinosis of the medial elbow at the origin of the flexor-pronator muscle group (see Images. Golfer's Elbow, Medial Elbow Anatomy). The tendons most commonly involved in medial epicondylitis include the pronator teres and flexor carpi radialis.
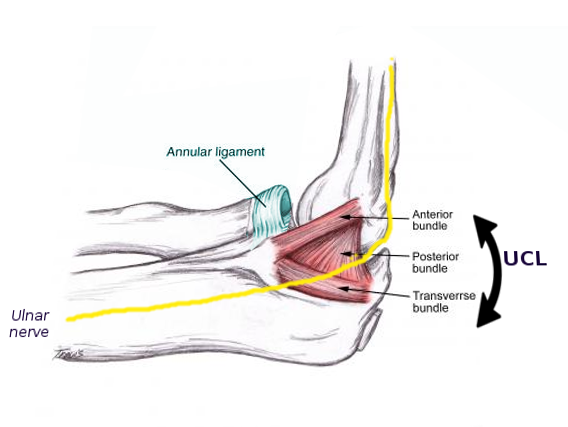
The medial epicondyle is on the distal humerus outside of the elbow joint capsule. It serves as the origin of the ulnar collateral ligament, pronator teres, and the common flexor tendon. The common flexor tendon includes the tendons of the flexor carpi radialis, flexor carpi ulnaris, flexor digitorum superficialis, and the palmaris longus. It provides stability against both valgus and flexion forces.[1] The ulnar collateral ligament is the primary restraint to valgus instability and is composed of anterior, posterior, and transverse bundles. The ulnar nerve runs posteriorly to the medial epicondyle in the ulnar groove and within the cubital tunnel.[2] See Image. Left Elbow Joint, Anterior and Internal Ligaments.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Overuse, specifically repetitive forearm pronation and wrist flexion, results in degenerative changes of the flexor and pronator tendons at their origin on the medial epicondyle. While uncommon, trauma or sudden eccentric contraction of the wrist flexors can result in an acute presentation of medial epicondylitis.[2]
Epidemiology
Research has found the prevalence of medial epicondylitis in working-aged adults to be between 0.4 to 0.6%.[3][4] A study examining medial epicondylitis in the United States military population reported an incidence rate of 0.81 per 1000 person-years.[5] While it may occur in all age groups, it is most prevalent in the fourth and fifth decades of life and most frequently involves the dominant arm. It affects men and women equally. Medial epicondylitis is less prevalent than lateral epicondylitis and represents less than 20% of all epicondylitis diagnoses.[6] Occupations requiring repetitive upper extremity movements, especially repetitive bending and straightening of the elbow, are associated with an increased risk of medial epicondylitis. Sports that require repetitive valgus stress and flexion at the elbow, such as golf, baseball, and bowling, increase the risk of the development of medial epicondylitis.[4]
Pathophysiology
Epicondylitis is an inaccurate term, as this condition does not represent acute inflammation of the bone. Instead, it is chronic tendinopathy of the flexor-pronator mass at its origin on the medial epicondyle. The condition occurs from recurrent microtrauma secondary to repetitive wrist flexion and pronation or repetitive valgus stress and flexion at the elbow. The flexor carpi radialis and pronator teres are the tendons most commonly involved.[6]
Histopathology
Histopathology reveals angiofibroblastic proliferation or disorganization of the collagen matrix with the development of neovessels.[2] Partial or full-thickness tears can occur as a part of the degenerative process.
History and Physical
Medial epicondylitis presents with a gradual onset of pain along the medial elbow that is worse with activity. Symptoms are often mild and intermittent but can be severe, resulting in significant pain and disability. The examination will reveal tenderness along the medial epicondyle and proximal pronator, and flexor tendons. Patients will have pain with resisted wrist flexion and pronation and passive terminal wrist extension. These provocative maneuvers should be performed with the elbow fully extended. In more chronic cases, patients may develop a loss of range of motion with wrist extension. There may be a decrease in grip strength.[6]
In cases of isolated medial epicondylitis, the ulnar collateral ligament and ulnar nerve should not be tender. A valgus stress test to assess the ulnar collateral ligament should be without instability or worsened pain. Ulnar neuritis is assessable by cubital tunnel compression testing and Tinel sign. A careful neurological examination, including 2-point discrimination testing of the fifth digit, is also necessary to assess the ulnar nerve. There is a high association of ulnar neuropathy with medial epicondylitis, occurring concomitantly in 60% of cases.[7]
Evaluation
Medial epicondylitis is a clinical diagnosis and does not require imaging. X-rays may be useful to evaluate recalcitrant cases and to rule out other pathology. MRI and ultrasound can visualize tendinosis but are not a requirement for diagnosis.
