Introduction
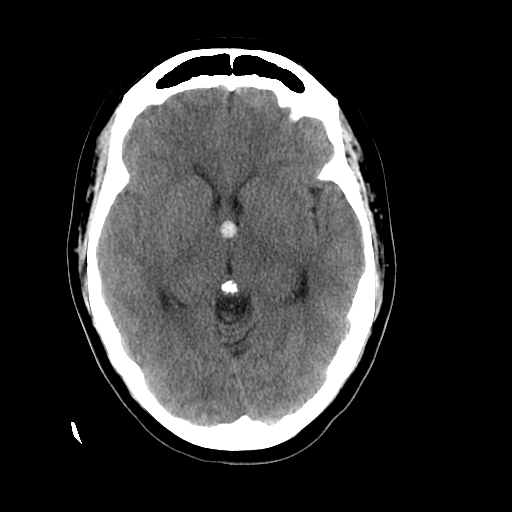
The colloid cyst is a benign growth usually located in the third ventricle and at or near the foramen of Monro, which is at the anterior aspect of the brain's third ventricle.[1] The colloid cyst is an epithelial-lined cyst filled with gelatinous material. The gelatinous material commonly contains mucin, old blood, cholesterol, and ions (See Image. Colloid Cyst, Head Computed Tomography).[1] Colloid cysts can cause various symptoms, including headaches, diplopia, memory issues, and vertigo. Rarely, colloid cysts have been cited as a cause of sudden death. When colloid cysts are symptomatic, they most commonly cause headaches, nausea, and vomiting secondary to obstructive hydrocephalus. The obstructive hydrocephalus is precipitated by blocking the cerebrospinal fluid egress from the lateral ventricles at the foramen of Monro, which connects the lateral and third ventricles.[2]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The precise etiology of colloid cysts is unclear and still debatable. In the early 20th century, the suggested etiology was that the cyst was a remnant of the paraphysis element. The paraphysis element is an embryonic structure located at the diencephalon's anterior portion between the telencephalon's 2 hemispheres. As colloid cysts have also been found in the cerebellum, frontal lobe, and pontomesencephalon, other theorized origins exist. Other etiologies include remnants of respiratory epithelium, an ependymal cyst from the diencephalon, and invagination of the neuroepithelium of the lateral ventricle, causing a cyst to form.[2]
Epidemiology
Colloid cyst accounts for less than 2% of all primary brain tumors. More than 99% of all colloid cysts are reported to occur at the rostral end of the third ventricle, at or near the foramen of Monro. Colloid cysts account for approximately 1 in 5 intraventricular primary brain tumors. Most patients diagnosed with a colloid cyst are in their third through the seventh decade of life, but cases have rarely been reported as early as the first year of life.
Pathophysiology
Most colloid cysts identified are currently asymptomatic and were incidentally found on imaging. When a colloid cyst does cause issues, it most commonly causes obstructive hydrocephalus. The colloid cyst is most commonly found in the rostral third ventricle at or near the foramen of Monro. The foramen of Monro is the conduit of cerebrospinal fluid (CSF) outflow from the lateral ventricles to the third ventricle. A colloid cyst can act as a ball valve, stopping CSF flow from the lateral ventricles. If this occurs, CSF backs up into the lateral ventricles and causes ventriculomegaly and hydrocephalus. Some have posited that colloid cysts can cause intermittent obstructive hydrocephalus, thus causing intermittent symptoms. Colloid cysts tend to grow very slowly over time. Some may never reach a size that will cause an issue and can be followed, whereas others grow more quickly and become symptomatic with time.
Histopathology
Grossly, a colloid cyst is a unilocular round structure filled with a viscous material. Microscopically, the cell wall is unicellular and typically composed of columnar epithelium, which may or may not be ciliated. The cyst contents are normally void of living cells and composed of desquamated ghost cells and filamentous material. The mucin stains are positive for periodic acid-Schiff stain. The epithelial cyst wall stains are positive for keratin and epithelial membrane antigen.
History and Physical
Most colloid cysts are found incidentally on brain imaging for other reasons. When a colloid cyst is symptomatic, it most commonly causes noncommunicating hydrocephalus. Symptoms of hydrocephalus can include headaches, nausea, vomiting, lethargy, coma, and death. If the hydrocephalus is slowly progressive, the patient can have more subtle findings, including urinary incontinence, trouble with walking, falls, altered mentation, and memory deficits. The physical exam should be normal for asymptomatic colloid cysts. Physical examination findings in a patient with hydrocephalus caused by a colloid cyst may include lethargy, impaired upward gaze, unsteady gait, ataxia, hyperreflexia, and, in cases of chronic hydrocephalus, papilledema or frontal release signs.
Evaluation
Immediate evaluation of suspected colloid cysts includes the airway, breathing, and circulation of emergency medical management if the patient may be at risk for acute hydrocephalus and neurologic deterioration. A thorough neurologic exam is important to identify deficits, but imaging remains the cornerstone of evaluating patients with a colloid cyst. Plain radiographs of the head typically do not visualize a colloid cyst, so computed tomography (CT) and magnetic resonance imaging (MRI) of the head are more critical imaging studies.
