Introduction
The uterus is a hollow, pear-shaped organ responsible for various functions, such as gestation (pregnancy), menstruation, and labor and delivery. On a coronal cut section, its cavity has an inverted triangle shape. Sometimes, the development in utero may be incomplete; this is called a Mullerian anomaly and can lead to many variants, ranging from a uterine septum to uterine didelphys (double uterus). Anatomically, the uterus is located in the female pelvis immediately posterior to the bladder and anterior to the rectum. The female uterus subdivides into four main anatomic segments (from superior to inferior): the fundus; a broad curved area in which Fallopian tubes connect to the uterus, the corpus (body); the main part of a uterus, and it starts directly below the level of fallopian tubes and continues downward, isthmus; a lower neck region of the uterus, and cervix; which extends downwards from the isthmus and opens in the vagina (see Image. The Uterus).[1][2][3]
Several ligaments support the uterus, including the utero-ovarian, round, broad, cardinal, and uterosacral ligaments. The pelvic diaphragm, urogenital diaphragm, and perineal body further support it (inferiorly). The uterus may naturally lie in different positions, such as anteverted/retroverted, anteflexed/retroflexed, or midline, and it may be rotated (especially during pregnancy). In 50% of women, the uterus most commonly lies in an anteflexed and anteverted position.
When the uterus is in a retroverted/retroflexed or "tipped" position, it may cause pelvic pain, dyspareunia, minor incontinence, fertility difficulty, and difficulty inserting tampons. In pregnancy, this may lead to uterine incarceration.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The uterus nurtures the fertilized ovum, which passes through the fallopian tube. The ovum then implants into the endometrium, where it receives nourishment from blood vessels exclusively developed for this purpose. As the embryo grows and matures, the uterus expands to accommodate the developing fetus. During normal labor, the uterus contracts as the cervix dilates, resulting in the delivery of the infant.
Embryology
The uterus's early development is quite complex. At about eight weeks of gestation, primordia for female and male internal genitalia paramesonephric (Mullerian) and mesonephric (Wolffian) ducts appear. The sexual differentiation process involves steps that occur due to growth factors, hormonal signals, and inherited genetic influences.
The paramesonephric ducts of both sides extend caudally until they reach the urogenital sinus, where they project into its posterior wall to become the Mullerian tubercle. The Mullerian duct has three parts.
- The first part is verticle and runs parallel to the Wolfian duct on its lateral side.
- The second part of the Müllerian duct lies horizontally and crosses the ipsilateral Wolfian duct anteriorly.
- The third part is vertical, which joins its counterpart in the midline.
The first two portions of Mullerian ducts make the fallopian tube. The third part canalizes after fusion with its counterpart to form the uterus, cervix, and upper 1/5th of the vagina.
In the female embryo, because of the absence of a Y chromosome and lack of testosterone from any testicular tissue, the typical sequence of developmental events results in canalization and fusion of the paramesonephric (Mullerian) ducts in the middle of the pelvis, which gives rise to the female pelvic organs. At this time, the mesonephric (Wolffian) ducts regress. Any abnormality that occurs during this phase of development may result in a variety of paramesonephric anomalies.
Blood Supply and Lymphatics
The uterus receives blood from the uterine and ovarian arteries, which arise from the anterior branch of the internal iliac artery. The uterine arteries are the main blood vessels that supply blood to the uterus. As the blood supply enters the myometrium, it branches into the arcuate arteries, which branch into the radial arteries. As they enter the endometrium level, they branch into the basal and spiral arteries.[3] Uterine arteries supply the different parts of the uterus and play an essential role in maintaining blood supply during menstrual and pregnancy.
The fundal area of the uterus chiefly drains into para-aortic lymph nodes along with the ovarian and fallopian tube lymphatic drainage. Some also drain into superficial inguinal lymph nodes along the round ligament. The lower portions of the uterus drain along uterine blood vessels into external and internal iliac lymph nodes.
Nerves
The internal pelvic organs receive nerve supply from the autonomic nervous system, sympathetic and parasympathetic nervous system. Autonomic T11 and T12 innervate the uterus, which derives its sympathetic nerve supply from the hypogastric plexus, and the parasympathetic supply is from S2 to S4. The uterus and cervix are sensitive to stretch (distension), and dilation of the cervix causes pain during normal vaginal delivery.[4]
Muscles
The uterus is located between the urinary bladder anteriorly and the rectum posteriorly. The average dimensions of the uterus in an adult female are 8 cm long, 5 cm across, and 4 cm thick. The uterine cavity has an average volume of 80 mL to 200 mL. The uterus is subdivided into three segments: the body, the cervix, and the fundus.