Treatment / Management
The initial management of epicondylitis is conservative. Non-operative treatment is successful in over 95% of patients. When treated with observation alone, symptoms persist between six months and two years.[8][9] First-line therapies include rest, ice, analgesics, bracing, and physical therapy. Relative rest and activity modification are key components to resolution and are required in both athletes and the general population for at least six weeks.(A1)
During the early stages, when acute inflammation may be present, ice, compression, and elevation may provide benefits. As the condition evolves into chronic tendinosis, these therapies are less likely to be effective. Non-steroidal anti-inflammatory drugs (NSAIDs) are a common choice for pain relief despite limited evidence on their effectiveness. A Cochrane review demonstrated low-quality evidence for short-term pain relief with topical NSAIDs, while results for oral NSAIDs have been inconclusive.[10](A1)
Bracing typically employs a counterforce strap applied just distal to the elbow joint to minimize the strain applied on the tendon origin at the medial epicondyle. Patients treated with a counterforce brace show improvement in pain and function compared to physical therapy at six weeks, but no difference after 26 weeks. Volar wrist splints are an option to immobilize the wrist and limit flexor activity. While wrist splints may result in a reduction in pain, they should be reserved for severe cases as they may result in a longer duration of symptoms.[11]
Physical therapy includes rehabilitation programs aimed at strengthening and flexibility. It also provides modalities to include soft tissue mobilization therapies. When used in isolation or as adjunctive therapy, eccentric exercises improve function and grip strength in addition to decreasing the pain.[12](A1)
Topical glyceryl trinitrate patches may stimulate collagen synthesis and play a role in healing tendons. When used along with physical therapy, patients demonstrated improvement in both pain and function, with 81% reporting no symptoms at six months.[13]
A medial epicondyle corticosteroid injection merits consideration in patients with symptoms refractory to other conservative measures or for those presenting with severe symptoms. Corticosteroid injections result in improved pain in the short term (less than 12 weeks).[14](A1)
Autologous blood and platelet-rich plasma (PRP) injections may result in improvements in the intermediate-term (12 to 26 weeks) compared to corticosteroids.[15] However, low-quality studies and conflicting results prevent routine recommendations for PRP or autologous blood injections.[16] (A1)
Both prolotherapy and botulinum toxin A injections result in reductions in pain compared to placebo but are not more effective than corticosteroid injections.[14](A1)
Surgical intervention is rarely necessary but is a consideration in cases with severe pain or marked dysfunction that is refractory to conservative treatments after six months or in cases persisting for longer than 12 months.
Differential Diagnosis
Medial epicondylitis requires differentiation from other causes of pain along the medial aspect of the elbow. This includes ulnar nerve entrapment, ulnar nerve subluxation, ulnar collateral ligament insufficiency, osteoarthritis, little league elbow, osteochondritis dissecans, and posteromedial elbow impingement.[17]
Treatment Planning
Indications for Medial Epicondyle Injection
Corticosteroids are the most common type of injection used for medial epicondylitis and are typically reserved for cases refractory to initial non-operative treatments after 6 to 12 weeks. Injections may also be used earlier in the course of the disease if symptoms are severe.
Contraindications
Contraindications to a medial epicondyle injection include cellulitis or other infection overlying or around the area, allergies to corticosteroid or anesthetic agents, local malignancy, skin breakdown, or fracture at the site of injection. In patients with diabetes mellitus, poorly controlled diabetes with hyperglycemia is an additional contraindication. There is no threshold for the number of injections that can be received; however, multiple injections are not a recommended approach, and instead, injections are usually limited to one.
Equipment
- 5 mL syringe
- 25 gauge, 1-inch needle
- 2 mL of anesthetic agent
- 1 mL corticosteroid (methylprednisolone, dexamethasone, and triamcinolone are common agents used. The provider may choose his or her preferred corticosteroid as there is no data to support one steroid type or dose.)[14]
- Gloves
- Chlorhexidine, alcohol pads, or other skin cleaning solution
- Topical anesthetic spray (optional)
Personnel
Physicians, physician assistants, or nurse practitioners trained in this procedure can perform the injection. A medical assistant, nurse, athletic trainer, or other assistants may be used to prep the patient.
