Introduction
As individuals age, facial structures undergo noticeable changes such as the descent and atrophy of the malar fat pad, deepening of nasolabial folds (NLF), loss of skin elasticity, and jowl development.[1][2] A spectrum of rejuvenation techniques exist that encompass surgical and nonsurgical approaches. Nonsurgical methods involve botulinum toxin, dermal fillers, skin resurfacing with lasers, dermabrasion, or chemical peels, and other adjuncts such as cryotherapy and radiofrequency energy application. Surgical options include fat transfer, brow lifting, eyelid blepharoplasty, cervicofacial rhytidectomy, and midface lifting.[3][4][5] Midface lifting can be achieved by a deep plane facelift as an addition to a superficial muscular aponeurotic system flap rhytidectomy or with a minimal access cranial suspension facelift. A midface lift can also be accomplished through a subciliary incision or with carefully placed incisions in the temporal hair tuft and gingivolabial sulcus. The chosen approach should align with the patient's specific rejuvenation objectives.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
A profound grasp of facial fascial planes is imperative for ensuring the safety and efficacy of any facelift surgery. These layers consist of the skin, subcutaneous fat, superficial muscular aponeurotic system (SMAS), parotidomasseteric fascia, and parotid gland (going from superficial to deep in the lateral cheek) (see Image. Fascial Planes of the Face).[6] Medially, extending beyond the anterior border of the parotid gland, the SMAS seamlessly connects with the mimetic muscles of the face, including the zygomaticus muscles, buccinator, risorius, and others (see Image. Muscular and Fibrous Structures of the Head, Face, and Neck). Superior to the zygomatic arch, the SMAS transforms into the temporoparietal fascia (TPF), while inferiorly, overlaying the mandibular body, it integrates with the platysma.[7] The facial nerve traverses beneath the SMAS layer and its adjacent fasciae (TPF, mimetic muscles, and platysma). Consequently, dissecting the superficial surface of this layer aids in averting iatrogenic nerve injuries. Dr. Ivo Pitanguy's 1966 delineation approximates the course of the frontal branch of the facial nerve, forming a line extending from 0.5 cm below the tragus diagonally to 1.5 cm above the lateral brow. However, separate rami of the frontal branch may traverse the zygomatic arch at various points within its central one-third to one-half.[8][9] Similarly, the Zuker point, situated midway along a line between the root of the helix and the oral commissure, reliably marks the location of the primary buccal branch controlling the zygomatic muscles.[10] Notably, the transverse facial vessels, branches of the superficial temporal vessels, and the parotid duct often share the same plane, just inferior to this nerve branch.
Achieving successful surgery involves preventing complications and realizing the patient's aesthetic objectives. In midface lifts, the primary goals typically involve smoothing NLFs and restoring youthful malar volume. NLFs result from the close juxtaposition of mimetic muscles to the dermis without intervening fat, akin to the anatomical configuration of the levator aponeurosis in the upper eyelid. A successful midface rejuvenation strategy entails repositioning and replenishing volume in the malar fat pads above the dermal attachments of perioral mimetic muscles. This approach targets the root causes, particularly facial fat atrophy linked to aging, rather than solely filling nasolabial folds with hyaluronic acid or fat.[1] Beyond the malar fat pads, the medial and lateral suborbicularis oculi fat pads contribute to the tear trough deformity observed in aging faces when separated from a descending malar fat pad.[2]
Restorating fat compartments to their youthful positions often necessitates identifying and dividing subdermal retaining ligaments, notably the zygomatic retaining ligaments (also referred to as a McGregor patch) and the mandibular retaining ligaments, shaping the pre-jowl sulcus overlying the medial mandibular body.[11] This nuanced approach ensures the anatomical rejuvenation of the midface, achieving more natural and comprehensive results.
Indications
Midface lifting is commonly prompted by the descent of malar fat pads, leading to pronounced nasolabial folds and concurrent facial fat pad atrophy.[12] The festoons, hypertrophic "bags" of orbicularis oculi muscle, may necessitate a midface lift, often performed alongside lower eyelid blepharoplasty and lateral canthopexy to prevent postoperative ectropion. This procedure can complement lower face or neck lifts for jowls or skin laxity cases, especially after significant weight loss. While some view midface lifting as a secondary option after failed dermal filler injections or fat transfers, others see volume augmentation as a beneficial complement to suspend the midface, achieving optimal midfacial rejuvenation surgically.
