Introduction
Tonsil cancer is the most common form of oropharyngeal malignancy, and its incidence is sharply rising due to the increasing prevalence of human papillomavirus (HPV)-induced cancers. The presence of HPV can dramatically alter the prognosis of tonsillar cancer, and there have recently been significant changes made to the WHO classification and TNM staging to reflect this. Tonsil cancer can be managed by both surgical and oncological approaches, although the optimal treatment regimen remains an area of ongoing research.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Traditionally, oropharyngeal and tonsil cancers were attributed to smoking and alcohol misuse, with the former remaining an independent indicator of poor prognosis. In more recent years; however, there has been a sharp increase in the number of cases occurring secondary to HPV, with up to 93% of new oropharyngeal cancers in Western Europe showing HPV positivity.[1] Additionally, there is a growing body of evidence to suggest having a spouse with HPV-related cancer can result in a slight increase in the likelihood of developing oropharyngeal and anogenital cancers.[2]
Epidemiology
Large epidemiological studies have shown tonsils are the most common site of oropharyngeal cancer, compromising 23.1% of all malignancies in this anatomical region, with an overall incidence rate of 8.4 cases per 100,000.[3] Of concern, the rate of tonsil and oropharyngeal cancers has increased dramatically in the last 40 years. This significant rise has been attributed to the "viral epidemic" of HPV, with western countries seeing an increase in the proportion of HPV-associated cancers from 42.5% before 2000 to 72.2% between 2005 and 2009. Conversely, was not a significant increase in the rate of non-HPV oropharyngeal cancers within the same period.[4]
Histopathology
HPV is a double-stranded DNA virus implicated in a host of carcinomas throughout the body. HPV 16 has the greatest association with oropharyngeal cancers, with other oncogenic strains including HPV 18 being less common[5]. p16 is a tumor-suppressor protein that is overexpressed in HPV-positive tumors and is well established as a useful surrogate marker of HPV in tonsil cancer.[6]
The fourth edition of the World Health Organization's Classification of Head and Neck Tumors has made a number of changes to reflect our current understanding of the disease. Oral and oropharyngeal cancers are now separate clinical entities, due to the presence of lymphoepithelial tissues within areas such as the tonsils. Most tonsil cancers are squamous cell carcinomas (SCC). However, the WHO classification now subdivides this into two distinct morphological groups; HPV positive and HPV negative. HPV positive SCCs arise from the deep lymphoid tissue of the tonsillar crypts and have a non-keratinising morphology. HPV negative SCC develops from the oropharyngeal/tonsil surface epithelium and is associated with keratinizing dysplasia.[7]
History and Physical
Tonsillar cancers can have a highly variable clinical history. Patient's may have complaints of a sore throat, unilateral otalgia, or sensation of a mass in the throat, with trismus being a concerning sign of local invasion. Others may be asymptomatic and referred as an incidental finding of asymmetrical tonsils. The tonsil's rich lymphatic supply means many tumors present as an occult lesion with enlarged cervical nodes, in particular within the jugulodigastric region. It is vital to ask the patient about red flag symptoms including weight loss, odynophagia, dysphagia, and persistent hoarseness. Thorough past medical history and discussion of etiological factors including smoking, increased alcohol intake and risk behaviors (e.g., intravenous drug use) may help elicit an underlying cause.
HPV-positive tumors will typically present in younger non-smoking patients of either gender, while HPV-negative tumors will present in older male smokers with more co-morbidities, and thus have a poorer prognosis overall.
Patients require a full ear, nose, and throat examination by an experienced otolaryngologist, including palpation of the neck for cervical lymphadenopathy and close inspection of the oropharynx. Particular attention should be paid to the tonsil beds as primary cancers can be missed within the tonsil crypts. Flexible nasal endoscopy should be performed in all patients for a thorough assessment of the oropharynx including inspection of the tonsils, tongue base, vallecula, and lateral pharyngeal wall for signs of local invasion.
Evaluation
Imaging
All cases of tonsillar cancer will need through pre-treatment cross-sectional imaging, with contrast-enhanced MRI providing the best quality soft tissue delineation of the primary disease and local spread.[8] CT can also assess the primary disease although an artifact from adjacent dental treatments often limits this. CT is currently the imaging modality of choice for staging all head and neck cancers and should be performed from skull base to diaphragm to look for associated nodal and pulmonary disease.[9]
PET-CT can also be used in tonsil cancer as a means to help with diagnosis and staging in difficult to detect cancers[10] and in post-treatment surveillance.[11]. However, it is limited by its false-positive findings, frequently showing uptake in contralateral tonsils,[12] tongue base and Waldeyer's ring[10] without the presence of malignancy.