Preparation
The provider will discuss the risks and benefits of the procedure and obtain written informed consent. A time-out to identify the patient, procedure, and site of the procedure should take place before the procedure.
Technique
The patient is placed in the supine position with the arm abducted and supinated. The point of maximal tenderness is palpated over the medial epicondyle and may get marked by indenting the skin with the tip of a pen or the capped needle. The injection site is then cleaned with chlorhexidine. An assistant may spray the area with topical anesthetic spray if desired. Using an aseptic technique, the needle is inserted directly down to the level of bone then withdrawn 1 to 2 mm before slowly injecting the anesthetic and corticosteroid solution. Ultrasound guidance has not demonstrated improved clinical outcomes compared to blinded techniques.[18][19]
A peppering technique that involves needle insertion with multiple small injections performed by retracting and repositioning without withdrawing the needle from the skin is also an option. Multiple passes are made until the clinician no longer feels crepitus while passing the needle. This minor fenestration of the tendon causes bleeding and inflammation, which may stimulate a healing response.
Toxicity and Adverse Effect Management
Corticosteroids have anti-inflammatory properties and can modify the body's immune response. The most feared complication of corticosteroid injections is an acute infection due to immunosuppression. With proper adherence to aseptic technique, this complication is exceedingly rare.
Common complications of the procedure include skin atrophy or skin hypopigmentation at the site of the procedure. Some patients may have a paradoxical increase in pain for the firth 24 hours after the injection. Increased pain that lasts for several days after the procedure is a rare complication known as a "steroid flare."
In patients with diabetes mellitus, it is imperative to note blood glucose levels before and after corticosteroid injection to prevent severe hyperglycemic episodes.
Prognosis
There is a paucity of data for outcomes of injections with medial epicondylitis, and much of the data used to guide treatment has been extrapolated from studies for lateral epicondylitis. Despite a lack of inflammation, corticosteroids are likely effective by providing relief of pain of neurogenic origin. Corticosteroids are effective in improving short-term pain relief. However, there is a high recurrence of pain and lack of benefit demonstrated at one year compared to observation and physical therapy. Therefore, corticosteroid injections should only be performed concurrently with other non-operative therapies.[20] Comparisons of a single injection of corticosteroid or a peppered injection of corticosteroid have shown more favorable results with the peppered technique.[21][22]
Complications
- Transient vasovagal reaction
- Bleeding
- Infection
- Acute worsening of pain
- Skin and fat atrophy
- Ulnar nerve damage
- Worsening of degeneration of the tendon
- Worsened pain and function after three months[23]
Deterrence and Patient Education
Patients should receive advice regarding relative rest following a medial epicondyle corticosteroid injection. Patients should understand the possibility of a steroid flare that can acutely worsen the pain; this is treatable with ice, acetaminophen, and NSAIDs.
Following an injection, patients should continue with activity modifications and other therapies until the pain subsides. A session on proper mechanics should take place before returning to work or sports. A slow functional progression of sport-specific exercises is required for a successful return to play. Typically, activity modifications and treatment are necessary for a total period of 6 to 12-weeks.
Enhancing Healthcare Team Outcomes
Medial epicondylitis is a chronic condition that can negatively impact function and cause significant pain. Initial treatment is conservative and requires multiple healthcare team members, including the clinical provider, nurses, medical assistants, athletic trainers, pharmacists, and physical therapists, to provide education, bracing, medications, and rehabilitation.
