Introduction
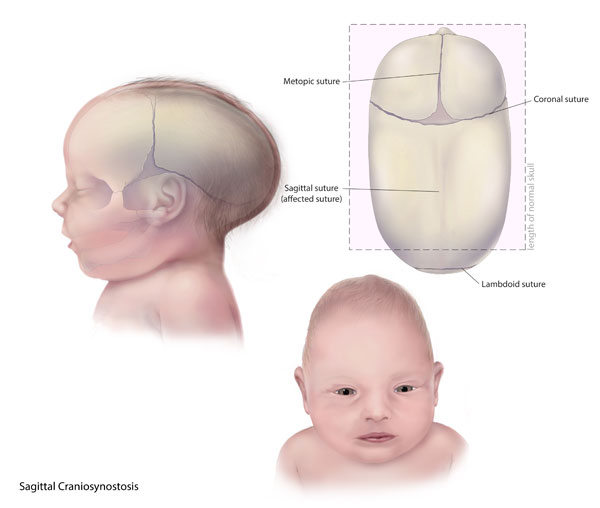
Scaphocephaly is the term used to describe the narrow and long abnormal skull shape in sagittal craniosynostosis due to the premature fusion of the sagittal suture forming an osseous ridge.[1] The head shape is described as a "boat-shaped" head, which is called dolichocephaly. It is the most common type of craniosynostosis. It is essential to make an early diagnosis since a delay may lead to abnormal growth of the cranial vault and affect brain growth and development.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The cause of scaphocephaly is the premature closure of all or most of the sagittal suture. Physiologic sagittal suture closure starts at 22 years of age. Sometimes, a complete fusion may not occur; however, most individuals have it closed between 30 and 50 years old. The specific etiology of craniosynostosis, especially the nonsyndromic type of craniosynostosis, is still not completely understood, but most cases are sporadic. Many factors have been studied and implicated, and these include genetic mutations, metabolic and hematologic syndromes, teratogens (i.e., valproic acid), maternal smoking, and advanced paternal age.
A combination of external factors and genetic mutations is implicated in this condition's etiology. There have been more than 100 mutations associated with nonsyndromic craniosynostosis. The most common and most studied mutation is the fibroblast growth factors (FGFR) gene 1-3.[2] In sagittal craniosynostosis, the most common mutation is in the SMAD6 gene.[3] Other mutations associated are in the TWIST1, TCF12, ERF, MSX2 genes.[3][4][5][6] However, only in a few cases, mutations are identified.[2][7]
Epidemiology
The incidence of craniosynostosis is approximately 1 in 200 to 2500 live births. Single suture involvement is most commonly seen. Craniosynostosis is most frequently seen in the child of a non-Hispanic white. Sagittal craniosynostosis is the most common of all the craniosynostosis. It represents about 53% to 60% of all craniosynostosis. It affects males predominantly, approximately 80%, with a male-to-female ratio of 3.5 to 1.[7] Hispanic ethnicity and non-Hispanic black race are associated with a lower prevalence of craniosynostosis.[8]
Pathophysiology
When the sagittal suture prematurely ossifies, the skull's growth proceeds parallel to the future, and the growth perpendicular to the suture terminates. Thus, when the sagittal suture closes, the head keeps growing in the anteroposterior direction producing an elongated head shape. This is recognized as Virchow’s law.[9][10] In premature single suture fusion, elevated intracranial pressure occurs in approximately 11% of cases. In sagittal craniosynostosis, this can be as high as 44%.[11]
Alterations in the expression of growth factors have been implicated in the pathophysiology of craniosynostosis. Various mutations have been identified in craniosynostosis, including three fibroblast growth factors and other genes such as the twisted family basic helix-loop-helix transcription factor TWIST 1.[4][5][12][13][14] They are more frequently found in syndromic craniosynostosis.[15] In sagittal craniosynostosis, approximately 10% of the patients show genetic alterations.[14]
History and Physical
The parents usually complain that the baby’s head doesn’t look right. Frequently they noted that the deformity continues to worsen as the child’s head continues to grow. Parents are asked for a history of prior cases of craniosynostosis.
Clinical observation is essential. A physical examination will show the elongated head and a palpable bone ridge at the head's vertex. Head measurement shows an increased anteroposterior dimension. The bilateral dimension is shortened, producing biparietal and bitemporal narrowing. Prominent frontal and occipital bossing can be observed. The cephalic index is calculated by measuring the biparietal diameter and the occipitofrontal diameter and obtaining the ratio. The typical average index is approximately 80-83. In scaphocephaly, the index is reduced as the occipitofrontal diameter is larger. There are no visible abnormalities of the cranial base, orbits, or face in nonsyndromic sagittal craniosynostosis.
