Introduction
Blepharoplasty is a surgical technique for correcting defects, deformities, and disfigurations of the eyelids; and for aesthetically modifying the eye region of the face. With excision and removal of skin and adipocyte fat and the reinforcement of the corresponding muscle and tendon tissues, blepharoplasty resolves functional and cosmetic problems of the periorbita, which is the area from the eyebrow to the upper portion of the cheek. The procedure is most common among women, who accounted for approximately 85% of blepharoplasty procedures in 2014 in the USA and 88% of such procedures in the UK.
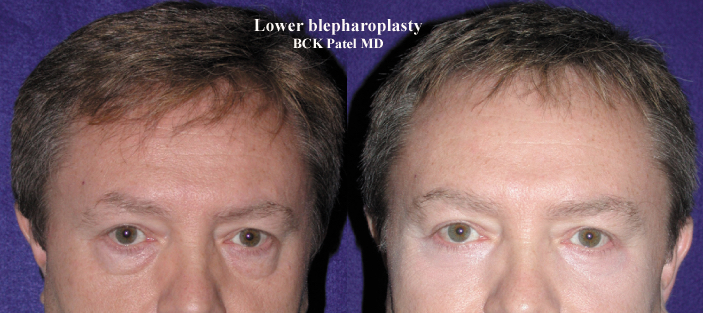
The operative goal of a blepharoplasty is the restoration of the correct functioning to the affected eyelid(s) and the restoration of the aesthetics of the eye-region of the face.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Lower Eyelid Laxity
When it comes to evaluating lower eyelids, there are many factors that need to be taken into consideration. One of the most important tests for this evaluation is called the snap-back test. This test is performed by pulling the lower eyelid away from the eye and assessing how quickly and easily the eyelid returns to its normal position. During this test, if the patient needs to blink for the eyelid to return to its original position, then laxity of the lower eyelid or canthal tendon is present. Moreover, the ability to pull the lower eyelid from the globe more than 5mm is another indication that lower eyelid laxity is present.
Through careful evaluation of the lower eyelid position, we can determine if lateral canthal tendon laxity is present. As we age, the collagen fibers in our eyelids become laxer and the eyelid will sag more. Therefore, the position of the lower eyelid can be lower than usual. This condition is termed inferior scleral show and can be measured in millimeters. The physician should measure the position of the lower eyelid in relation to the inferior corneal limbus.
The normal anatomical position of the lateral canthal tendon is higher than that of the medial canthal tendon. A change in the relationship where the lateral canthal tendon position falls lower than the medial canthal tendon would indicate that lateral canthal tendon laxity is present. In contrast, medial canthal tendon laxity would manifest clinically with either punctal eversion or increase in distance between the lower punctum and lacrimal caruncle.
Lateral canthal laxity can be addressed during a lower eyelid blepharoplasty procedure. The treatment of lower eyelid lateral canthal laxity is either through lateral canthopexy or canthoplasty. In cases of any medial canthal tendon laxity, a medial canthoplasty can be performed to address it.
The skin laxity of the lower eyelid is called dermatochalasis. As we age, the upper and lower eyelids’ skin can become redundant. The skin appears very loose with many deep and superficial rhytids. There is a condition called blepharochalasis, which causes severe laxity of the eyelid skin during younger ages. These patients often report intermittent edema of the tissues around the eyes, including the eyelids. This condition is usually genetic and is autosomal dominant.
To correct lower eyelid skin laxity, surgeons use a method called the pinch technique. This procedure treats moderate to severe forms of skin laxity of the lower eyelid.
Laser skin resurfacing, either with CO2 or Erbium Yag laser, can also be used to treat skin laxity, but are typically resolved for milder cases. These types of laser treatments are not suitable for all skin types. The CO2 laser resurfacing is only suitable for Fitzpatrick skin types 1 to 3, while Erbium Yag laser can be used conservatively on darker skin types.
The Pinch Technique
This method is suitable for patients with severe laxity of the lower eyelid skin. The physician should ask the patient to look up while opening his/her mouth. The physician should pinch the skin of the lower eyelid below the lashes using a smooth forceps and mark the area with a marking pen. It is recommended to repeat this step to ensure that the marking is correct. This area can then be injected with local anesthetic placed in the subcutaneous plane. The skin can be excised and then closed with a running 6-0 plain gut suture. The video below demonstrates the pinch technique.
Indications
The thorough pre-operative medical and surgical histories, and the physical examination of the patient’s periorbital area (eyebrow-to-cheek-to-nose) determine if the patient can safely undergo a blepharoplasty procedure to feasibly resolve the functional and aesthetic indications presented by the patient. Sequentially, lower eyelid blepharoplasty can successfully address the anatomic matters of excess eyelid skin, slackness of the eye-muscles and of the orbital septum (palpebral ligament), excess orbital fat, malposition of the lower eyelid, and prominence of the nasojugal groove, where the orbit (eye socket) meets the slope of the nose.