Contraindications
While midface lifting typically doesn't exert a significant postoperative physiological impact, certain preexisting conditions may complicate the procedure. Patients with bleeding disorders or those unable to discontinue anticoagulant therapy face a higher risk of postoperative hematoma, which can lead to prolonged ecchymosis, edema, infection, and suboptimal scarring. Patients with diabetes often need to temporarily halt antihyperglycemic medications, particularly sulfonylureas and sodium-glucose cotransporter-2 inhibitors, before surgery. Individuals prone to unfavorable scarring or healing issues may not be ideal candidates, with risk factors including diabetes mellitus, immunosuppression, active or prolonged tobacco use, history of facial radiation therapy, and autoimmune or collagen vascular diseases. Similarly, patients with a heightened risk of cardiopulmonary complications under general anesthesia should undergo medical optimization before considering elective aesthetic surgery.
Equipment
A marking pen is used preoperatively to denote the location of the tear troughs and nasolabial folds. The patient, even under general anesthesia, will benefit from injections with local anesthetic or a tumescent solution to reduce the requirement for anesthetic drugs and to improve hemostasis and postoperative pain control.[13] In particular, adding tranexamic acid to the injectate can decrease intraoperative bleeding during facial plastic surgery.[14][15] Betadine or isopropyl alcohol can be used to clean the skin. Isopropyl alcohol offers the advantage of not masking the patient's skin color and texture subtleties and doesn't require removal after the procedure. However, caution is needed to prevent contact with the corneas, as alcohol can cause severe damage.
Incisions and excess skin removal are performed intraoperatively using a #15 blade scalpel. Essential facelift instruments include Gorney-Freeman or Goldman-Fox scissors, a facelift retractor with a light source, skin hooks, suction, fine and heavy forceps, needle drivers, and electrocautery. Sutures play a crucial role, with many surgeons opting for heavy 2-0 polyester or polydioxanone material to suspend ptotic soft tissues and 4-0, 5-0, and 6-0 sutures for skin closure. Midface lifting can extend endoscopic brow lifting, requiring standard endoscopic brow lift instruments like a 30° Hopkins rod telescope, camera, optical dissector sheath, and Freer and Daniel elevators for surgical access. Bioresorbable implants are commonly used in endoscopic midface lifting, requiring 1 implant per side (see Image. Midface Lift Using Resorbable Tine Prosthesis).
Postoperatively, a bulky dressing is applied using fluff sponges, gauze rolls, and a compressive wrap—often in the form of a Barton dressing or something similar. Ice packs are recommended to limit bruising and swelling, and drains may be placed depending on the extent of dissection and the amount of bleeding encountered.
Personnel
During surgical procedures, the surgeon is typically accompanied by a team of medical professionals, including an anesthesia provider, a circulating nurse, and a surgical technologist. In some cases, an additional surgical assistant, such as a physician assistant, a nurse first assistant, or a resident/fellow, may also be present. Following the surgery, nursing staff play a critical role in ensuring patients are comfortable and following the prescribed postoperative care regimen, which may include administering medication, removing sutures or staples, monitoring activity restrictions, and providing wound care. Nursing staff are also responsible for recognizing and addressing any complications during recovery.
Preparation
An interprofessional approach to facial rejuvenation procedures will facilitate smooth surgery and improve patient satisfaction. This begins with thorough patient education regarding typical postoperative recovery and careful expectation management for the patient and the healthcare team members. Appropriate pain management and activity restrictions for 4 weeks after surgery should be discussed to optimize postoperative healing. A conversation regarding the role of adjunctive procedures, such as skin resurfacing, botulinum toxin, dermal filler injection, or other noninvasive treatments to further augment a youthful appearance should occur as well.[16] Perioperative herbal supplements, such as Arnica montana, may be recommended to minimize bruising.[17]
When signing the consent form, discussing the patient's surgical goals and confirming them in the preoperative holding area is crucial, as this helps ensure that the correct maneuvers are performed during surgery. Patients may have last-minute questions or concerns that affect the surgical plan, so addressing them before surgery is essential. During the preoperative physical examination, the tear troughs, NLFs, and jowls should be identified and marked, as well as any preexisting weakness of the facial nerve, particularly in the frontal and marginal mandibular branches, and any numbness in the distribution of the greater auricular nerve. Taking preoperative photographs of the patient in the operating room for reference during the case is also essential. The soft tissues shift upward when the patient is supine, making them appear deceptively younger than when upright and awake, which can obscure surgical targets. Before beginning the case, all surgical team members should meet to clarify equipment needs and outline the operative flow to help minimize delays during the procedure.