The baby is evaluated for respiratory difficulty. In severe cases, the head is abnormally flexed when lying supine causing airway compromise. An ophthalmologic examination should be obtained to assess for papilledema, indicating an increased intracranial pressure.[16]
Evaluation
Manual palpation of a bony prominence over the sagittal suture will aid in the initial diagnosis. The radiological finding of the absence of the sagittal suture or a bony ridge across part of the suture confirms the diagnosis.
Ultrasonography can be used to detect the fused suture and avoid radiation to the patient.[17][18][19][20][21][22]
Plain skull X-rays can also show the fused suture; however, the study of choice is the head computed tomographic (CT) scan with 3D reconstruction.[23][24][25][26][27][28] The CT scan will also show other bone anomalies or hydrocephalus. However, some authors do not recommend the 3D CT scan in single sagittal craniosynostosis.[29][30] Magnetic resonance imaging (MRI) is not necessary except in syndromic cases to evaluate in detail the brain. Black box MRI offers an alternative to CT scan, avoiding radiation in patients with craniosynostosis.[31][32][33]
In patients with rare skeletal metabolic disorders and suspected craniosynostosis, it is essential to screen them at the time of diagnosis and follow-up.[34]
Treatment / Management
Treatment of sagittal craniosynostosis is usually surgical to correct head shape and prevent psychological effects on the parents and patient. In most cases, surgery involves the removal of the affected suture. The width of the craniectomy has to be at least 3 cm. The surgery is preferably done within the first 3–6 months of life. If surgery is performed after 12 months of age, more bone removal and remodeling is required. If surgical intervention is not performed early, suboptimal outcomes can result from the thickened skull and slowed brain growth. Control of bleeding is one of the essentials during the surgery. Preoperative prophylactic antibiotics are used. An adequate initial correction of the skull deformity protects the patient from the additional surgical risk by making a reoperation less likely. Surgery can be performed open or endoscopically. Endoscopic surgery has the advantage of reducing blood loss; however, a helmet is usually required for several months. The optimal duration of helmet use is around 7 to 9 months after surgery.[35][36]
Endoscopic surgery (strip craniectomy): Patients are usually placed in a modified prone position with the cervical spine extended. The modified prone position allows access to the frontal and occipital areas. The procedure incorporates two incisions on the midline. The initial incision is done 2-3 cm behind the anterior fontanelle, and the second incision is done anterior to the lambda. The pericranium is preserved. A subgaleal plane from the anterior fontanelle to the lambda of about 3 cm is done bilaterally. A burr hole at the edge of each incision is made. The dura is separated and then cut with Mayo scissors in a triangular shape towards the anterior fontanelle. A second posterior osteotomy is made at the lambda similarly. An endoscope is inserted and advanced posteriorly toward the lambda. Once the dura has been freed from the overlying bone, bone-cutting or Mayo scissors are used to make lateral osteotomies and remove the fused suture. Barrel stave, wedge osteotomies are created with scissors after the dura is freed from the bone directly behind the coronal suture and then directly in front of the lambdoid sutures. No direct cauterization of the dura is performed to allow bone growth from the osteogenic cells.[37][38][39][40][41](B2)
Open surgery (cranial vault remodeling): Milder cases can be successfully treated with the removal of the fused sagittal suture. In more severe cases, a complete reshaping of the skull may be necessary. Patients with complete sagittal synostosis frequently have deformities in the anterior and posterior skull, which need to be addressed. Treatment is directed at the most salient deformity. After the bicoronal zigzag or sawtooth-shaped scalp flap is completed, exposure of the individual sutures is done. Each suture is removed separately. If the sutures are not removed, they will prevent the reshaping process and will maintain the deformity. Removal of the sagittal suture usually results in spontaneous widening of the entire skull as the restraining force is removed. The sagittal bone strip is reduced in length. Several barrel stave lateral osteotomies are made down to the level of the squamosal suture. The removed sutures are floated over the dura. If used, bone grafts are fixed with absorbable plate and screw fixation to fill the bone gaps. If there is significant frontal bossing, the frontal bone is removed and remolded. Radial barrel stave osteotomies are made, and the bone is flattened to correct the abnormal curvature. The frontal bone is then fixed with absorbable plates and screw fixation. If there is posterior bossing, a similar procedure in the occipital bone using radial barrel stave osteotomies is performed.[37] A suction drain can be placed to reduce the subgaleal blood collection, and a firm head dressing is applied. The patient is monitored overnight at the pediatric intensive care unit. The use of tranexamic acid reduces the need for multiple blood transfusions.[42][43][44][45]