To improve healthcare outcomes, it is essential to have a functioning, cohesive interprofessional team, especially if a medial epicondyle injection is planned. The clinical providers should communicate the treatment plan with the specialty nurses, pharmacists, and physical therapists to achieve this goal. The pharmacists' role in these cases involves a thorough evaluation of the patient's medication profile and previous treatments to identify any possible interactions or adverse reactions. By communicating these findings with the medical team, the pharmacist can help decrease adverse reactions for these patients. The specialty nurse plays a crucial role in educating the patient in regards to post-procedure restrictions and monitoring, especially in patients with diabetes mellitus. Identifying patients most at risk for complications, the nurse can help focus the healthcare team's resources where they would be most effective. The physical therapist will need to alter the treatment plan once a medical epicondyle corticosteroid injection is given. The medical provider needs to communicate this with the physical therapist to ensure appropriate therapy is delivered. [Level 5]
Media
(Click Image to Enlarge)
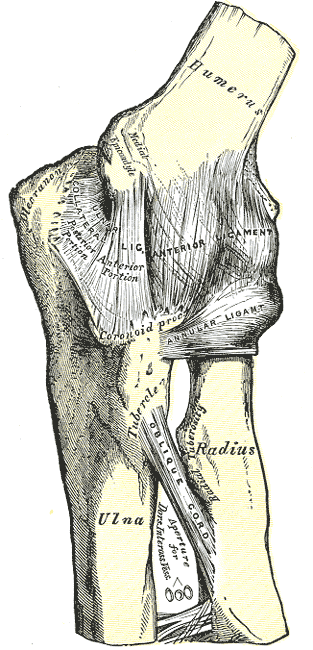
Left Elbow Joint, Anterior and Internal Ligaments. The illustration shows the left elbow joint and the anterior and internal ligaments.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Kheterpal AB, Bredella MA. Overuse Injuries of the Elbow. Radiologic clinics of North America. 2019 Sep:57(5):931-942. doi: 10.1016/j.rcl.2019.03.005. Epub 2019 May 6 [PubMed PMID: 31351542]
Pitzer ME, Seidenberg PH, Bader DA. Elbow tendinopathy. The Medical clinics of North America. 2014 Jul:98(4):833-49, xiii. doi: 10.1016/j.mcna.2014.04.002. Epub [PubMed PMID: 24994055]
Shiri R, Viikari-Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. American journal of epidemiology. 2006 Dec 1:164(11):1065-74 [PubMed PMID: 16968862]
Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Occupation and epicondylitis: a population-based study. Rheumatology (Oxford, England). 2012 Feb:51(2):305-10. doi: 10.1093/rheumatology/ker228. Epub 2011 Oct 22 [PubMed PMID: 22019808]
Level 2 (mid-level) evidenceWolf JM, Mountcastle S, Burks R, Sturdivant RX, Owens BD. Epidemiology of lateral and medial epicondylitis in a military population. Military medicine. 2010 May:175(5):336-9 [PubMed PMID: 20486505]
Taylor SA, Hannafin JA. Evaluation and management of elbow tendinopathy. Sports health. 2012 Sep:4(5):384-93 [PubMed PMID: 23016111]
Hariri S, McAdams TR. Nerve injuries about the elbow. Clinics in sports medicine. 2010 Oct:29(4):655-75. doi: 10.1016/j.csm.2010.06.001. Epub [PubMed PMID: 20883903]
Smidt N, Lewis M, VAN DER Windt DA, Hay EM, Bouter LM, Croft P. Lateral epicondylitis in general practice: course and prognostic indicators of outcome. The Journal of rheumatology. 2006 Oct:33(10):2053-59 [PubMed PMID: 16881095]
Struijs PA, Kerkhoffs GM, Assendelft WJ, Van Dijk CN. Conservative treatment of lateral epicondylitis: brace versus physical therapy or a combination of both-a randomized clinical trial. The American journal of sports medicine. 2004 Mar:32(2):462-9 [PubMed PMID: 14977675]
Level 1 (high-level) evidencePattanittum P, Turner T, Green S, Buchbinder R. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. The Cochrane database of systematic reviews. 2013 May 31:2013(5):CD003686. doi: 10.1002/14651858.CD003686.pub2. Epub 2013 May 31 [PubMed PMID: 23728646]
Level 1 (high-level) evidenceMeissner A, Vives MI, Román J, Meissner A. Is wrist splint more effective than forearm band for lateral epicondylitis? Medwave. 2017 Dec 28:17(9):e7124. doi: 10.5867/medwave.2017.09.7124. Epub 2017 Dec 28 [PubMed PMID: 29286358]