Head CT
CT of the head can be quickly obtained to identify acute hydrocephalus. On CT imaging, the colloid cyst is typically a circular, hyperdense mass at or near the foramen of Monro. Rarely are colloid cysts isodense, hypodense, or calcified.
Brain MRI
MRI is the preferred method for imaging colloid cysts. On T1 sequencing, a colloid cyst can have variable characteristics and be either hyperintense, isointense, or hypointense. With gadolinium administration, the colloid cysts should not be enhanced. Rarely a peripheral enhancement will be noted around the colloid cyst, which most likely represents a vessel stretched over the colloid cyst.
On T2 sequence imaging, most colloid cysts are hypointense. They may also have a heterogeneous T2 signal. Low signal intensity on T2 imaging may suggest the contents of the colloid cyst are more viscous and, thus, harder to aspirate. Most colloid cysts have a similar intensity to the surrounding CSF on fluid-attenuated inversion recovery sequencing. Most colloid cysts have decreased signal intensity on diffusion-weighted imaging.
Treatment / Management
Treatment and management depend on whether the colloid cyst is found incidentally or is symptomatic.[3][4][5][6] The condition should be treated if the colloid cyst is symptomatic and causes hydrocephalus. For acute, life-threatening hydrocephalus, treatment should be the next priority after ensuring adequate airway, breathing, and circulation. An external ventricular drain can be placed to relieve acute hydrocephalus and may be a life-saving procedure. After acute, life-threatening hydrocephalus has either been treated or ruled out, the clinician can deal with the colloid cyst. Current treatment options include craniotomy with excision via a transcallosal or transcortical route, endoscopic removal, and stereotactic aspiration.
Craniotomy for Colloid Cyst Removal
A colloid cyst can be removed with a craniotomy. A craniotomy is a surgery where an incision is made in the scalp, and part of the skull is removed for the duration of the surgery; then, the skull is put back in place. Two separate routes exist to remove the colloid cysts: transcallosal and transcortical. In the transcallosal approach, the 2 frontal hemispheres are split apart, and a surgical corridor is created through the rostral end of the genu of the corpus callosum to access the colloid cyst.
For the transcortical route, a surgical corridor is developed directly through the brain cortex, most commonly through the right frontal and middle gyrus, to access the lateral ventricle. The colloid cyst can then be removed through the lateral ventricle. Surgical removal of a colloid cyst via craniotomy carries the highest initial risk but is associated with the lowest rates of recurrence and need for reoperation. Open craniotomy offers greater flexibility in accessing the cyst, making it a more suitable option for larger cysts, though its effectiveness depends on the chosen surgical approach.[7][8]
Endoscopic Removal of a Colloid Cyst
An endoscopic surgery consists of making a small incision in the scalp and a small hole in the bone. A small tube, typically called a sheath, is advanced through the brain to access the lateral ventricle. An endoscope can then be passed into the lateral ventricle to remove the colloid cyst. In its simplest form, an endoscopic is a tube with a light, camera, and working channel. The light provides illumination for the camera to see what is going on. The working channel allows the surgeon to get instruments and tools before the camera performs surgery. Endoscopic removal of a colloid cyst tends to have less up-front risk than open surgery but also may have a slightly higher reoperation rate than open surgery. The endoscopic approach may not be suitable for all colloid cysts depending on the size and location of the cyst.[8][9]
Stereotactic Aspiration of a Colloid Cyst
A third option to treat a colloid cyst is a stereotactic aspiration. This is performed by making a small incision in the scalp and then a small hole in the bone. The surgeon then advances a needle through the brain and into the cyst using some variety of either frame-based or frameless neuronavigation. The contents of the colloid cyst may be able to be aspirated, decreasing its size.
Aspiration of a colloid cyst may not be achievable if the contents of the colloid cyst are particularly thick or if there is no safe corridor to the colloid cyst. Stereotactic aspiration of a colloid cyst has less relative surgical risk than an endoscopic or open resection of the colloid cyst. Still, it has the highest reoperation rate compared to the other 2 treatment modalities. With the aspiration of the colloid cyst, the cyst is left in place and decompressed. The cyst may reexpand over time and become symptomatic again.[8]
Asymptomatic Colloid Cyst
An asymptomatic colloid cyst does not necessarily warrant treatment. If there is hydrocephalus, all surgeons would agree that surgery is warranted, but if a colloid cyst is found incidentally, then surgery is not necessarily warranted. Colloid cysts smaller than 10 mm or more centrally located in the third ventricle are less likely to obstruct the near term. Such colloid cysts may be monitored with serial imaging, looking for colloid cyst size and location and any evidence of hydrocephalus. There have been infrequent reported cases of colloid cysts, which were followed clinically but caused acute hydrocephalus and death.