Spring-assisted surgery: Uses a strip craniectomy, and indwelling springs aid in the cranial vault expansion.[46][47][48] This technique offers similar cosmetic results with less operative time and blood loss.[47][49] However, a second surgery is required for spring removal. Spring-assisted surgery had shorter operative time, shorter length of hospital stay, and less blood loss than open strip craniectomy with parietal barrel staving.[49][50] (B2)
Studies have shown that the principal differences between the endoscopic approach and the open approach include shorter surgical time, shorter pediatric intensive care unit length of stay, less intraoperative blood loss, and fewer blood transfusions in the endoscopic approach.[51][52](B2)
Differential Diagnosis
Non-syndromic craniosynostosis has to be differentiated from other sources that cause secondary synostosis.[34][53][54]
- Hyperthyroidism
- Hypercalcemia
- Renal osteodystrophy
- Hypophosphatemia
- Vitamin D deficiency
- Sickle cell anemia
- Thalassemia
- Polycythemia vera
- Microcephaly
- Prematurity
- Shunted hydrocephalus
- Sly syndrome
- Morquio syndrome
- Hurler's syndrome
- Beta-glucuronidase deficiency
- Mucopolysaccharidosis
- Mucolipidosis III
- X-linked hypophosphatemia
- 1-alpha hydroxylase deficiency
- Teratogens (phenytoin, valproic acid, retinoic acid, aminopterin)
- Pseudohypoparathyroidism
- Osteopetrosis
The single suture craniosynostosis has to be differentiated from syndromic craniosynostosis. Most syndromic craniosynostosis involves the coronal suture producing brachycephaly.[53]
- Apert syndrome
- Crouzon syndrome
- Muenke syndrome
- Pfeiffer syndrome
- Saether Chotzen syndrome
- Craniofrontonasal syndrome
- Carpenter syndrome
Prognosis
After surgery, the head will remodel and obtain a rounder shape that, in most cases, is satisfactory.[55] The endoscopic approach and the open approach are both effective in correcting sagittal craniosynostosis deformities.[51][52][56][16] A systematic review showed insufficient information to suggest that any treatment had greater cosmetic improvement over the other.[56] The cephalic index correction in strip craniectomy is less than in cranial vault reconstruction but not cosmetically significant.[57][58] Some surgeons recommended overcorrection to compensate for the reduced postoperative cranial growth.[59][60]
Long-term studies have shown that patients with sagittal craniosynostosis and other nonsyndromic craniosynostosis present difficulties in cognitive, language, and motor domains with mild neuropsychological deficits in infancy and childhood.[61][62] A study showed reading and/or spelling disability in up to 50% of the patients.[63] Sagittal craniosynostosis patients show that 39% of them have cognitive and speech problems. However, patients with sagittal craniosynostosis are less likely to have cognitive and speech problems than any other craniosynostosis type.[64]
Patients with sagittal craniosynostosis have a normal range for intelligence but showed a higher incidence of learning disabilities.[56][63][65] Patients have a higher verbal IQ than the performance IQ, which can suggest finer problems in achievement.[65] One study found no increase in cognitive impairment.[66] A systematic review showed that operated patients for sagittal craniosynostosis have an increased risk of developing learning disorders, but there is insufficient evidence comparing procedures regarding cognitive and neurological outcomes.[56]
Complications
Several complications may occur from surgical correction of the craniosynostosis:[37][67][68][69]
- Cerebrospinal fluid leak
- Dural tears
- Excessive blood loss
- Consumption coagulopathy
- Hypoactivity
- Hyperthermia
- Wound infection local
- Epidural abscess
- Subcutaneous hematoma
- Epidural hematoma
- Venous air embolism
- Inadequate correction
- Reoperation
- Scalp erosion
- Scalp ulcer
Postoperative and Rehabilitation Care
The patient is admitted to the pediatric intensive care unit for at least 24 hours. Then initial nursing care focuses on evaluating the neurologic status, fluid and electrolyte balance, and pain management. The hematocrit level is closely monitored, and blood transfusions are given if indicated. Pain control is maintained with alternating acetaminophen and ibuprofen and intermittent intravenous morphine as needed. Prophylactic antibiotics may be continued for 24 hours postoperatively. The child is evaluated for adequate hemostasis and signs of infection. Postoperative scalp swelling can be uncomfortable and can be reduced by elevating the head of the bed. The child is usually transferred to the general pediatric floor on the first or second postoperative day. The face and scalp swelling will resolve over 1 to 2 weeks.
