Introduction
The septum pellucidum (meaning translucent wall in Latin - SP), also known as the ventricle of Sylvius, is a thin, triangular double membrane separating the frontal horns of the right and left lateral ventricles of the brain. It extends between the anterior portion of the corpus callosum, and the body of the fornix and its width varies from 1.5 to 3.0 mm
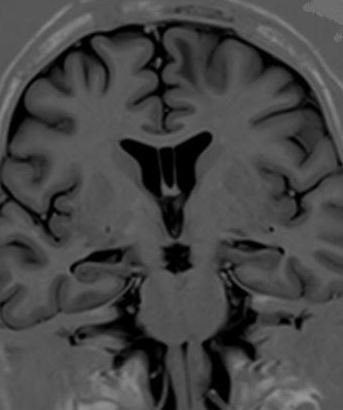
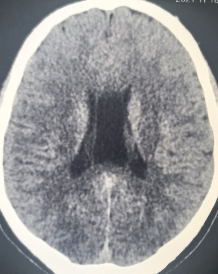
The cavum septum pellucidum (CSP) is a potential cavity between the membranous leaves of the septum pellucidum, separated by at least 1 mm, and is considered a normal anatomical variation (see Images. Cavum Septum Pellucidum). It contains a filtrate of cerebrospinal fluid transferred from the ventricles through the septal laminae, and it does not communicate with the subarachnoid space. Sometimes, it may connect to a more posterior cavity called cavum vergae (CV), but separates from each other by an arbitrary vertical plane formed by the columns of the fornix. CSP and CV were respectively and incorrectly called the fifth and sixth ventricles in the past. Both are not parts of the ventricular system as they have a different embryological origin and lack a lining with ependymal or choroid plexus cells.
Boundaries of SP:
Superiorly - Inferior surface of the body of the corpus callosum
Antero-inferiorly - Superior surface of the genu of the corpus callosum
Posteroinferiorly - Corpus and columns of the fornix
Laterally - Medial wall of frontal horns of lateral ventricles
Medially - Virtual space with the contralateral septum
Boundaries of CSP [1]
Anteriorly - Genu of the corpus callosum
Superiorly - Body of the corpus callosum
Posteriorly - Anterior limb and pillars of the fornix
Inferiorly - Anterior commissure and the rostrum of the corpus callosum and
Laterally - Leaflets of the septum pellucidum.
SP is an important part of the limbic system, with prominent connections to both the medial and the basolateral limbic circuit. Disease affecting the CSP can cause symptoms either by mass effect or by disturbance of the emotional and behavioral functions of the limbic system.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The septum pellucidum is formed embryologically by two closely opposed leaves enclosing a cavity called the CSP. The leaves of SP fuse in a caudal to the rostral direction at approximately six months of intrauterine life. The CSP cavity usually disappears by three months of postnatal life. However, if the gap is not closed, CSP may persist and can be seen even in adults.
Epidemiology
Cavum septum pellucidum is estimated to occur in all premature infants, in 85% of full-term neonates, and 12% of children between 6 months and 16 years old. Eighty-five percent of CSP fuses around 3 to 6 months after birth.[2] In adults, the prevalence varies from 4 to 74%, depending on detection methods and anatomical definition. Cysts of CSP are rarer with an incidence of 0.04%, as found by Wang et al.[3], whereas symptomatic CSP cysts are very rare lesions with only a few cases described in the literature.
Pathophysiology
Cavum septum pellucidum will not cause symptoms. Symptoms are more likely to occur with cavum septum pellucidum cysts though most of them are incidental findings. There are mainly three mechanisms described:
- Ball-valve phenomenon - Obstruction of interventricular foramina by the cyst leading to hydrocephalus and increased intracranial pressure.
- Compression of the hypothalamo-septal triangle (formed by the specific septal, periseptal nuclei, and associated projection pathways) - Leading to neuropsychiatric symptoms and compression of optic chiasm and pathways
- A chronic deep venous impairment - displacement and stretching of the internal cerebral and subependymal veins may cause progressive focal deficits.[4]
The CSP cavity may expand to form a CSP cyst, probably due to an ability to secrete fluid internally. The well-accepted definition of a CSP cyst is a cystic structure having a width of 10 mm or more in the septum's region, the walls of which exhibiting lateral bowing.[5] There is no strict definition differentiating a large CSP from the CSP cyst.
CSP cyst classifies into two categories: communicating and noncommunicating cyst, depending on whether it communicates with the ventricles or not. Noncommunicating cyst may become communicating due to spontaneous rupture or during head trauma, diagnostic procedures (ventriculography and pneumoencephalography), or surgery. The reverse is also possible if fibrosis occurs at the site of communication.
CSP cysts can also classify as symptomatic or asymptomatic.