During surgery, the anesthesia provider may administer steroids to reduce postoperative edema and nausea, in addition to antibiotics that cover skin flora. Some surgical teams choose to use a total intravenous anesthetic with propofol and remifentanil instead of volatile anesthetics to limit intraoperative bleeding, coughing, or agitation during extubation.[18] Hemodynamic parameters must be monitored to reduce postoperative hematoma risk.[19] Communication with the anesthesia provider is crucial for blood pressure control and to prevent bleeding during and after surgery. If tranexamic acid is not included in the local anesthetic or tumescent solution mixture, it can be given intravenously to control bleeding. The recommended dosage is 1 g at the start, and an additional 1 g dose may be given at the end of the case or 4 hours after the first dose.[15][20]
Technique or Treatment
SMAS Imbrication with Deep Plane Component
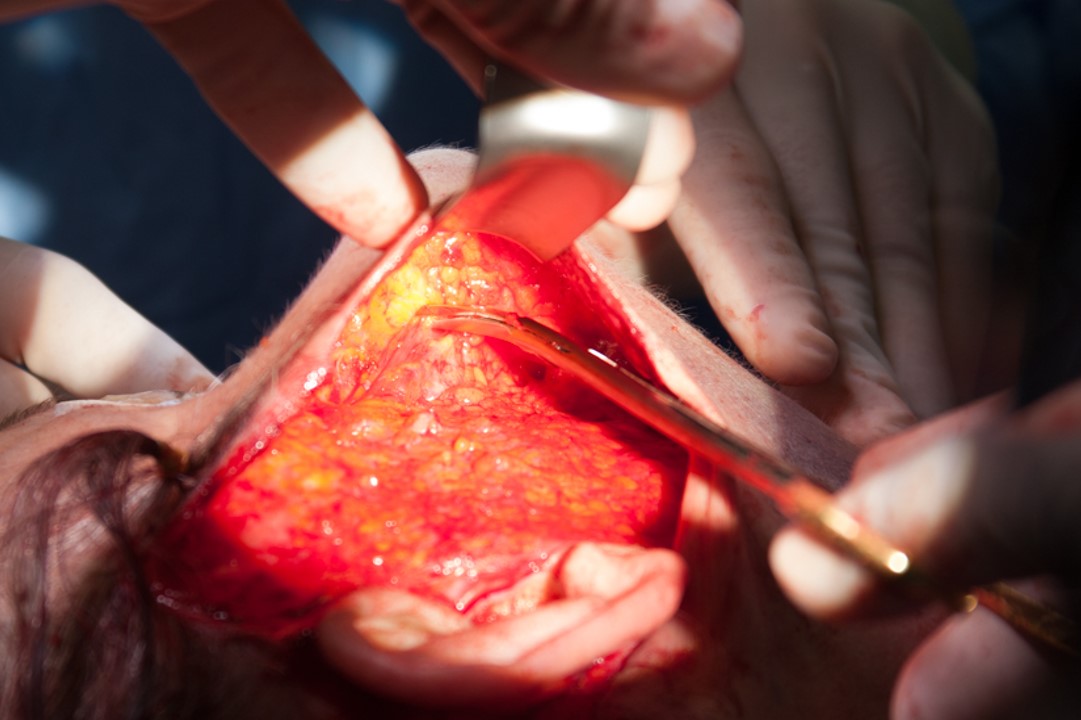
The midface lift is performed via a conventional Blair incision from the temporal hair tuft to the postauricular hairline as an adjunctive maneuver to standard rhytidectomy.[5][21][22] In men, the incision is placed between the sideburn's posterior border and the tragus's anterior margin to avoid pulling hair-bearing skin too close to the auricle. In contrast, in women, the incision may run in a preauricular rhytid or posterior to the free margin of the tragus. Subsequently, a subcutaneous flap is elevated up to a line running between the lateral canthus and the angle of the mandible. The elevation plane dives deep to run beneath the SMAS and separate the malar fat pad from the zygomaticus major muscle below it (see Image. Deep Plane Rhytidectomy). After the remaining facelift procedure, the malar fat pad can be suspended in a superolateral vector and secured with a fibrin sealant or absorbable sutures (3-0 or 4-0), ensuring symmetry between the left and right cheeks. Placement of a sterile, cold pack or glove filled with ice and wrapped in gauze on the first side of the face to be completed may help limit the progression of edema while the second side of the face is undergoing surgery.[23][24][25]
Minimal Access Cranial Suspension Facelift
Utilizing an abbreviated Blair incision without extension into the postauricular area, a subdermal elevation is executed over the midface, leaving the malar fat pad above the zygomaticus major muscle. A 0 polydioxanone suture forms a purse string around the malar fat pad, suspending it to the deep temporal fascia just lateral to the lateral orbital rim through a window in the orbicularis oculi muscle. The muscle window closure precedes redraping and excision of excess skin to minimize knot palpability. Additional purse-string sutures, if needed, can raise the remaining mid and lower face soft tissues, reducing jowls and enhancing mandibular definition (see Image. Minimal Access Cranial Suspension Facelift).[26]
Subciliary Midface Lift
A subciliary incision is initiated, extending from the lacrimal punctum laterally to a point 7 to 10 mm beyond the lateral canthus. A traction suture is applied through the gray line at the eyelid margin for superior retraction and corneal protection. The orbicularis oculi muscle is incised inferior to its pretarsal portion to preserve eyelid function and minimize postoperative ectropion risk. The dissection occurs in the preseptal plane, reaching the inferior orbital rim and the arcus marginalis. Surgeon preference dictates whether this is done as a single skin-muscle flap or in separate layers. This approach provides access to the lower eyelid fat pads for reduction or repositioning if needed.
