Introduction
The male urethra is a crucial component of the male genitourinary system. Its function is not limited to just micturition, as it is also an essential portion of the male reproductive system. The urethra is a dynamic fibromuscular tube which serves as the terminal region of both the male urinary and reproductive systems. The average male urethra is 20 cm long and begins within the bladder wall and ends in the distal glans of the penis.
Structure
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure
The male urethra is unique because it is a relatively long structure that passes through several compartments in the body and therefore, receives blood supply and innervation from a broad array of sources. The male urethra receives blood supply from the inferior vesical artery, bulbourethral artery, and the internal pudendal artery. The sympathetic, parasympathetic and visceral innervation to the male urethra gets delivered through the prostatic plexus.
The male urethra can subdivide into four parts, each part containing unique gross and histological features.
- Pre-prostatic urethra
- Location: Extends inferiorly from urinary bladder and ends prior to entering the prostate gland.
- Gross Features: It is embedded within the walls of the urinary bladder and is typically 0.5 to 1.5 cm in length.
- Histological Features: transitional epithelium (urothelium)
- Prostatic urethra
- Location: Completely encompassed within the prostate gland.
- Gross Features: This is generally the widest part of the male urethra, and contains the urethral crest, seminal colliculus, prostatic utricle, and the orifices of the prostatic ducts - typically 3.0 to 4.0 cm in length.
- Histological Features: Urothelium immediately surrounded by the glandular and stromal tissue of the periurethral zone of the prostate.
- Membranous urethra
- Location: Begins immediately outside of the prostate and ends just prior to entering the bulb of the penis.
- Gross Features: Passes through the deep perineal pouch, the external urethral sphincter, and the perineal membrane. Bulbourethral (Cowper) glands lie just posterior to this portion - typically 1 to 1.5 cm in length.
- Histological Features: The urothelium changes into pseudostratified columnar epithelium. Thick layers of skeletal muscle is present at the level of the external urethral sphincter. Bulbourethral glands may be seen in a cross-section view.
- Spongy urethra
- Location: Travels the entire length of the penis via the corpus spongiosum.
- Gross Features: Widens initially as it enters the bulb of the penis and widens again in the glans of the penis, forming the navicular fossa. Bulbourethral and urethral glands empty into this portion. Typically around 15 cm in length.
- Histological Features: Pseudostratified columnar epithelium except for the terminal portion which is stratified squamous epithelium. The corpus spongiosum is immediately surrounding this portion of the urethra.[1][2][3]
Function
Overall the function of the male urethra is to allow passage of urine and semen. The urethra connects the distal portions of the urinary system, such as the urinary bladder, to the external environment and allows for urine excretion from the body. Likewise, the urethra provides a conduit for ejaculate to pass from the distal portions of the male reproductive system, specifically the vas deferens, seminal vesicles, and prostate.
Microscopically there are groups of cells that serve essential functions related to the urethra. The epithelial cells lining the lumen of the urethra are protective against the constant exposure to urine, seminal fluid and the external environment. The submucosal layer is supportive due to its extensive vascular content. The fibromuscular layer of cells is the outer-most portion of the urethra and provides structure, propulsion, and tone to the urethra.[4]
Tissue Preparation
Preparing a urethral tissue sample for histologic observation is similar to the preparation of any other tissue. The tissue is first fixed with a solution to preserve the sample. Next, the tissue is processed, which generally includes dehydrating and embedding in a wax mold. Lastly, the wax mold gets sliced into thin sections, and the tissue sample is washed and transferred to a slide. At this point, the tissue sample has been harvested and processed, but still needs to undergo a staining process. Different stains reveal structural components in different colors and intensities, and therefore, the stain used is dependant upon the type of tissue and the structural elements sought.[5][6]
Histochemistry and Cytochemistry
The two commonly utilized histological stains to observe the male urethra are the hematoxylin and eosin stain and the trichrome stain.
The hematoxylin and eosin stain contains an acidic and basic dye, which allows for a general visualization of the cell and its different cellular components like the nucleus, cytoplasmic granules, and proteins. In regards to general observation of the male urethra, this stain is useful in determining the type of epithelium in a particular cross-section.