Preoperative and postoperative photographs are taken to serve for outcome assessment. Follow-up for at least five years is ideal for assessing the progressive skull reshaping. Evaluation of the skull reshaping pattern and the child's age will guide the timing for revisional surgery. In children older than 1-2 years, defects >2 cm diameter usually require calvarial split bone grafts or bone substitutes to fill the cranial defects and prevent permanent defects.
Consultations
The following consultations are required:
- Pediatric neurosurgeon
- Craniofacial surgeon
- Plastic surgeon
- Pediatric intensivist
- Geneticist
Deterrence and Patient Education
The diagnosis and treatment of craniosynostosis can produce a significant impact on families.[70] Careful explanation of the diagnosis, treatment modalities, postoperative care, and prognosis can help families deal with the initial struggle after the diagnosis is made. The entire family, including grandparents, are offered the occasion to meet with the surgical team to discuss any concerns with the surgical experience, which will impact all of them.
In non-syndromic cases of sagittal craniosynostosis, it is recommended to perform screening for SMAD6 mutations, and if present, genetic counseling is given to the parents.[3] If there is no family history for craniosynostoses and no genetic mutations are found, there is a 5% recurrence risk to offsprings for nonsyndromic sagittal craniosynostosis.[71]
Patients who have increased intracranial pressure due to craniosynostosis may not present with typical hydrocephalus symptoms but may develop signs such as papilledema, skull deformities, developmental delay, and developmental milestones underachievement.
Enhancing Healthcare Team Outcomes
An interprofessional team of healthcare professionals includes a pediatric neurosurgeon, craniofacial surgeon, plastic surgeon, psychologists, geneticists, and a pediatric intensivist to work together to obtain the best possible outcomes. It is essential to educate parents about diagnosis, prognosis, complications, potential treatment options, and follow-up. It is important to differentiate between patients and individualize the treatment selection concerning age, weight, degree of deformity, and associated symptoms. Every patient is different, and making the proper selection to obtain the best possible outcome is essential. The identification of genetic mutations is necessary for prognosis and parental counseling. Nursing roles include direct patient care, physician-family liaison, and family educator.
Media
(Click Image to Enlarge)
References
Dempsey RF,Monson LA,Maricevich RS,Truong TA,Olarunnipa S,Lam SK,Dauser RC,Hollier LH Jr,Buchanan EP, Nonsyndromic Craniosynostosis. Clinics in plastic surgery. 2019 Apr; [PubMed PMID: 30851746]
Ye X,Guilmatre A,Reva B,Peter I,Heuzé Y,Richtsmeier JT,Fox DJ,Goedken RJ,Jabs EW,Romitti PA, Mutation Screening of Candidate Genes in Patients with Nonsyndromic Sagittal Craniosynostosis. Plastic and reconstructive surgery. 2016 Mar; [PubMed PMID: 26910679]
Timberlake AT,Persing JA, Genetics of Nonsyndromic Craniosynostosis. Plastic and reconstructive surgery. 2018 Jun; [PubMed PMID: 29579021]
Wilkie AO, Craniosynostosis: genes and mechanisms. Human molecular genetics. 1997; [PubMed PMID: 9300656]
Level 3 (low-level) evidenceJohnson D, A comprehensive screen of genes implicated in craniosynostosis. Annals of the Royal College of Surgeons of England. 2003 Nov; [PubMed PMID: 14629875]
Lajeunie E,Catala M,Renier D, Craniosynostosis: from a clinical description to an understanding of bone formation of the skull. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 1999 Nov; [PubMed PMID: 10603009]