Releasing the orbicularis retaining ligament and the zygomatic retaining ligament via a pre-periosteal or suborbicular approach is essential. Dissection extends about 2 cm inferior to the inferior orbital rim for SMAS access. The SMAS flap containing the orbicularis oculi muscle can be elevated in a vertical or superolateral vector. For a vertical vector, fixation to the arcus marginalis with a mattress suture is performed. Dissection along the zygoma to the frontozygomatic suture is carried out in the superolateral vector, staying along the bone to protect the facial nerve. The goal is to reach the deep temporal fascia/fascia of the temporalis muscle, where the SMAS-orbicularis oculi flap is suspended with a mattress suture. Redraping the orbicularis oculi muscle follows, and excess skin is excised before closing the subciliary incision with an absorbable suture.[25][27]
Implant-Assisted Endoscopic Midface Lift
There are absorbable implants made of a polylactic-polyglycolic acid polymer that dissolves over a period of 6 to 8 months. These implants can be used to simplify midface lifting. An implant with multiple tines (usually 5) and a short stem can anchor the SMAS and malar fat to the zygoma through a subciliary or transconjunctival incision. The latter approach requires an additional lateral canthotomy and inferior cantholysis for access.[28][29][30]
By using an implant with a longer stem, the end with the tines may be placed in a subperiosteal plane deep to the midfacial soft tissues and suspended to the temporalis fascia with absorbable sutures, such as 2-0 polydioxanone or polyglactin (see Image. Midface Lift Using Resorbable Tine Prosthesis). This procedure is often performed in conjunction with an endoscopic brow lift, as the dissection required to release the midfacial soft tissues from the zygoma is an extension of the elevation needed to release the arcus marginalis around the lateral aspect of the orbital rim, which is essential for effective endoscopic brow lifting.[31] The midface lift can be performed with no additional incisions beyond those required for endoscopic brow lifting. However, some authors prefer to add a superior gingivobuccal sulcus incision to improve access to the midfacial skeleton and enhance the release and elevation of its soft tissues.[32]
Postoperative Care
A compressive head dressing should be applied after the procedure and kept in place for 24 hours. In the recovery room, the nurses should know the ideal blood pressure parameters: systolic pressure <150 mm Hg and diastolic pressure >65 mm Hg.[33][34][33]
After 24 hours, the head dressing can be changed to a jaw bra with ice on and off the area at 20-minute intervals. If drains are placed, they should be removed at the dressing change appointment on postoperative day 1. Facial and greater auricular nerve function should be evaluated and documented. Patients should have a second follow-up appointment at 1 week for suture removal and wound check. Another appointment should be scheduled 1 month after surgery for wound evaluation and to discuss overall patient satisfaction. Photos should be taken 3 months postoperatively and at every follow-up visit afterward.