The uterus has three tissue layers, which include the following:
- Endometrium: is the inner lining, consisting of the functional (superficial) and basal endometrium. The functional layer responds to reproductive hormones. When this layer sheds, it results in menstrual bleeding. If there is damage to the basal endometrium, this can result in the formation of adhesions and fibrosis (Asherman syndrome).
- Myometrium: the muscle layer and is composed of smooth muscle cells.
- Serosa/Perimetrium: the thin outer layer composed of epithelial cells.
Physiologic Variants
The long axis of the cervix is rarely in line with the long axis of the body of the uterus. Commonly, the long axis of the body of the uterus is tilted forward over the long axis of the cervix, which is called anteflexion of the uterus. A backward tilt at this level is called retroflection. In 80 percent of women, the long axis of the uterus lies at the right angle to the long axis of the vagina with a forward tilt. It is called anteversion retroversion, which is present in 20 percent of women and is a backward tilt of the uterus over the vagina.[5] The anatomical position within the pelvis may vary. The normal position is an anteverted uterus, where the uterus tips forward, whereas a retroverted uterus is angled slightly posteriorly. The uterine position is also sometimes described relative to the location of the fundus; that is, an anteflexed uterus, which is normal and where the fundus tilts forward. On the other hand, a retroflexed uterus tilts posteriorly.
The uterus may also vary in size and shape depending on the female's reproductive phase and its response to female sex hormones.
- Pre-pubertal age: Uterus is small, and the cervix is longer than the body. The cervix-to-body ratio is 2:1.
- Reproductive age: Mature size, the body is bigger than the cervix, and the cervix-to-body ratio is 1:2.
- Post-menopausal: The uterus is atrophic, and the body size is smaller than the cervix. The cervix-to-body ratio is 2:1.
Also, a nulliparous uterus is usually smaller than a multiparous uterus. Furthermore, as the female reaches menopause, the uterus starts to atrophy chiefly due to a lack of hormonal stimulation and loss of menstruation.[6][7]
Surgical Considerations
Uterine anomalies of clinical significance include:
- Segmental hypoplasia (cervical, vaginal, fundal, or combined)
- Unicornuate uterus (with rudimentary horn and a communicating or noncommunicating endometrial cavity
- Uterine didelphys
- Bicornuate uterus
- Septate uterus
- Women exposed to diethylstilbestrol may develop a T-shaped uterus.
Clinical Significance
The uterus is affected by a variety of gynecologic disorders, including prolapse, fibroids, polyps, infections, cancer, malformations, and adhesions. Hysterectomy is the second most common surgical procedure performed on women in the United States (cesarean section is the most common). The following are the most common uterine pathologies.
- Polyp: It is a well-circumscribed collection of endometrial tissue within the uterine wall. It has smooth muscle cells, and it can extend into the endometrium cavity in the form of a polyp. It can be asymptomatic or present with painless abnormal uterine bleeding.[8] Small polyps without symptoms might resolve on their own. Progestins and gonadotropin-releasing hormone agonists may lessen the symptoms of poly, while the definitive treatment is surgical removal.
- Leiomyoma (fibroid): It is the most common benign tumor in females and often presents with multiple discrete tumors in the uterine cavity. It is more common in African-American ethnicity. It is a benign smooth muscle tumor, but it can rarely transform into malignant leiomyosarcoma. It is estrogen-sensitive, and its size increases in pregnancy and decreases after menopause. It may cause abnormal uterine bleeding and result in miscarriage. Severe bleeding in young females may cause iron deficiency anemia.[9] It usually gives an irregular shape to the uterus; it may cause constipation by compressing the rectum posteriorly. Oral medication is not often effective, and surgery, including hysterectomy or myomectomy, is considered the standard gold treatment.
- Endometrial hyperplasia: Excess estrogen stimulation causes abnormal endometrial gland proliferation. It is usually associated with an increased risk of endometrial carcinoma.
- Adenomyosis: It is an extension of endometrial tissue (glandular) into uterine myometrium caused by hyperplasia of the basal layer of the endometrium. It usually presents with dysmenorrhea and menorrhagia. Morphologically, it is an enlarged, uniform, and globular uterus.[10] Medical treatment includes NSAIDs and hormonal therapy (Combined estrogen-progestin pills, patches, and vaginal rings), while hysterectomy is considered the definitive treatment.
- Endometritis: It is an inflammation of the endometrium associated with retained products of conception following delivery, miscarriage, abortion, or with a foreign body—retained material in the uterus promotes infection by bacterial flora from the vagina or intestinal tract.