Level 3 (low-level) evidenceLajeunie E,Le Merrer M,Bonaïti-Pellie C,Marchac D,Renier D, Genetic study of scaphocephaly. American journal of medical genetics. 1996 Mar 29; [PubMed PMID: 8882788]
Schraw JM,Woodhouse JP,Langlois PH,Canfield MA,Scheuerle AE,Agopian AJ,Benjamin RH,Lupo PJ, Risk factors and time trends for isolated craniosynostosis. Birth defects research. 2020 Oct 22; [PubMed PMID: 33091229]
Delashaw JB,Persing JA,Broaddus WC,Jane JA, Cranial vault growth in craniosynostosis. Journal of neurosurgery. 1989 Feb; [PubMed PMID: 2913214]
Delashaw JB,Persing JA,Jane JA, Cranial deformation in craniosynostosis. A new explanation. Neurosurgery clinics of North America. 1991 Jul; [PubMed PMID: 1821307]
Level 3 (low-level) evidenceWall SA,Thomas GP,Johnson D,Byren JC,Jayamohan J,Magdum SA,McAuley DJ,Richards PG, The preoperative incidence of raised intracranial pressure in nonsyndromic sagittal craniosynostosis is underestimated in the literature. Journal of neurosurgery. Pediatrics. 2014 Dec; [PubMed PMID: 25259602]
Level 2 (mid-level) evidenceKutkowska-Kaźmierczak A,Gos M,Obersztyn E, Craniosynostosis as a clinical and diagnostic problem: molecular pathology and genetic counseling. Journal of applied genetics. 2018 May; [PubMed PMID: 29392564]
Roscioli T,Elakis G,Cox TC,Moon DJ,Venselaar H,Turner AM,Le T,Hackett E,Haan E,Colley A,Mowat D,Worgan L,Kirk EP,Sachdev R,Thompson E,Gabbett M,McGaughran J,Gibson K,Gattas M,Freckmann ML,Dixon J,Hoefsloot L,Field M,Hackett A,Kamien B,Edwards M,Adès LC,Collins FA,Wilson MJ,Savarirayan R,Tan TY,Amor DJ,McGillivray G,White SM,Glass IA,David DJ,Anderson PJ,Gianoutsos M,Buckley MF, Genotype and clinical care correlations in craniosynostosis: findings from a cohort of 630 Australian and New Zealand patients. American journal of medical genetics. Part C, Seminars in medical genetics. 2013 Nov; [PubMed PMID: 24127277]
Armand T,Schaefer E,Di Rocco F,Edery P,Collet C,Rossi M, Genetic bases of craniosynostoses: An update. Neuro-Chirurgie. 2019 Nov; [PubMed PMID: 31605683]
Kimonis V,Gold JA,Hoffman TL,Panchal J,Boyadjiev SA, Genetics of craniosynostosis. Seminars in pediatric neurology. 2007 Sep; [PubMed PMID: 17980312]
Al-Shaqsi SZ,Lam NW,Forrest CR,Phillips JH, Endoscopic Versus Open Total Vault Reconstruction of Sagittal Craniosynostosis. The Journal of craniofacial surgery. 2020 Dec 3; [PubMed PMID: 33278249]
Proisy M,Bruneau B,Riffaud L, How ultrasonography can contribute to diagnosis of craniosynostosis. Neuro-Chirurgie. 2019 Nov; [PubMed PMID: 31586456]
Constantine S,Kiermeier A,Anderson P, Sonographic indicators of isolated fetal sagittal craniosynostosis during pregnancy. Journal of medical imaging and radiation oncology. 2020 Oct; [PubMed PMID: 32530572]
Miller C,Losken HW,Towbin R,Bowen A,Mooney MP,Towbin A,Faix RS, Ultrasound diagnosis of craniosynostosis. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association. 2002 Jan; [PubMed PMID: 11772173]
Level 2 (mid-level) evidencePogliani L,Zuccotti GV,Furlanetto M,Giudici V,Erbetta A,Chiapparini L,Valentini L, Cranial ultrasound is a reliable first step imaging in children with suspected craniosynostosis. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2017 Sep; [PubMed PMID: 28578511]
Hall KM,Besachio DA,Moore MD,Mora AJ,Carter WR, Effectiveness of screening for craniosynostosis with ultrasound: a retrospective review. Pediatric radiology. 2017 May; [PubMed PMID: 28213626]
Level 2 (mid-level) evidenceProisy M,Riffaud L,Chouklati K,Tréguier C,Bruneau B, Ultrasonography for the diagnosis of craniosynostosis. European journal of radiology. 2017 May; [PubMed PMID: 28583642]