Endoscopy
It is strongly recommended all suspected tonsillar cancers undergo an examination under anesthesia and panendoscopy.[13] This can facilitate close assessment and biopsy of the disease, planning of surgical interventions, and exclusion of secondary malignancies within the upper airway and esophagus. FNA biopsies have been used in those who are unfit for surgery; however, the reliability of HPV testing in cytology samples has been questioned.[14]
Treatment / Management
Surgical Management
Early tonsil cancer is preferably managed with single modality treatment, with transoral robotic surgery (TORS) and transoral laser microsurgery (TLM) having comparable oncological outcomes.[15] TORs is growing in popularity and has been shown to have reduced operating time, shorter hospital stay, and improved swallowing recovery compared to open techniques[16]; although, persistent severe dysphagia can occur post-operatively.[17] TLM is less widely adopted and involves removal of the tumor in several pieces, making a histological examination of margins difficult.[13] Regardless of the method of surgical intervention, it is advised to remove both tonsils at time of surgery due to a small rate of bilateral synchronous tonsillar cancers.[18](B2)
In more advanced disease, TLM or TORS can still be offered for early T3 tumors; however, this is often not possible for T4 malignancies. Most of these cases will instead undergo chemoradiotherapy, as a surgical intervention will usually require a mandibulotomy and extensive surgical reconstruction resulting in poor post-operative functional outcomes.[13]
Given the high rate of nodal disease in both early and advanced tonsillar cancer, it is recommended that most cases undergoing surgical intervention should also have an elective level II to IV neck dissection.[19](B3)
Oncological Management
Primary radiotherapy for early tonsillar cancer has been shown to have good oncological outcomes and overall survival. Unilateral radiotherapy to levels II to IV can be used in non-lateralized cancers with a low rate of contralateral nodal recurrence and improved rates of radiation toxicity.[20] It is advised to treat those with contralateral nodes with bilateral radiotherapy.[13]
A previous Cochrane review has established chemoradiotherapy as the management of choice for advanced tonsil and oropharyngeal cancers.[21] This avoids the need for extensive surgery which carries significant long-term morbidity and often requires post-operative chemoradiotherapy. Radiotherapy in addition to concurrent platinum-based cisplatin chemotherapy is the most widely used regime, with the monoclonal antibody cetuximab being used as an equally effective alternative in cases where cisplatin is contraindicated (renal impairment and hearing loss).[22](A1)
Differential Diagnosis
The histological differential diagnosis of suspected tonsillar cancer includes;
Staging
Tonsil malignancy is staged as oropharyngeal cancer according to the AJCC TNM classification of malignant tumors. The 2016 eight edition splits oropharyngeal cancer into p16 positive and negative cancers to reflect the current understanding of the influence of HPV and p16 on the prognosis and management.[28] This marks a dramatic change from previous editions of the manual, and can significantly alter the final staging of the malignancy.
T Classification Oropharyngeal Cancers
- T1: Tumor 2 cm or less
- T2: Tumor more than 2 cm but less than 4 cm
- T3: Tumor greater than 4 cm or extension into the lingual surface of epiglottis
- p16 negative tumors
- T4a: Tumor invades larynx, deep/extrinsic muscle of tongue, medial pterygoid, hard palate, or mandible
- T4b: Tumor invades lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, skull base; or encases carotid artery
- p16 positive tumors
- T4: Larynx, deep/extrinsic muscle of tongue, medial pterygoid, hard palate, mandible, lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, skull base; or encases carotid artery
N Classification p16 Negative
- N0: No regional lymph node metastasis
- N1: Single ipsilateral node less than 3 cm
- N2
- N2a: Single ipsilateral node greater than 3 cm but less than 6cm
- N2b: Multiple ipsilateral nodes less than 6 cm
- N2c: Bilateral and contralateral nodes less than 6cm
- N3
- N3a: Single node greater than 6 cm
- N3b: Single or multiple nodes with extra-capsular spread
N Classification p16 Positive
- N0: No regional lymph node metastasis
- N1: Unilateral nodes all less than 6 cm
- N2: Contralateral or bilateral nodes all less than 6 cm
- N3: Metastasis greater than 6 cm
M Classification
- M0: No distant metastasis
- M1: Distant metastasis
Prognosis
Prognosis of tonsil cancer is dependent on the HPV status of the tumor, with HPV positive tumors showing a 5-year overall survival of 71% compared to 46% in HPV negative disease in one study.[29] However, this survival benefit can be negated by the presence of smoking, with mortality rates being significantly higher in HPV-positive smokers compared to non-smokers.[30] Other factors including low volume tumors, lack of nodal disease, young age, low comorbid status, and presence of tumor invading lymphocytes are thought to influence prognosis in oropharyngeal tumors positively.[31] There are no studies directly comparing survival outcomes in tonsil cancers managed with a single modality surgical or oncological management.