Complications
Patient dissatisfaction is the most prevalent complication in facial cosmetic procedures, emphasizing the importance of thorough preoperative counseling on expectations and careful patient selection.[33][35] In addition, various adverse outcomes may arise, including hematomas, which are relatively common and are more likely to develop in males due to increased blood supply needed for facial hair follicles. Hematomas often appear within the first 24 hours after surgery. Later in healing, seromas or sialoceles may develop, with the former addressed by needle drainage and compression dressing and the latter possibly benefiting from botulinum toxin injections into the parotid gland.[36] Permanent facial nerve injury is rare (<1%), with temporary weakness rates slightly higher, up to 2.6%.[37][38]
Other complications include wound infection, pixie ear deformity, poor scarring, and alopecia. Skin necrosis may also occur due to excessive tension at closure or thinning of the skin flap during elevation. Ectropion is a risk if a subciliary approach is used and excessive tension or cautery is applied. First bite syndrome is an uncommon sequela of face lifting.[39] Last, a depressive episode may occur during the postoperative period, particularly in patients with a history of depression. Goin et al reported that over 50% of female patients undergoing face lifting will experience depression after surgery.[40]
Clinical Significance
Midface lifting is a surgical procedure that can be performed alone or with other facial rejuvenation procedures like endoscopic brow lifting, blepharoplasty, and cervicofacial rhytidectomy. This procedure effectively addresses facial aging by restoring a youthful position to the malar soft tissues, which can help reduce the appearance of nasolabial folds and smooth the transition between the cheeks and the perioral area. By combining midface lifting with other surgeries, the surgeon can achieve a more comprehensive and holistic approach to facial rejuvenation.
Enhancing Healthcare Team Outcomes
Achieving optimal outcomes in midface lifting necessitates a collaborative effort among various healthcare professionals, each contributing distinct skills and responsibilities to enhance patient-centered care, safety, and overall team performance. Physicians, specifically facial plastic surgeons, must possess advanced surgical skills and a nuanced understanding of facial anatomy to perform midface lifting procedures effectively. They are responsible for conducting thorough preoperative evaluations, discussing realistic expectations with patients, and ensuring proper patient selection. Advanced practitioners, such as physician assistants or nurse practitioners, play a crucial role in preoperative and postoperative care, conducting assessments, educating patients, and assisting in managing potential complications. Nurses are integral to the perioperative process, assisting with patient preparation, monitoring vital signs, and providing postoperative care. Pharmacists contribute by managing medications, ensuring appropriate pain control, and minimizing the risk of adverse drug interactions. Interprofessional communication is paramount, with open and effective dialogue among team members fostering a collaborative environment. Care coordination involves seamless transitions between preoperative, intraoperative, and postoperative phases, ensuring a patient care continuum. The interdisciplinary team's collective efforts aim to prioritize patient safety, enhance outcomes, and deliver patient-centered care throughout the midface lifting process.
Media
(Click Image to Enlarge)
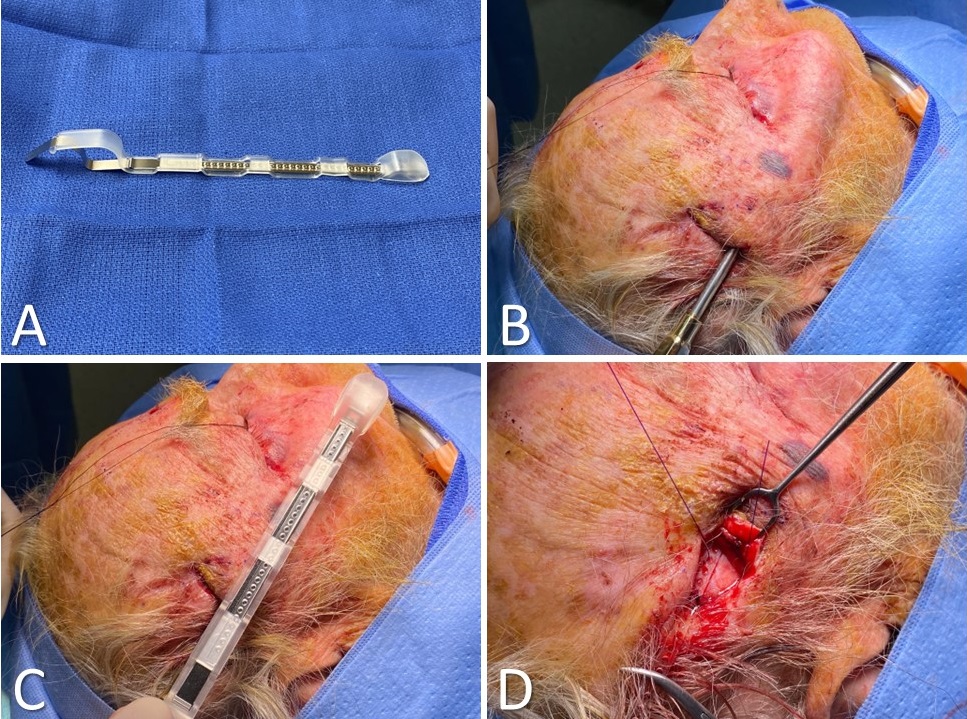
Midface Lift Using Resorbable Tine Prosthesis. A) The prosthesis is supplied in a retractable sheath that protects the tines and permits smooth insertion. B) Subperiosteal elevation proceeds along the lateral orbit down to the level of the malar eminence. C) The prosthesis is inserted, and the tines are engaged within the midfacial soft tissues. D) Tension is applied to the prosthesis to affect the midface lift, and the prosthesis is anchored to the temporalis fascia.