- Endometriosis: It is a condition in which non-neoplastic endometrial glands or stroma are present outside the endometrial cavity. It can occur anywhere, but the most common sites are the ovary, pelvis, and peritoneum. In the ovary, it appears as an endometrioma (Blood-filled chocolate cyst). Evidence suggests that it is due to the retrograde flow of menstrual blood.[11] On the ultrasonogram, it appears as a homogenous echotexture and hypoechoic. Medical treatment includes NSAIDs, gonadotropin-releasing hormones, progestin therapy, and aromatase inhibitors. If the patient is having difficulty in conceiving, then surgery to remove the endometriosis implants while preserving the uterus and ovaries may increase the chances of success.
Uterine cancer is the most common gynecologic cancer in developed countries and is associated with excess estrogen. Exogenous sources of estrogen include tamoxifen use or unopposed estrogen replacement therapy. Tamoxifen increases endometrial cancer risk due to its ability to stimulate the estrogen receptors found in the endometrium. Endogenous sources of estrogen include polycystic ovary syndrome, obesity, and estrogen-secreting tumors such as granulosa cell tumors. The majority of women with endometrial cancer present with abnormal vaginal bleeding or postmenopausal vaginal bleeding. Less commonly, they may present with abdominal pain, change in bowel habits, weight loss, and bloat.
Media
(Click Image to Enlarge)
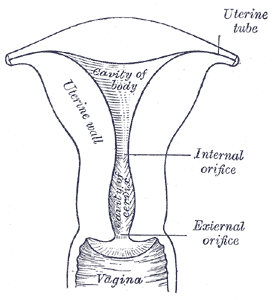
The Uterus. The illustration depicts the posterior half of the uterus and the upper part of the vagina, including the uterine tube, cavity of body, uterine wall, internal orifice, and the vagina.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Chaudhry SR, Chaudhry K. Anatomy, Abdomen and Pelvis: Uterus Round Ligament. StatPearls. 2024 Jan:(): [PubMed PMID: 29763145]
Craig ME, Sudanagunta S, Billow M. Anatomy, Abdomen and Pelvis: Broad Ligaments. StatPearls. 2024 Jan:(): [PubMed PMID: 29763118]
Chaudhry R, Chaudhry K. Anatomy, Abdomen and Pelvis: Uterine Arteries. StatPearls. 2024 Jan:(): [PubMed PMID: 29489202]
Tong XK, Huo RJ. The anatomical basis and prevention of neurogenic voiding dysfunction following radical hysterectomy. Surgical and radiologic anatomy : SRA. 1991:13(2):145-8 [PubMed PMID: 1925917]
Fidan U, Keskin U, Ulubay M, Öztürk M, Bodur S. Value of vaginal cervical position in estimating uterine anatomy. Clinical anatomy (New York, N.Y.). 2017 Apr:30(3):404-408. doi: 10.1002/ca.22854. Epub 2017 Mar 9 [PubMed PMID: 28192868]
Alimi Y, Iwanaga J, Loukas M, Tubbs RS. The Clinical Anatomy of Endometriosis: A Review. Cureus. 2018 Sep 25:10(9):e3361. doi: 10.7759/cureus.3361. Epub 2018 Sep 25 [PubMed PMID: 30510871]
Al-Qattan MM, Al-Qattan AM. Fibromodulin: Structure, Physiological Functions, and an Emphasis on its Potential Clinical Applications in Various Diseases. Journal of the College of Physicians and Surgeons--Pakistan : JCPSP. 2018 Oct:28(10):783-790 [PubMed PMID: 30266125]
Hodler J, Kubik-Huch RA, von Schulthess GK, Kinkel K, Ascher SM, Reinhold C. Benign Disease of the Uterus. Diseases of the Abdomen and Pelvis 2018-2021: Diagnostic Imaging - IDKD Book. 2018:(): [PubMed PMID: 31314373]
Rosa P, Pidhorecky I. A Case of Intravenous Leiomyomatosis with Involvement of a Renal Vein. Annals of vascular surgery. 2018 Nov:53():271.e11-271.e13. doi: 10.1016/j.avsg.2018.05.061. Epub 2018 Aug 6 [PubMed PMID: 30092420]
Level 3 (low-level) evidencePaul PG, Gulati G, Shintre H, Mannur S, Paul G, Mehta S. Extrauterine adenomyoma: a review of the literature. European journal of obstetrics, gynecology, and reproductive biology. 2018 Sep:228():130-136. doi: 10.1016/j.ejogrb.2018.06.021. Epub 2018 Jun 12 [PubMed PMID: 29940416]
Pääkkö E, Niinimäki M. Diagnostics of endometriosis by using magnetic resonance imaging. Duodecim; laaketieteellinen aikakauskirja. 2017:133(1):61-7 [PubMed PMID: 29200236]