Histopathology
Cavum septum pellucidum has a lining of glial and neuronal cells.[6] The boxer’s cavum displayed a characteristic fenestration with the detachment of the fornix from the undersurface of the corpus callosum, with the two flattened forniceal bodies splaying out horizontally.[7]
History and Physical
Many symptoms and diseases have historically been attributed to cysts of the CSP - mental disturbances, ataxia, disordered speech, epilepsy, and bilateral pyramidal signs. But these are now being questioned because of a lack of proper evidence.
CSP cysts may also cause acute or chronic headaches, papilledema, emesis, syncope, cognitive impairment, emotional and behavioral disturbances, and visual and sensorimotor findings.
Evaluation
Proper evaluation of cavum septum pellucidum requires magnetic resonance imaging of the brain.
In fetal life, visualization of the CSP between 18 and 20 weeks’ gestation implies normal development of the brain.[8] Its assessment is a mandatory part of second-trimester ultrasound. The absence of CSP is a marker of associated fetal anomalies (listed under complications).
Treatment / Management
Treatment indications for cavum septum pellucidum are the following conditions:
- Association of a CSP cyst on imaging studies and clinical signs and symptoms because of the obstruction of the cerebrospinal fluid flow in the foramen of Monro
- Direct compression of surrounding tissues by the cyst
- Mental status changes or focal neurological deficits attributable to the CSP cyst
The primary goal of treatment is to relieve the mass effect caused by the cyst, and it is only surgical.
The classic treatment in these cases is surgical approaches, including open surgical procedures, conventional shunting, and stereotactic fenestration.
Dandy published the first treated CSP cyst in 1931; he treated a 4.5-year-old boy by a transcallosal fenestration.[9](B3)
Since 1995 when Jacowski et al. described the first endoscopic approach,[10] neuroendoscopic fenestration has become a well-established therapeutic option and currently the treatment of choice for symptomatic CSP cysts.(B3)
Three endoscopic approaches are described:[11](B3)
- A frontal approach on the coronal suture 3 cm from the midline targeting the frontal horn of the lateral ventricle (used by the majority of authors)
- The same cortical frontal approach but directly targeting the cyst that is punctured and then a fenestration of the two walls is performed
- An occipital burr hole to optimize the trajectory into the atrium of the lateral ventricle, which would allow an approach both leaflets of the cyst perpendicularly.
The endoscopic fenestration offers a less invasive approach, direct visualization, and effectiveness. Direct visualization of neural and vascular structures prevents inadvertent injury. It is also important to inspect the foramina of Monro to search potential adhesions, which may play a role in the hydrocephalus to persist after apparently successful drainage of the cyst. Additionally, this technique avoids the need to place a shunt and allows a biopsy of the cyst walls.
The presence of CSP and cavum vergae may affect the choice of route for intracranial endoscopic surgery, with the transcavum interforniceal path preferred over the transforaminal approach into the third ventricle.[6]
Differential Diagnosis
- The cavum vergae extends from the cavum septum pellucidum posterior to the anterior columns of the fornix, lying anterior to the splenium of the corpus callosum (see Image. Cavum Vergae).
- The cavum veli interpositi extends from below the splenium of the corpus callosum and the column of the fornix and above the internal cerebral veins. Its shape is triangular, with the apex pointing anteriorly reaching as far forward as the foramen of Munro
- Vein of Galen aneurysm - Diagnosed by color Doppler technology
- Arachnoid cyst
- Dilated third ventricle (distinguished by its location between the thalami)
Prognosis
Cavum septum pellucidum is usually an incidental diagnosis and typically asymptomatic.
Complications
Enlarged cavum septum pellucidum is seen in the following conditions[12][13][6][14]:
- Schizophrenia patients (First reported by De Greef)
- Aggressive, individuals with an alcohol use disorder
- People with neurological development disorders
- Boxers due to repeated head trauma
- Post-traumatic stress disorder patients
- Military population currently participating in war conflicts or veterans of wars
- Obsessive-compulsive disorders
The absence of the cavum septum pellucidum in fetal life correlates with the following conditions:
- Holoprosencephaly
- Septo-optic dysplasia
- Agenesis of the corpus callosum
- Alexander disease
- Tuberous sclerosis
- Phacomatosis
- Pinealoma
- Trisomy 21
- Schizencephaly
- Lissencephaly
- Chiari malformation
Deterrence and Patient Education
Patients need reassurance that cavum septum pellucidum is a normal anatomical variation and requires no surgical intervention and is unlikely to progress.
Only if the size is >1 cm or if symptomatic, enlarged CSP requires further evaluation and management.
Pearls and Other Issues
Symptomatic enlargement of the cavum septum pellucidum is rare and most commonly causes intermittent obstructive hydrocephalus with headache and loss of consciousness. It is amenable to surgical treatment such as cyst puncture or shunting, ventriculoperitoneal shunting, or radical excision.