Contributed by Marc H Hohman, MD, FACS; Vladimir S Yakopson, MD, FACS; and Paloma I Perez, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
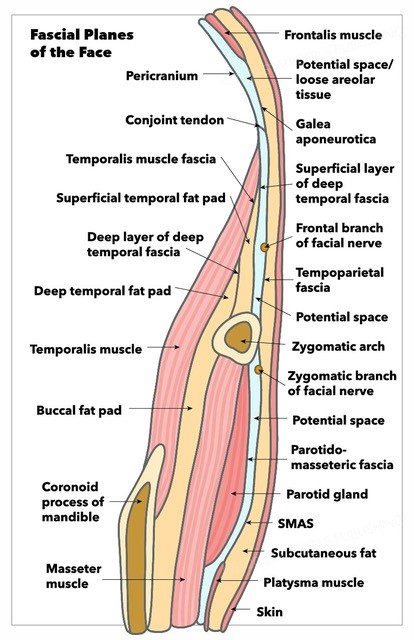
Fascial Planes of the Face and Musculature. This illustration depicts the fascial planes of the face, highlighting the continuity of the frontalis muscle, galea aponeurotica, temporoparietal fascia, superficial musculoaponeurotic system, platysma, and the location of the facial nerve.
Contributed by K Humphreys and MH Hohman, MD, FACS
(Click Image to Enlarge)
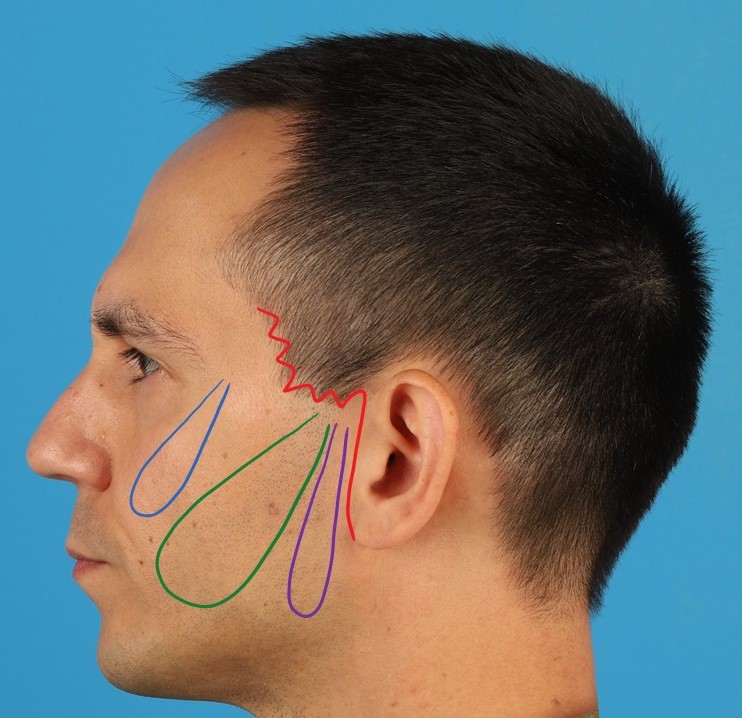
Minimal Access Cranial Suspension Facelift. The red line indicates the abbreviated Blair incision and the blue loop is the midface suspension suture. The green loop reduces the jowls, and the violet loop suspends the posterior platysma, improving the cervicomental angle.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)

Muscles of the Head, Face, and Neck. The epicranius, galea aponeurotica, frontalis, temporal fascia, auricularis superior, auricularis anterior, auricularis posterior, occipitalis, sternocleidomastoid, platysma, trapezius, orbicularis oculi, corrugator, procerus, nasalis, dilator naris anterior, dilator naris posterior, depressor septi, mentalis, orbicularis oris, masseter, zygomaticus, and risorius muscles are shown in the image.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Wan D, Amirlak B, Rohrich R, Davis K. The clinical importance of the fat compartments in midfacial aging. Plastic and reconstructive surgery. Global open. 2013 Dec:1(9):e92. doi: 10.1097/GOX.0000000000000035. Epub 2014 Jan 6 [PubMed PMID: 25289286]
Owsley JQ, Roberts CL. Some anatomical observations on midface aging and long-term results of surgical treatment. Plastic and reconstructive surgery. 2008 Jan:121(1):258-268. doi: 10.1097/01.prs.0000293872.14916.bb. Epub [PubMed PMID: 18176229]
Level 3 (low-level) evidenceDe Jong R, Hohman MH. Brow Ptosis. StatPearls. 2024 Jan:(): [PubMed PMID: 32809597]
Rebowe RE, Runyan C. Blepharoplasty. StatPearls. 2024 Jan:(): [PubMed PMID: 29494003]
Yang AJ, Hohman MH. Rhytidectomy. StatPearls. 2024 Jan:(): [PubMed PMID: 33232008]
Sykes JM, Riedler KL, Cotofana S, Palhazi P. Superficial and Deep Facial Anatomy and Its Implications for Rhytidectomy. Facial plastic surgery clinics of North America. 2020 Aug:28(3):243-251. doi: 10.1016/j.fsc.2020.03.005. Epub 2020 May 6 [PubMed PMID: 32503712]
Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plastic and reconstructive surgery. 1976 Jul:58(1):80-8 [PubMed PMID: 935283]
Pitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plastic and reconstructive surgery. 1966 Oct:38(4):352-6 [PubMed PMID: 5926990]
Gosain AK, Sewall SR, Yousif NJ. The temporal branch of the facial nerve: how reliably can we predict its path? Plastic and reconstructive surgery. 1997 Apr:99(5):1224-33; discussion 1234-6 [PubMed PMID: 9105349]
Dorafshar AH, Borsuk DE, Bojovic B, Brown EN, Manktelow RT, Zuker RM, Rodriguez ED, Redett RJ. Surface anatomy of the middle division of the facial nerve: Zuker's point. Plastic and reconstructive surgery. 2013 Feb:131(2):253-257. doi: 10.1097/PRS.0b013e3182778753. Epub [PubMed PMID: 23357986]
Cotofana S, Lachman N. Anatomy of the Facial Fat Compartments and their Relevance in Aesthetic Surgery. Journal der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology : JDDG. 2019 Apr:17(4):399-413. doi: 10.1111/ddg.13737. Epub 2019 Jan 30 [PubMed PMID: 30698919]
Gierloff M, Stöhring C, Buder T, Gassling V, Açil Y, Wiltfang J. Aging changes of the midfacial fat compartments: a computed tomographic study. Plastic and reconstructive surgery. 2012 Jan:129(1):263-273. doi: 10.1097/PRS.0b013e3182362b96. Epub [PubMed PMID: 21915077]
Roberge CW, McEwen M. The effects of local anesthetics on postoperative pain. AORN journal. 1998 Dec:68(6):1003-12 [PubMed PMID: 9864591]
Level 2 (mid-level) evidenceCouto RA, Charafeddine A, Sinclair NR, Nayak LM, Zins JE. Local Infiltration of Tranexamic Acid With Local Anesthetic Reduces Intraoperative Facelift Bleeding: A Preliminary Report. Aesthetic surgery journal. 2020 May 16:40(6):587-593. doi: 10.1093/asj/sjz232. Epub [PubMed PMID: 31504134]
Locketz GD, Lozada KN, Bloom JD. Tranexamic Acid in Aesthetic Facial Plastic Surgery: A Systematic Review of Evidence, Applications, and Outcomes. Aesthetic surgery journal. Open forum. 2020 Sep:2(3):ojaa029. doi: 10.1093/asjof/ojaa029. Epub 2020 Jun 14 [PubMed PMID: 33791652]
Level 1 (high-level) evidenceSantosa KB, Oliver JD, Thompson G, Beil RJ. Perioperative Management of the Facelift Patient. Clinics in plastic surgery. 2019 Oct:46(4):625-639. doi: 10.1016/j.cps.2019.06.008. Epub 2019 Aug 2 [PubMed PMID: 31514813]
Seeley BM, Denton AB, Ahn MS, Maas CS. Effect of homeopathic Arnica montana on bruising in face-lifts: results of a randomized, double-blind, placebo-controlled clinical trial. Archives of facial plastic surgery. 2006 Jan-Feb:8(1):54-9 [PubMed PMID: 16415448]
Level 1 (high-level) evidenceDušanovic A, Vlajkovic G, Sindjelic R. Use of Propofol in Combination with Remifentanil for Plastic and Reconstructive Surgery. Aesthetic plastic surgery. 2016 Oct:40(5):806-7. doi: 10.1007/s00266-016-0654-5. Epub 2016 May 25 [PubMed PMID: 27225875]