Concerning the upper eyelid, a blepharoplasty procedure can resolve the loss of peripheral vision caused by the slackness of the upper-eyelid skin draping over the eyelashes. The outer and the upper portions of the field of vision of the patient are affected and cause him or her difficulty in performing mundane activities such as driving an automobile and reading a book.
Contraindications
Patients who may seek secondary gains, such as improvement in personal relationships are not good candidates for cosmetic surgery. Patients who judge the success of the surgery by their satisfaction rather than by restoration and minimization of aging changes.
Absolute contraindications include any pathologic condition of the eyelids or orbital structures. Relative contraindications include any medical conditions that might alter the patient’s response to anesthesia or unrealistic patient expectations.
Technique or Treatment
In an eye surgery procedure, the usual correction or modification is of the upper and the lower eyelids, and of the surrounding tissues of the eyebrows, the upper nasal-bridge area, and the upper portions of the cheeks, which are achieved by modifying the periosteal coverings of the facial bones that form the orbit. [1][2]The periosteum comprises two-layer connective tissues that cover the bones of the human body:
- The external layer of networks of dense, connective tissues with blood vessels
- The internal, deep layer of collagenous bundles composed of spindle-shaped cells of connective tissue, and a network of thin, elastic fibers.
The importance of lower eyelid assessment is crucial to achieving outstanding results. Hence this procedure is challenging for many surgeons including the most experienced ones.
Complications
Complications of blepharoplasty include:[3][4]
- Infection
- Bleeding
- Wound separation
- Suture cysts
- Asymmetry
- Insufficient or insufficient skin or fat removal
- Excessive muscle removal
- Excessive internal and external scarring
- Inappropriate crease
- Rounding at the lateral commissure
- Drooping upper eyelid
- Fat necrosis
- Swelling on the eyeball surface
- Lacrimal duct injury
- Double vision
- Loss of vision
- Anesthetic complications
Clinical Significance
Blepharoplastic restores the correct functioning to the affected eyelid(s) and the aesthetics of the eye-region of the face. This is achieved by eliminating excess skin from the eyelid(s), smoothing the underlying eye muscles, tightening the supporting structures, and resecting excess fat of the retroseptal area of the eye to produce a smooth anatomic transition from the lower eyelid to the cheek.
Enhancing Healthcare Team Outcomes
Lower eyelid blepharoplasty is primarily done by the ophthalmologist and plastic surgeons. However, the patients may be referred by the primary care provider or nurse practitioner. Unlike upper eyelid blepharoplasty, lower eyelid blepharoplasty is more technically challenging and prone to complications. All patients must be warned of potential complications. When done well, the results are excellent.[5] (Level V) However, the durability of the procedures remains questionable.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Huang SH, Lin YN, Lee SS, Huang YH, Takahashi H, Chou CK, Lin TY, Chen RF, Kuo YR, Lai CS, Lin SD, Lin TM. Three Simple Steps for Refining Transcutaneous Lower Blepharoplasty for Aging Eyelids: The Indispensability of Micro-Autologous Fat Transplantation. Aesthetic surgery journal. 2019 Oct 15:39(11):1163-1177. doi: 10.1093/asj/sjz005. Epub [PubMed PMID: 30668643]
Gawdat TI, Elsherif EAE, Alahmadawy YA, Mostafa YSE. Management of tear trough deformity with and without tear trough-orbicularis retaining ligament complex release in transconjunctival blepharoplasty: a comparative study. International journal of ophthalmology. 2019:12(1):89-93. doi: 10.18240/ijo.2019.01.14. Epub 2019 Jan 18 [PubMed PMID: 30662846]
Level 2 (mid-level) evidenceLower Eyelid Blepharoplasty: Does the Literature Support the Longevity of This Procedure?, Wilson SC,Daar DA,Maliha SG,Abdou SA,Levine SM,Baker DC,, Aesthetic surgery journal, 2018 Jul 31 [PubMed PMID: 30084870]
Lemaître S, Lévy-Gabriel C, Desjardins L, González-Candial M, Gardrat S, Dendale R, Cassoux N, Couturaud B. Outcomes after surgical resection of lower eyelid tumors and reconstruction using a nasal chondromucosal graft and an upper eyelid myocutaneous flap. Journal francais d'ophtalmologie. 2018 May:41(5):412-420. doi: 10.1016/j.jfo.2017.10.008. Epub 2018 May 16 [PubMed PMID: 29778279]
Kim MJ,Oh TS, Treatment for ophthalmic paralysis: functional and aesthetic optimization. Archives of craniofacial surgery. 2019 Feb; [PubMed PMID: 30840813]