Complications
Untreated tonsillar cancer will result in gradual growth and invasion of local structures. Invasion of the lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, skull base and encasement around the carotid is suggestive of unresectable T4b disease in p16 negative cancers. Moreover, invasion of the skull base and vertebral tissues can interfere with emerging nerves, resulting in Horner's syndrome and palsies of the brachial plexus and phrenic nerve. Encasement of the carotid artery can cause a life-threatening carotid blow-out.
The management options of tonsil cancer can also carry significant complications. TORS can result in significant pain and dysphagia postoperatively, particularly in advanced disease. Radiotherapy frequently causes mucositis, xerostomia, and skin reactions, which can also have a significant impact on swallowing.[32] These effects can be amplified in those who undergo TORS resection with post-operative chemo-radiotherapy, who have reported significantly worse swallowing and quality of life outcomes compared to those undergoing single modality treatments.[33]
Consultations
- Otolaryngologists
- Oncologists
- Radiologists
- Plastic/maxillofacial surgeons
- Restorative dentists
- Clinical nurse specialists
- Dieticians
- Speech and language therapists
- Palliative care
Deterrence and Patient Education
Advice on alcohol and smoking cessation should be offered to all patients given their etiological and prognostic influence. HPV vaccination is a controversial topic within the lay media, and although numerous studies have established their effectiveness in the prevention of gynecological malignancies, there is little evidence supporting their use in tonsillar cancers. Moreover, the lack of a pre-malignant stage (as seen in cervical CIS) and differences in HPV epidemiology between cancers could present barriers to its effectiveness.[34] Nevertheless, vaccination of females and males in several countries including the United Kindom, United States, Canada, and Australia is hoped to reduce the rates of oropharyngeal cancers long term.
Enhancing Healthcare Team Outcomes
Management of tonsil cancer requires an interprofessional approach. The initial investigation occurs within the otolaryngology outpatient setting, with the involvement of radiology and pathology departments proving vital for definitive diagnosis and clinical staging. Otolaryngologists and oncologists will ultimately manage the disease with a specialist interest in head and neck cancer; however, support is required from speech and language therapists, nurse specialists, and dietician teams to manage the resultant swallowing, emotional, and nutritional issues. For those undergoing radiotherapy, a review by restorative dentistry is necessary to avoid debilitating osteoradionecrosis.
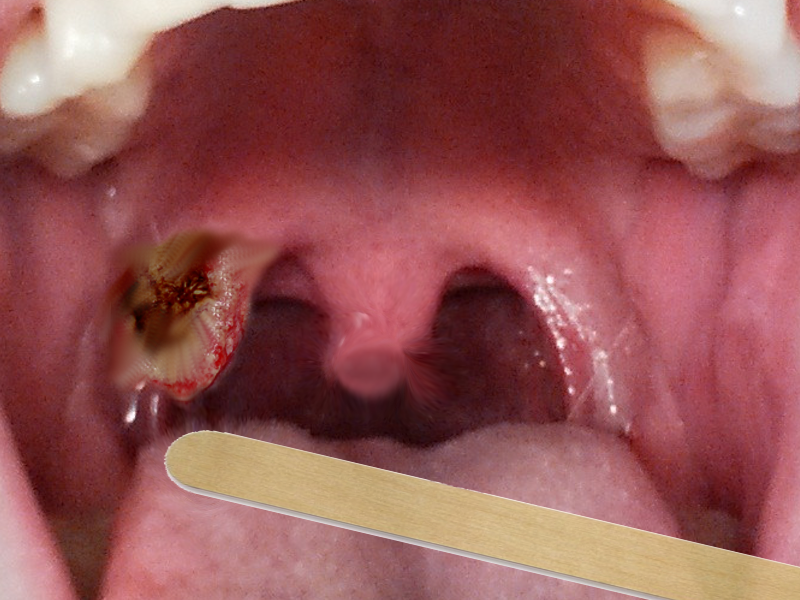
Media
References
Näsman A, Attner P, Hammarstedt L, Du J, Eriksson M, Giraud G, Ahrlund-Richter S, Marklund L, Romanitan M, Lindquist D, Ramqvist T, Lindholm J, Sparén P, Ye W, Dahlstrand H, Munck-Wikland E, Dalianis T. Incidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma? International journal of cancer. 2009 Jul 15:125(2):362-6. doi: 10.1002/ijc.24339. Epub [PubMed PMID: 19330833]
Mirghani H, Sturgis EM, Aupérin A, Monsonego J, Blanchard P. Is there an increased risk of cancer among spouses of patients with an HPV-related cancer: A systematic review. Oral oncology. 2017 Apr:67():138-145. doi: 10.1016/j.oraloncology.2017.02.024. Epub 2017 Feb 28 [PubMed PMID: 28351568]