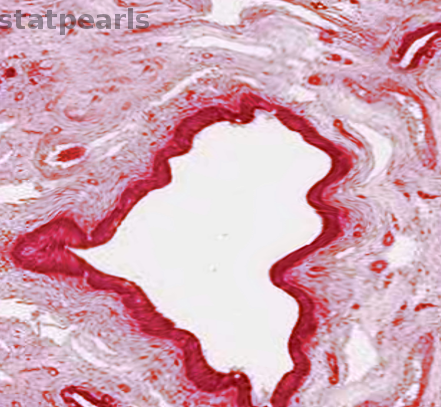
The trichrome stain, as its name implies, contains three different dyes. This stain is able to differentiate muscle, especially smooth muscle, from connective tissues like collagen. This is beneficial when looking at cross-sections and trying to determine which portion of the urethra you are observing. Depending on the muscular and connective tissue environment surrounding the urethra, you can get a good idea of where in the male urethra the cross section was taken. For example, if there was suspicion of fibrosis involving the smooth muscle layers of the urethra, a trichrome stain would be well suited to observe and contrast the proportion of smooth muscle to connective tissue.[7]
Microscopy, Light
When observing a specimen of the male urethra under light microscopy, there are several vital elements to identify. In a standard cross-sectional preparation, the first thing to look for is the lumen. The lumen will appear as empty white space on the slide surrounded by epithelial cells. In a well-prepared slide that doesn't contain artifacts, nothing should be within the lumen. Next, it is important to determine the type of epithelium that is lining the lumen to determine from which region of urethra the specimen came.
In the urethra, there will be two types of epithelium. The proximal epithelium is transitional epithelium (uroepithelium). These cells appear columnar near the basement membrane and become more rounded and dome-shaped towards the lumen. The more distal epithelium is pseudostratified columnar epithelium and appears as multiple layers of columnar cells. In reality, each cell makes contact with the basement membrane, and therefore, there is only one layer of epithelium. Single layers of epithelial cells are normally referred to as simple, but since the cells overlap in such a unique manner in vivo and during histological preparation, they tend to take on the appearance of being stratified. Because of these characteristics, this type of epithelium is referred to as pseudostratified.
Microscopy, Electron
Electron microscopy is a relatively young imaging technique that allows observation of the ultrastructure of cells. Since the first use of electron microscopy in the early 1930s, it has revolutionized our understanding of cellular biology. The ultrastructure of a cell refers to the biological structures that can't be seen with standard light microscopy, such as cilia and extracellular proteins. Through the utilization of electron microscopy, it has been possible to better characterize the features of the male urethra. For example, some even more subspecialized regions of the male urethra have been recently described due to certain portions of the epithelium of the prostatic and spongy urethra expressing cilia on their apical surfaces. Research has shown that some regions of epithelium contain higher concentrations of glycogen compared to the rest. These findings suggest that the urethra is a more complex and dynamic organ than previously understood.[8][9][10]
Pathophysiology
The urethra, being open to the external environment, is susceptible to infection, disease, and damage. Although biopsy and histological observation of the male urethra are not always necessary during the workup of a urethral disease, it is crucial to understand the anatomy and histological characteristics of the urethra to best be able to understand, manage and treat disease.
One of the most common pathological processes that involve the male urethra is urinary tract infections. Urinary tract infections are usually the result of bacteria that enter the body through the distal opening to the urethra. The exact manifestation and colonization of the bacteria depend on the specific agent, some bacteria may adhere to the epithelial lining, penetrate through the lining, or continue traveling towards the bladder and upper portions of the urinary tract. Risk factors for urinary tract infections are poor hygiene, low urinary outflow and being immunocompromised.[11]
A much less common pathological process involving the male urethra is cancer. Although male urethral cancers account for less than 1% of urologic malignancies, it is important to understand the pathophysiology, presentation, and impact of this rare but serious disease. Due to the limited amount of cases per year, there is little standardized data to guide physicians towards the best treatment choices. In the past, the primary surgical treatment option was a complete or near-complete penectomy. Though this may ensure the complete removal of cancerous cells, it has a severe impact on the patient's physical and mental wellbeing. Moreso today, where precision and efficiency matter more than ever, more conservative procedures like partial urethrectomies are being performed to remove less tissue and allow patients to maintain a better quality of life.[12]
Clinical Significance
The male urethra is an area of clinical significance because of its role in both the urinary and reproductive systems. By understanding the dual role played by the male urethra, health care providers are better able to take care of their patient as a whole. Understanding that a urinary tract infection may cause pain during urination is only part of the whole patient care picture. Going further and considering that it may increase susceptibility to sexually transmitted infections or affect the ability to conceive ensures that complete patient care and counseling take place. Though a commonly overlooked organ, the male urethra is a dynamic and vital structure that is of immense clinical significance due to both its direct physical and indirect integration with multiple systems of the body.