Cullinane FL, Boocock MG, Trevelyan FC. Is eccentric exercise an effective treatment for lateral epicondylitis? A systematic review. Clinical rehabilitation. 2014 Jan:28(1):3-19. doi: 10.1177/0269215513491974. Epub 2013 Jul 23 [PubMed PMID: 23881334]
Level 1 (high-level) evidenceMcCallum SD, Paoloni JA, Murrell GA. Five-year prospective comparison study of topical glyceryl trinitrate treatment of chronic lateral epicondylosis at the elbow. British journal of sports medicine. 2011 Apr:45(5):416-20. doi: 10.1136/bjsm.2009.061002. Epub 2009 Jun 23 [PubMed PMID: 19553221]
Sims SE, Miller K, Elfar JC, Hammert WC. Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials. Hand (New York, N.Y.). 2014 Dec:9(4):419-46. doi: 10.1007/s11552-014-9642-x. Epub [PubMed PMID: 25414603]
Level 1 (high-level) evidenceHouck DA, Kraeutler MJ, Thornton LB, McCarty EC, Bravman JT. Treatment of Lateral Epicondylitis With Autologous Blood, Platelet-Rich Plasma, or Corticosteroid Injections: A Systematic Review of Overlapping Meta-analyses. Orthopaedic journal of sports medicine. 2019 Mar:7(3):2325967119831052. doi: 10.1177/2325967119831052. Epub 2019 Mar 14 [PubMed PMID: 30899764]
Level 1 (high-level) evidenceAhmad Z, Brooks R, Kang SN, Weaver H, Nunney I, Tytherleigh-Strong G, Rushton N. The effect of platelet-rich plasma on clinical outcomes in lateral epicondylitis. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2013 Nov:29(11):1851-62. doi: 10.1016/j.arthro.2013.07.272. Epub 2013 Sep 21 [PubMed PMID: 24060428]
Level 1 (high-level) evidenceDonaldson O, Vannet N, Gosens T, Kulkarni R. Tendinopathies Around the Elbow Part 2: Medial Elbow, Distal Biceps and Triceps Tendinopathies. Shoulder & elbow. 2014 Jan:6(1):47-56. doi: 10.1111/sae.12022. Epub 2013 Jun 10 [PubMed PMID: 27582910]
Gulabi D, Uysal MA, Akça A, Colak I, Çeçen GS, Gumustas S. USG-guided injection of corticosteroid for lateral epicondylitis does not improve clinical outcomes: a prospective randomised study. Archives of orthopaedic and trauma surgery. 2017 May:137(5):601-606. doi: 10.1007/s00402-017-2657-3. Epub 2017 Mar 4 [PubMed PMID: 28258434]
Level 2 (mid-level) evidenceMalahias MA, Kaseta MK, Kazas ST, Megaloikonomos PD, Mavrogenis AF, Babis GC. Image-guided versus palpation-guided injections for the treatment of chronic lateral epicondylopathy: a randomized controlled clinical trial. Handchirurgie, Mikrochirurgie, plastische Chirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie : Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse : Organ der V.... 2018 Sep:50(5):348-352. doi: 10.1055/a-0732-5556. Epub 2018 Nov 7 [PubMed PMID: 30404123]
Level 1 (high-level) evidenceCiccotti MC, Schwartz MA, Ciccotti MG. Diagnosis and treatment of medial epicondylitis of the elbow. Clinics in sports medicine. 2004 Oct:23(4):693-705, xi [PubMed PMID: 15474230]
Dogramaci Y, Kalaci A, Savaş N, Duman IG, Yanat AN. Treatment of lateral epicondilitis using three different local injection modalities: a randomized prospective clinical trial. Archives of orthopaedic and trauma surgery. 2009 Oct:129(10):1409-14. doi: 10.1007/s00402-009-0832-x. Epub 2009 Feb 14 [PubMed PMID: 19219442]
Level 1 (high-level) evidenceOkçu G, Erkan S, Sentürk M, Ozalp RT, Yercan HS. Evaluation of injection techniques in the treatment of lateral epicondylitis: a prospective randomized clinical trial. Acta orthopaedica et traumatologica turcica. 2012:46(1):26-9 [PubMed PMID: 22441448]
Level 1 (high-level) evidenceOlaussen M, Holmedal O, Lindbaek M, Brage S, Solvang H. Treating lateral epicondylitis with corticosteroid injections or non-electrotherapeutical physiotherapy: a systematic review. BMJ open. 2013 Oct 29:3(10):e003564. doi: 10.1136/bmjopen-2013-003564. Epub 2013 Oct 29 [PubMed PMID: 24171937]
Level 1 (high-level) evidence