Level 1 (high-level) evidenceWeatherspoon DJ, Chattopadhyay A, Boroumand S, Garcia I. Oral cavity and oropharyngeal cancer incidence trends and disparities in the United States: 2000-2010. Cancer epidemiology. 2015 Aug:39(4):497-504. doi: 10.1016/j.canep.2015.04.007. Epub 2015 May 11 [PubMed PMID: 25976107]
Mehanna H, Beech T, Nicholson T, El-Hariry I, McConkey C, Paleri V, Roberts S. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer--systematic review and meta-analysis of trends by time and region. Head & neck. 2013 May:35(5):747-55. doi: 10.1002/hed.22015. Epub 2012 Jan 20 [PubMed PMID: 22267298]
Level 1 (high-level) evidenceKreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2005 Feb:14(2):467-75 [PubMed PMID: 15734974]
Level 1 (high-level) evidenceHassani S, Castillo A, Ohori J, Higashi M, Kurono Y, Akiba S, Koriyama C. Molecular Pathogenesis of Human Papillomavirus Type 16 in Tonsillar Squamous Cell Carcinoma. Anticancer research. 2015 Dec:35(12):6633-8 [PubMed PMID: 26637879]
Westra WH, Lewis JS Jr. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Oropharynx. Head and neck pathology. 2017 Mar:11(1):41-47. doi: 10.1007/s12105-017-0793-2. Epub 2017 Feb 28 [PubMed PMID: 28247229]
Lewis-Jones H, Colley S, Gibson D. Imaging in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. The Journal of laryngology and otology. 2016 May:130(S2):S28-S31 [PubMed PMID: 27841111]
Loh KS, Brown DH, Baker JT, Gilbert RW, Gullane PJ, Irish JC. A rational approach to pulmonary screening in newly diagnosed head and neck cancer. Head & neck. 2005 Nov:27(11):990-4 [PubMed PMID: 16136584]
Level 2 (mid-level) evidenceWong WL, Sonoda LI, Gharpurhy A, Gollub F, Wellsted D, Goodchild K, Lemon C, Farrell R, Saunders M. 18F-fluorodeoxyglucose positron emission tomography/computed tomography in the assessment of occult primary head and neck cancers--an audit and review of published studies. Clinical oncology (Royal College of Radiologists (Great Britain)). 2012 Apr:24(3):190-5. doi: 10.1016/j.clon.2011.11.001. Epub 2011 Dec 17 [PubMed PMID: 22183080]
Level 2 (mid-level) evidenceMehanna H, McConkey CC, Rahman JK, Wong WL, Smith AF, Nutting C, Hartley AG, Hall P, Hulme C, Patel DK, Zeidler SV, Robinson M, Sanghera B, Fresco L, Dunn JA. PET-NECK: a multicentre randomised Phase III non-inferiority trial comparing a positron emission tomography-computerised tomography-guided watch-and-wait policy with planned neck dissection in the management of locally advanced (N2/N3) nodal metastases in patients with squamous cell head and neck cancer. Health technology assessment (Winchester, England). 2017 Apr:21(17):1-122. doi: 10.3310/hta21170. Epub [PubMed PMID: 28409743]
Level 1 (high-level) evidenceHirshoren N, Olayos E, Callahan J, Lau E. PET/CT findings within the contralateral tonsil following unilateral tonsillectomy. The Laryngoscope. 2016 Nov:126(11):2480-2483. doi: 10.1002/lary.26023. Epub 2016 Apr 26 [PubMed PMID: 27114188]
Mehanna H, Evans M, Beasley M, Chatterjee S, Dilkes M, Homer J, O'Hara J, Robinson M, Shaw R, Sloan P. Oropharyngeal cancer: United Kingdom National Multidisciplinary Guidelines. The Journal of laryngology and otology. 2016 May:130(S2):S90-S96 [PubMed PMID: 27841123]