Media
References
Kohler TS, Yadven M, Manvar A, Liu N, Monga M. The length of the male urethra. International braz j urol : official journal of the Brazilian Society of Urology. 2008 Jul-Aug:34(4):451-4; discussion 455-6 [PubMed PMID: 18778496]
Yucel S, Baskin LS. Neuroanatomy of the male urethra and perineum. BJU international. 2003 Oct:92(6):624-30 [PubMed PMID: 14511049]
Holstein AF, Davidoff MS, Breucker H, Countouris N, Orlandini G. Different epithelia in the distal human male urethra. Cell and tissue research. 1991 Apr:264(1):23-32 [PubMed PMID: 2054843]
Jung J, Ahn HK, Huh Y. Clinical and functional anatomy of the urethral sphincter. International neurourology journal. 2012 Sep:16(3):102-6. doi: 10.5213/inj.2012.16.3.102. Epub 2012 Sep 30 [PubMed PMID: 23094214]
Copper JE, Budgeon LR, Foutz CA, van Rossum DB, Vanselow DJ, Hubley MJ, Clark DP, Mandrell DT, Cheng KC. Comparative analysis of fixation and embedding techniques for optimized histological preparation of zebrafish. Comparative biochemistry and physiology. Toxicology & pharmacology : CBP. 2018 Jun:208():38-46. doi: 10.1016/j.cbpc.2017.11.003. Epub 2017 Nov 20 [PubMed PMID: 29157956]
Level 2 (mid-level) evidenceAlturkistani HA, Tashkandi FM, Mohammedsaleh ZM. Histological Stains: A Literature Review and Case Study. Global journal of health science. 2015 Jun 25:8(3):72-9. doi: 10.5539/gjhs.v8n3p72. Epub 2015 Jun 25 [PubMed PMID: 26493433]
Level 3 (low-level) evidenceChang JY, Kessler HP. Masson trichrome stain helps differentiate myofibroma from smooth muscle lesions in the head and neck region. Journal of the Formosan Medical Association = Taiwan yi zhi. 2008 Oct:107(10):767-73. doi: 10.1016/S0929-6646(08)60189-8. Epub [PubMed PMID: 18926943]
Fischer ER, Hansen BT, Nair V, Hoyt FH, Dorward DW. Scanning electron microscopy. Current protocols in microbiology. 2012 May:Chapter 2():Unit 2B.2.. doi: 10.1002/9780471729259.mc02b02s25. Epub [PubMed PMID: 22549162]
Orlandini SZ, Orlandini GE. Ultrastructure of human male urethra. Archives of andrology. 1989:23(1):51-9 [PubMed PMID: 2675786]
Goldsmith CS, Miller SE. Modern uses of electron microscopy for detection of viruses. Clinical microbiology reviews. 2009 Oct:22(4):552-63. doi: 10.1128/CMR.00027-09. Epub [PubMed PMID: 19822888]
Bono MJ, Leslie SW, Reygaert WC. Uncomplicated Urinary Tract Infections. StatPearls. 2025 Jan:(): [PubMed PMID: 29261874]
Hosseini J, Razi A, Javanmard B, Lotfi B, Mazloomfard MM. Penile Preservation for Male Urethral Cancer. Iranian journal of cancer prevention. 2011 Fall:4(4):199-201 [PubMed PMID: 26322198]