Differential Diagnosis
There are other lesions that can appear similar to a colloid cyst on imaging, including:
- Craniopharyngioma
- Ependymoma
- Germinoma
- Giant cell astrocytoma
- Hemorrhage
- Lymphoma
- Meningioma
- Metastasis
- Pilocytic astrocytoma
- Pituitary tumor
Prognosis
Some colloid cysts can be watched for years to decades without any issue. Others can slowly grow in size or cause subacute or acute hydrocephalus. With complete surgical resection, the prognosis is good, and colloid cysts rarely recur after complete resection. However, rare cases of sudden death have been reported with colloid cysts, which are usually attributed to acute obstructive hydrocephalus.
Complications
Complications of colloid cysts include:
- Hydrocephalus
- Brain herniation
- Death
- Intralesional hemorrhage [10]
Deterrence and Patient Education
Patients kept on observation should be instructed to report to the nearest emergency department should they develop severe headaches or vomiting.
Enhancing Healthcare Team Outcomes
The CNS colloid cyst is best managed by an interprofessional team, including neurosurgeons, neurologists, radiologists, and neuroscience nurses. When a colloid cyst is diagnosed, the biggest dilemma is managing it. The minimally invasive approaches have less morbidity but a higher recurrence and reoperation rate. Removing a colloid cyst via a craniotomy has the highest up-front surgical risk but may have the lowest recurrence and reoperation rate.
The open craniotomy provides more degrees of freedom for access to the colloid cyst and may be more suitable for larger colloid cysts but does have limitations based on the approach chosen. A thorough discussion should be undertaken with the patient, and the patient should be allowed to decide which approach they favor. Specialty-trained nurses in perianesthesia and operating rooms, as well as critical assistance in the care, monitor patients, and report changes in status to the team. An interprofessional team approach will result in good outcomes.
Media
(Click Image to Enlarge)
References
Ahmed SI, Javed G, Laghari AA, Bareeqa SB, Aziz K, Khan M, Samar SS, Humera RA, Khan AR, Farooqui MO, Shahbaz A. Third Ventricular Tumors: A Comprehensive Literature Review. Cureus. 2018 Oct 5:10(10):e3417. doi: 10.7759/cureus.3417. Epub 2018 Oct 5 [PubMed PMID: 30542631]
Barbagallo GM, Raudino G, Visocchi M, Maione M, Certo F. Out-of-third ventricle colloid cysts: review of the literature on pathophysiology, diagnosis and treatment of an uncommon condition, with a focus on headache. Journal of neurosurgical sciences. 2019 Jun:63(3):330-336. doi: 10.23736/S0390-5616.16.03831-5. Epub 2016 Sep 7 [PubMed PMID: 27603409]
Heller RS, Heilman CB. Colloid Cysts: Evolution of Surgical Approach Preference and Management of Recurrent Cysts. Operative neurosurgery (Hagerstown, Md.). 2020 Jan 1:18(1):19-25. doi: 10.1093/ons/opz059. Epub [PubMed PMID: 31220314]
Lara-Reyna JJ, Uribe-Cardenas R, Perera I, Szerlip N, Giamouriadis A, Savage N, Haussner T, Souweidane MM. Endoscopic removal of recurrent colloid cysts. Journal of neurosurgery. 2019 Apr 12:132(5):1636-1641. doi: 10.3171/2018.12.JNS181859. Epub 2019 Apr 12 [PubMed PMID: 30978688]
Ibáñez-Botella G, Segura M, De Miguel L, Ros B, Arráez MÁ. Purely neuroendoscopic resection of intraventricular tumors with an endoscopic ultrasonic aspirator. Neurosurgical review. 2019 Dec:42(4):973-982. doi: 10.1007/s10143-018-1011-8. Epub 2018 Jul 17 [PubMed PMID: 30019320]
Haider G, Laghari AA, Shamim MS. Choosing between endoscopic or microscopic removal of third ventricle colloid cysts. JPMA. The Journal of the Pakistan Medical Association. 2017 Sep:67(9):1458-1459 [PubMed PMID: 28924297]
Kumar V, Behari S, Kumar Singh R, Jain M, Jaiswal AK, Jain VK. Pediatric colloid cysts of the third ventricle: management considerations. Acta neurochirurgica. 2010 Mar:152(3):451-61. doi: 10.1007/s00701-009-0531-y. Epub 2009 Oct 25 [PubMed PMID: 19856141]
Yadav YR, Yadav N, Parihar V, Kher Y, Ratre S. Management of colloid cyst of third ventricle. Turkish neurosurgery. 2015:25(3):362-71. doi: 10.5137/1019-5149.JTN.11086-14.1. Epub [PubMed PMID: 26037175]
Yadav YR, Parihar V, Pande S, Namdev H. Endoscopic management of colloid cysts. Journal of neurological surgery. Part A, Central European neurosurgery. 2014 Sep:75(5):376-80. doi: 10.1055/s-0033-1343984. Epub 2013 May 22 [PubMed PMID: 23700169]
Al Abdulsalam HK, Ajlan AM. Hemorrhagic colloid cyst. Neurosciences (Riyadh, Saudi Arabia). 2018 Oct:23(4):326-333. doi: 10.17712/nsj.2018.4.20180051. Epub [PubMed PMID: 30351291]