Takes RP, Kaanders JH, van Herpen CM, Merkx MA, Slootweg PJ, Melchers WJ. Human papillomavirus detection in fine needle aspiration cytology of lymph node metastasis of head and neck squamous cell cancer. Journal of clinical virology : the official publication of the Pan American Society for Clinical Virology. 2016 Dec:85():22-26. doi: 10.1016/j.jcv.2016.10.008. Epub 2016 Oct 27 [PubMed PMID: 27816020]
Moore EJ, Hinni ML. Critical review: transoral laser microsurgery and robotic-assisted surgery for oropharynx cancer including human papillomavirus-related cancer. International journal of radiation oncology, biology, physics. 2013 Apr 1:85(5):1163-7. doi: 10.1016/j.ijrobp.2012.08.033. Epub 2012 Nov 20 [PubMed PMID: 23182390]
Lee SY, Park YM, Byeon HK, Choi EC, Kim SH. Comparison of oncologic and functional outcomes after transoral robotic lateral oropharyngectomy versus conventional surgery for T1 to T3 tonsillar cancer. Head & neck. 2014 Aug:36(8):1138-45. doi: 10.1002/hed.23424. Epub 2013 Oct 17 [PubMed PMID: 23836492]
Patel AB, Hinni ML, Pollei TR, Hayden RE, Moore EJ. Severe prolonged dysphagia following transoral resection of bilateral synchronous tonsillar carcinoma. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2015 Nov:272(11):3585-91. doi: 10.1007/s00405-015-3540-x. Epub 2015 Feb 8 [PubMed PMID: 25663269]
Level 3 (low-level) evidenceRokkjaer MS, Klug TE. Prevalence of synchronous bilateral tonsil squamous cell carcinoma: A retrospective study. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2018 Feb:43(1):1-6. doi: 10.1111/coa.12981. Epub 2017 Sep 25 [PubMed PMID: 28891195]
Level 2 (mid-level) evidenceGrégoire V, Ang K, Budach W, Grau C, Hamoir M, Langendijk JA, Lee A, Le QT, Maingon P, Nutting C, O'Sullivan B, Porceddu SV, Lengele B. Delineation of the neck node levels for head and neck tumors: a 2013 update. DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiotherapy and oncology : journal of the European Society for Therapeutic Radiology and Oncology. 2014 Jan:110(1):172-81. doi: 10.1016/j.radonc.2013.10.010. Epub 2013 Oct 31 [PubMed PMID: 24183870]
Level 3 (low-level) evidenceCharbonneau N, Gélinas M, del Vecchio P, Guertin L, Larochelle D, Tabet JC, Soulières D, Charpentier D, Nguyen-Tân PF. Primary radiotherapy for tonsillar carcinoma: a good alternative to a surgical approach. The Journal of otolaryngology. 2006 Aug:35(4):227-34 [PubMed PMID: 17176797]
Chan KK, Glenny AM, Weldon JC, Furness S, Worthington HV, Wakeford H. Interventions for the treatment of oral and oropharyngeal cancers: targeted therapy and immunotherapy. The Cochrane database of systematic reviews. 2015 Dec 1:2015(12):CD010341. doi: 10.1002/14651858.CD010341.pub2. Epub 2015 Dec 1 [PubMed PMID: 26625332]
Level 1 (high-level) evidenceOnita B, Lester D R T, Iman A A, Jergin C, Shawn I. Comparison of high-dose Cisplatin-based chemoradiotherapy and Cetuximab-based bioradiotherapy for p16-positive oropharyngeal squamous cell carcinoma in the context of revised HPV-based staging. Reports of practical oncology and radiotherapy : journal of Greatpoland Cancer Center in Poznan and Polish Society of Radiation Oncology. 2018 Sep-Oct:23(5):451-457. doi: 10.1016/j.rpor.2018.08.007. Epub 2018 Sep 7 [PubMed PMID: 30210266]
Sehdev A, Zhao Y, Singh AK, Sharma N. Primary small cell carcinoma of the tonsil: a case report and review of the literature. Case reports in oncology. 2012 Sep:5(3):537-41. doi: 10.1159/000343676. Epub 2012 Oct 5 [PubMed PMID: 23139668]