CSP is an important marker for the evaluation of normal development of the fetal neural axis.
Enhancing Healthcare Team Outcomes
A rigorous evaluation, neurological and radiological examinations are necessary before treatment. Hence discussions with the radiologist, neurologist, neuropsychiatrist are needed before proceeding with surgery for CSP cysts even though they appear to be symptomatic.
Media
References
Born CM, Meisenzahl EM, Frodl T, Pfluger T, Reiser M, Möller HJ, Leinsinger GL. The septum pellucidum and its variants. An MRI study. European archives of psychiatry and clinical neuroscience. 2004 Oct:254(5):295-302 [PubMed PMID: 15365704]
Farruggia S, Babcock DS. The cavum septi pellucidi: its appearance and incidence with cranial ultrasonography in infancy. Radiology. 1981 Apr:139(1):147-50 [PubMed PMID: 7208915]
Wang KC, Fuh JL, Lirng JF, Huang WC, Wang SJ. Headache profiles in patients with a dilatated cyst of the cavum septi pellucidi. Cephalalgia : an international journal of headache. 2004 Oct:24(10):867-74 [PubMed PMID: 15377318]
Fratzoglou M, Grunert P, Leite dos Santos A, Hwang P, Fries G. Symptomatic cysts of the cavum septi pellucidi and cavum vergae: the role of endoscopic neurosurgery in the treatment of four consecutive cases. Minimally invasive neurosurgery : MIN. 2003 Aug:46(4):243-9 [PubMed PMID: 14506571]
Level 3 (low-level) evidenceSener RN. Cysts of the septum pellucidum. Computerized medical imaging and graphics : the official journal of the Computerized Medical Imaging Society. 1995 Jul-Aug:19(4):357-60 [PubMed PMID: 8653673]
Tubbs RS, Krishnamurthy S, Verma K, Shoja MM, Loukas M, Mortazavi MM, Cohen-Gadol AA. Cavum velum interpositum, cavum septum pellucidum, and cavum vergae: a review. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2011 Nov:27(11):1927-30. doi: 10.1007/s00381-011-1457-2. Epub 2011 Jun 18 [PubMed PMID: 21687999]
Pearce JM. Some observations on the septum pellucidum. European neurology. 2008:59(6):332-4. doi: 10.1159/000121428. Epub 2008 Apr 11 [PubMed PMID: 18408379]
Coleridge-Smith P, Labropoulos N, Partsch H, Myers K, Nicolaides A, Cavezzi A. Duplex ultrasound investigation of the veins in chronic venous disease of the lower limbs--UIP consensus document. Part I. Basic principles. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2006 Jan:31(1):83-92 [PubMed PMID: 16226898]
Level 3 (low-level) evidenceAmin BH. Symptomatic cyst of the septum pellucidum. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 1986:2(6):320-2 [PubMed PMID: 3829032]
Level 3 (low-level) evidenceJackowski A, Kulshresta M, Sgouros S. Laser-assisted flexible endoscopic fenestration of giant cyst of the septum pellucidum. British journal of neurosurgery. 1995:9(4):527-31 [PubMed PMID: 7576280]
Level 3 (low-level) evidenceTamburrini G, Mattogno PP, Narenthiran G, Caldarelli M, Di Rocco C. Cavum septi pellucidi cysts: a survey about clinical indications and surgical management strategies. British journal of neurosurgery. 2017 Aug:31(4):464-467. doi: 10.1080/02688697.2016.1229743. Epub 2016 Sep 13 [PubMed PMID: 27619551]
Level 3 (low-level) evidenceTrzesniak C, Oliveira IR, Kempton MJ, Galvão-de Almeida A, Chagas MH, Ferrari MC, Filho AS, Zuardi AW, Prado DA, Busatto GF, McGuire PK, Hallak JE, Crippa JA. Are cavum septum pellucidum abnormalities more common in schizophrenia spectrum disorders? A systematic review and meta-analysis. Schizophrenia research. 2011 Jan:125(1):1-12. doi: 10.1016/j.schres.2010.09.016. Epub 2010 Oct 20 [PubMed PMID: 20965698]
Level 1 (high-level) evidenceDegreef G, Lantos G, Bogerts B, Ashtari M, Lieberman J. Abnormalities of the septum pellucidum on MR scans in first-episode schizophrenic patients. AJNR. American journal of neuroradiology. 1992 May-Jun:13(3):835-40 [PubMed PMID: 1590179]
Chon MW, Choi JS, Kang DH, Jung MH, Kwon JS. MRI study of the cavum septum pellucidum in obsessive-compulsive disorder. European archives of psychiatry and clinical neuroscience. 2010 Jun:260(4):337-43. doi: 10.1007/s00406-009-0081-6. Epub 2009 Oct 25 [PubMed PMID: 19856198]
Level 2 (mid-level) evidence