Parisi M,Mehdizadeh HM,Hunter JC,Finch IJ, Evaluation of craniosynostosis with three-dimensional CT imaging. Journal of computer assisted tomography. 1989 Nov-Dec; [PubMed PMID: 2584477]
Craven CM,Naik KS,Blanshard KS,Batchelor AG,Spencer JA, Multispiral three-dimensional computed tomography in the investigation of craniosynostosis: technique optimization. The British journal of radiology. 1995 Jul; [PubMed PMID: 7640927]
Medina LS, Three-dimensional CT maximum intensity projections of the calvaria: a new approach for diagnosis of craniosynostosis and fractures. AJNR. American journal of neuroradiology. 2000 Nov-Dec; [PubMed PMID: 11110553]
Shen WM,Gao F,Wang G,Cui J,Chen JB, [3-Dimensional CT for preoperative measurement and postoperative assessment in craniosynostosis]. Zhonghua zheng xing wai ke za zhi = Zhonghua zhengxing waike zazhi = Chinese journal of plastic surgery. 2008 Sep; [PubMed PMID: 19119635]
Montoya JC,Eckel LJ,DeLone DR,Kotsenas AL,Diehn FE,Yu L,Bartley AC,Carter RE,McCollough CH,Fletcher JG, Low-Dose CT for Craniosynostosis: Preserving Diagnostic Benefit with Substantial Radiation Dose Reduction. AJNR. American journal of neuroradiology. 2017 Apr; [PubMed PMID: 28183836]
Ginat DT,Lam D,Kuhn AS,Reid R, CT Imaging Findings after Craniosynostosis Reconstructive Surgery. Pediatric neurosurgery. 2018; [PubMed PMID: 29874675]
Schweitzer T,Böhm H,Meyer-Marcotty P,Collmann H,Ernestus RI,Krauß J, Avoiding CT scans in children with single-suture craniosynostosis. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2012 Jul; [PubMed PMID: 22349960]
Cerovac S,Neil-Dwyer JG,Rich P,Jones BM,Hayward RD, Are routine preoperative CT scans necessary in the management of single suture craniosynostosis? British journal of neurosurgery. 2002 Aug; [PubMed PMID: 12389887]
Level 2 (mid-level) evidenceSaarikko A,Mellanen E,Kuusela L,Leikola J,Karppinen A,Autti T,Virtanen P,Brandstack N, Comparison of Black Bone MRI and 3D-CT in the preoperative evaluation of patients with craniosynostosis. Journal of plastic, reconstructive [PubMed PMID: 31917189]
Eley KA,Watt-Smith SR,Sheerin F,Golding SJ, [PubMed PMID: 25038852]
Level 2 (mid-level) evidenceTan AP, MRI Protocol for Craniosynostosis: Replacing Ionizing Radiation-Based CT. AJR. American journal of roentgenology. 2019 Dec; [PubMed PMID: 31532254]
Di Rocco F,Rothenbuhler A,Cormier Daire V,Bacchetta J,Adamsbaum C,Baujat G,Rossi M,Lingart A, Craniosynostosis and metabolic bone disorder. A review. Neuro-Chirurgie. 2019 Nov; [PubMed PMID: 31562881]
Iyer RR,Ye X,Jin Q,Lu Y,Liyanage L,Ahn ES, Optimal duration of postoperative helmet therapy following endoscopic strip craniectomy for sagittal craniosynostosis. Journal of neurosurgery. Pediatrics. 2018 Dec 1; [PubMed PMID: 30168732]
Ridgway EB,Berry-Candelario J,Grondin RT,Rogers GF,Proctor MR, The management of sagittal synostosis using endoscopic suturectomy and postoperative helmet therapy. Journal of neurosurgery. Pediatrics. 2011 Jun; [PubMed PMID: 21631199]
Panchal J,Uttchin V, Management of craniosynostosis. Plastic and reconstructive surgery. 2003 May; [PubMed PMID: 12711969]
Jimenez DF,Barone CM, Endoscopic craniectomy for early surgical correction of sagittal craniosynostosis. Journal of neurosurgery. 1998 Jan; [PubMed PMID: 9420076]
Jimenez DF,Barone CM,McGee ME,Cartwright CC,Baker CL, Endoscopy-assisted wide-vertex craniectomy, barrel stave osteotomies, and postoperative helmet molding therapy in the management of sagittal suture craniosynostosis. Journal of neurosurgery. 2004 May; [PubMed PMID: 15287447]
Jimenez DF,Barone CM, Endoscopy-assisted wide-vertex craniectomy, [PubMed PMID: 16833253]