Level 3 (low-level) evidenceVasileiadis I, Sofopoulos M, Arnogiannaki N, Georgopoulos S. A Merkel-cell carcinoma metastatic to the tonsil: a case report and review of the literature. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2013 Oct:71(10):1812.e1-6. doi: 10.1016/j.joms.2013.06.196. Epub 2013 Aug 1 [PubMed PMID: 23911145]
Level 3 (low-level) evidenceMassaccesi M, Morganti AG, Serafini G, Di Lallo A, Deodato F, Picardi V, Scambia G. Late tonsil metastases from renal cell cancer: a case report. Tumori. 2009 Jul-Aug:95(4):521-4 [PubMed PMID: 19856668]
Level 3 (low-level) evidenceWang H, Chen P. Palatine tonsillar metastasis of rectal adenocarcinoma: a case report and literature review. World journal of surgical oncology. 2013 May 25:11():114. doi: 10.1186/1477-7819-11-114. Epub 2013 May 25 [PubMed PMID: 23705669]
Level 3 (low-level) evidenceUnsal M, Kutlar G, Sullu Y, Yurtlu S. Tonsillar metastasis of small cell lung carcinoma. The clinical respiratory journal. 2016 Nov:10(6):681-683. doi: 10.1111/crj.12275. Epub 2015 Mar 3 [PubMed PMID: 25620524]
Level 3 (low-level) evidenceLydiatt WM, Patel SG, O'Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, Loomis AM, Shah JP. Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA: a cancer journal for clinicians. 2017 Mar:67(2):122-137. doi: 10.3322/caac.21389. Epub 2017 Jan 27 [PubMed PMID: 28128848]
Charfi L, Jouffroy T, de Cremoux P, Le Peltier N, Thioux M, Fréneaux P, Point D, Girod A, Rodriguez J, Sastre-Garau X. Two types of squamous cell carcinoma of the palatine tonsil characterized by distinct etiology, molecular features and outcome. Cancer letters. 2008 Feb 18:260(1-2):72-8 [PubMed PMID: 18060686]
Level 3 (low-level) evidenceGillison ML, Zhang Q, Jordan R, Xiao W, Westra WH, Trotti A, Spencer S, Harris J, Chung CH, Ang KK. Tobacco smoking and increased risk of death and progression for patients with p16-positive and p16-negative oropharyngeal cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012 Jun 10:30(17):2102-11. doi: 10.1200/JCO.2011.38.4099. Epub 2012 May 7 [PubMed PMID: 22565003]
Ward MJ, Thirdborough SM, Mellows T, Riley C, Harris S, Suchak K, Webb A, Hampton C, Patel NN, Randall CJ, Cox HJ, Jogai S, Primrose J, Piper K, Ottensmeier CH, King EV, Thomas GJ. Tumour-infiltrating lymphocytes predict for outcome in HPV-positive oropharyngeal cancer. British journal of cancer. 2014 Jan 21:110(2):489-500. doi: 10.1038/bjc.2013.639. Epub 2013 Oct 29 [PubMed PMID: 24169344]
Level 2 (mid-level) evidenceRusthoven KE, Raben D, Ballonoff A, Kane M, Song JI, Chen C. Effect of radiation techniques in treatment of oropharynx cancer. The Laryngoscope. 2008 Apr:118(4):635-9. doi: 10.1097/MLG.0b013e31815fdf0e. Epub [PubMed PMID: 18176348]
Level 2 (mid-level) evidenceAchim V, Bolognone RK, Palmer AD, Graville DJ, Light TJ, Li R, Gross N, Andersen PE, Clayburgh D. Long-term Functional and Quality-of-Life Outcomes After Transoral Robotic Surgery in Patients With Oropharyngeal Cancer. JAMA otolaryngology-- head & neck surgery. 2018 Jan 1:144(1):18-27. doi: 10.1001/jamaoto.2017.1790. Epub [PubMed PMID: 29075740]
Level 2 (mid-level) evidenceGuo T, Eisele DW, Fakhry C. The potential impact of prophylactic human papillomavirus vaccination on oropharyngeal cancer. Cancer. 2016 Aug 1:122(15):2313-23. doi: 10.1002/cncr.29992. Epub 2016 May 6 [PubMed PMID: 27152637]