Jimenez DF,Barone CM, Endoscopic technique for sagittal synostosis. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2012 Sep; [PubMed PMID: 22872245]
Level 2 (mid-level) evidenceOngun EA,Dursun O,Kazan MS, Tranexamic Acid Utilization in Craniosynostosis Surgery. Turkish neurosurgery. 2020; [PubMed PMID: 32020570]
Martin DT,Gries H,Esmonde N,Diggs B,Koh J,Selden NR,Schreiber M,Kuang AA, Implementation of a Tranexamic Acid Protocol to Reduce Blood Loss During Cranial Vault Remodeling for Craniosynostosis. The Journal of craniofacial surgery. 2016 Sep; [PubMed PMID: 27557459]
Eustache G,Riffaud L, Reducing blood loss in pediatric craniosynostosis surgery by use of tranexamic acid. Neuro-Chirurgie. 2019 Nov; [PubMed PMID: 31586574]
Song G,Yang P,Zhu S,Luo E,Feng G,Hu J,Li J,Li Y, Tranexamic Acid reducing blood transfusion in children undergoing craniosynostosis surgery. The Journal of craniofacial surgery. 2013 Jan; [PubMed PMID: 23348305]
David LR,Plikaitis CM,Couture D,Glazier SS,Argenta LC, Outcome analysis of our first 75 spring-assisted surgeries for scaphocephaly. The Journal of craniofacial surgery. 2010 Jan; [PubMed PMID: 20061981]
Runyan CM,Gabrick KS,Park JG,Massary D,Hemal K,Owens ES,Thompson JT 2nd,Couture D,David LR, Long-Term Outcomes of Spring-Assisted Surgery for Sagittal Craniosynostosis. Plastic and reconstructive surgery. 2020 Oct; [PubMed PMID: 32590513]
Lauritzen C,Sugawara Y,Kocabalkan O,Olsson R, Spring mediated dynamic craniofacial reshaping. Case report. Scandinavian journal of plastic and reconstructive surgery and hand surgery. 1998 Sep; [PubMed PMID: 9785439]
Level 3 (low-level) evidenceWindh P,Davis C,Sanger C,Sahlin P,Lauritzen C, Spring-assisted cranioplasty vs pi-plasty for sagittal synostosis--a long term follow-up study. The Journal of craniofacial surgery. 2008 Jan; [PubMed PMID: 18216666]
Level 2 (mid-level) evidenceTaylor JA,Maugans TA, Comparison of spring-mediated cranioplasty to minimally invasive strip craniectomy and barrel staving for early treatment of sagittal craniosynostosis. The Journal of craniofacial surgery. 2011 Jul; [PubMed PMID: 21772211]
Level 2 (mid-level) evidenceMelin AA, Moffitt J, Hopkins DC, Shah MN, Fletcher SA, Sandberg DI, Teichgraeber JF, Greives MR. Is Less Actually More? An Evaluation of Surgical Outcomes Between Endoscopic Suturectomy and Open Cranial Vault Remodeling for Craniosynostosis. The Journal of craniofacial surgery. 2020 Jun:31(4):924-926. doi: 10.1097/SCS.0000000000006152. Epub [PubMed PMID: 32049919]
Isaac KV,Meara JG,Proctor MR, Analysis of clinical outcomes for treatment of sagittal craniosynostosis: a comparison of endoscopic suturectomy and cranial vault remodeling. Journal of neurosurgery. Pediatrics. 2018 Nov 1; [PubMed PMID: 30074449]
Level 2 (mid-level) evidenceMathijssen IM, Guideline for Care of Patients With the Diagnoses of Craniosynostosis: Working Group on Craniosynostosis. The Journal of craniofacial surgery. 2015 Sep; [PubMed PMID: 26355968]
Huang MH,Mouradian WE,Cohen SR,Gruss JS, The differential diagnosis of abnormal head shapes: separating craniosynostosis from positional deformities and normal variants. The Cleft palate-craniofacial journal : official publication of the American Cleft Palate-Craniofacial Association. 1998 May; [PubMed PMID: 9603553]
Wang J,Yan Q,He J,Gao Z,Qiu D,Zheng L,Zhang X,Qian J,Wang G, Total Cranial Reconstruction for the Treatment of Sagittal Craniosynostosis in Chinese Children. The Journal of craniofacial surgery. 2020 Sep 3; [PubMed PMID: 32890147]
Level 2 (mid-level) evidenceThwin M,Schultz TJ,Anderson PJ, Morphological, functional and neurological outcomes of craniectomy versus cranial vault remodeling for isolated nonsyndromic synostosis of the sagittal suture: a systematic review. JBI database of systematic reviews and implementation reports. 2015 Sep; [PubMed PMID: 26470674]
Level 1 (high-level) evidenceDe Praeter M,Nadjmi N,Reith FCM,Vercruysse H,Menovsky T, Is There an Advantage to Minimizing Surgery in Scaphocephaly? A Study on Extended Strip Craniectomy Versus Extensive Cranial Vault Remodeling. The Journal of craniofacial surgery. 2019 Sep; [PubMed PMID: 31022147]
Gerety PA,Basta MN,Fischer JP,Taylor JA, Operative Management of Nonsyndromic Sagittal Synostosis: A Head-to-Head Meta-analysis of Outcomes Comparing 3 Techniques. The Journal of craniofacial surgery. 2015 Jun; [PubMed PMID: 26080168]
Level 1 (high-level) evidenceFearon JA,McLaughlin EB,Kolar JC, Sagittal craniosynostosis: surgical outcomes and long-term growth. Plastic and reconstructive surgery. 2006 Feb; [PubMed PMID: 16462336]
Level 2 (mid-level) evidenceFearon JA,Ruotolo RA,Kolar JC, Single sutural craniosynostoses: surgical outcomes and long-term growth. Plastic and reconstructive surgery. 2009 Feb; [PubMed PMID: 19182624]
Level 2 (mid-level) evidenceKapp-Simon KA,Speltz ML,Cunningham ML,Patel PK,Tomita T, Neurodevelopment of children with single suture craniosynostosis: a review. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2007 Mar; [PubMed PMID: 17186250]
Knight SJ,Anderson VA,Spencer-Smith MM,Da Costa AC, Neurodevelopmental outcomes in infants and children with single-suture craniosynostosis: a systematic review. Developmental neuropsychology. 2014; [PubMed PMID: 24742309]
Level 1 (high-level) evidenceMagge SN,Westerveld M,Pruzinsky T,Persing JA, Long-term neuropsychological effects of sagittal craniosynostosis on child development. The Journal of craniofacial surgery. 2002 Jan; [PubMed PMID: 11887004]
Becker DB,Petersen JD,Kane AA,Cradock MM,Pilgram TK,Marsh JL, Speech, cognitive, and behavioral outcomes in nonsyndromic craniosynostosis. Plastic and reconstructive surgery. 2005 Aug; [PubMed PMID: 16079664]
Level 2 (mid-level) evidenceBellew M, Chumas P. Long-term developmental follow-up in children with nonsyndromic craniosynostosis. Journal of neurosurgery. Pediatrics. 2015 Oct:16(4):445-51. doi: 10.3171/2015.3.PEDS14567. Epub 2015 Jul 24 [PubMed PMID: 26207667]
Shipster C,Hearst D,Somerville A,Stackhouse J,Hayward R,Wade A, Speech, language, and cognitive development in children with isolated sagittal synostosis. Developmental medicine and child neurology. 2003 Jan; [PubMed PMID: 12549753]
Lee HQ,Hutson JM,Wray AC,Lo PA,Chong DK,Holmes AD,Greensmith AL, Analysis of morbidity and mortality in surgical management of craniosynostosis. The Journal of craniofacial surgery. 2012 Sep; [PubMed PMID: 22948658]
Level 2 (mid-level) evidenceNoto M,Imai K,Masuoka T,Sakahara D,Kunihiro N, Retrospective Review and Analysis of Complications Due to Cranial Distraction for Craniosynostosis. The Journal of craniofacial surgery. 2020 Nov 4; [PubMed PMID: 33156168]
Level 2 (mid-level) evidencePearson GD,Havlik RJ,Eppley B,Nykiel M,Sadove AM, Craniosynostosis: a single institution's outcome assessment from surgical reconstruction. The Journal of craniofacial surgery. 2008 Jan; [PubMed PMID: 18216667]
Level 2 (mid-level) evidenceKuta V,Curry L,McNeely D,Walling S,Chorney J,Bezuhly M, Understanding families' experiences following a diagnosis of non-syndromic craniosynostosis: a qualitative study. BMJ open. 2020 Sep 24; [PubMed PMID: 32973048]
Level 2 (mid-level) evidenceJohnson D,Wilkie AO, Craniosynostosis. European journal of human genetics : EJHG. 2011 Apr; [PubMed PMID: 21248745]