Maricevich MA, Adair MJ, Maricevich RL, Kashyap R, Jacobson SR. Facelift complications related to median and peak blood pressure evaluation. Aesthetic plastic surgery. 2014 Aug:38(4):641-7. doi: 10.1007/s00266-014-0353-z. Epub 2014 Jun 10 [PubMed PMID: 24912427]
Cohen JC, Glasgold RA, Alloju LM, Glasgold MJ. Effects of Intravenous Tranexamic Acid During Rhytidectomy: A Randomized, Controlled, Double-Blind Pilot Study. Aesthetic surgery journal. 2021 Jan 25:41(2):155-160. doi: 10.1093/asj/sjaa072. Epub [PubMed PMID: 32173730]
Level 1 (high-level) evidenceJoshi K, Hohman MH, Seiger E. SMAS Plication Facelift. StatPearls. 2025 Jan:(): [PubMed PMID: 30285353]
Raggio BS, Patel BC. Deep Plane Facelift. StatPearls. 2024 Jan:(): [PubMed PMID: 31424861]
Charafeddine AH, Zins JE. The Extended Superficial Musculoaponeurotic System. Clinics in plastic surgery. 2019 Oct:46(4):533-546. doi: 10.1016/j.cps.2019.05.002. Epub 2019 Jul 18 [PubMed PMID: 31514806]
Baker SR. Deep plane rhytidectomy and variations. Facial plastic surgery clinics of North America. 2009 Nov:17(4):557-73, vi. doi: 10.1016/j.fsc.2009.06.003. Epub [PubMed PMID: 19900662]
Freeman MS. Rejuvenation of the midface. Facial plastic surgery : FPS. 2003 May:19(2):223-36 [PubMed PMID: 12825162]
Tonnard P, Verpaele A. The MACS-lift short scar rhytidectomy. Aesthetic surgery journal. 2007 Mar-Apr:27(2):188-98. doi: 10.1016/j.asj.2007.01.008. Epub [PubMed PMID: 19341646]
Yin VT, Chou E, Nakra T. The transeyelid midface lift. Clinics in plastic surgery. 2015 Jan:42(1):95-101. doi: 10.1016/j.cps.2014.09.004. Epub [PubMed PMID: 25440746]
Saltz R, Ohana B. Thirteen years of experience with the endoscopic midface lift. Aesthetic surgery journal. 2012 Nov:32(8):927-36. doi: 10.1177/1090820X12462714. Epub [PubMed PMID: 23110925]
Level 2 (mid-level) evidenceBerkowitz RL, Apfelberg DB, Simeon S. Midface lift technique with use of a biodegradable device for tissue elevation and fixation. Aesthetic surgery journal. 2005 Jul-Aug:25(4):376-82. doi: 10.1016/j.asj.2005.05.011. Epub [PubMed PMID: 19338834]
Anderson RD, Lo MW. Endoscopic malar/midface suspension procedure. Plastic and reconstructive surgery. 1998 Nov:102(6):2196-208 [PubMed PMID: 9811022]
Raggio BS, Winters R. Endoscopic Brow Lift. StatPearls. 2024 Jan:(): [PubMed PMID: 31424804]
Hönig JF. Subperiosteal Endotine-assisted vertical upper midface lift. Aesthetic surgery journal. 2007 May-Jun:27(3):276-88. doi: 10.1016/j.asj.2007.04.005. Epub [PubMed PMID: 19341654]
Fedok FG. The Avoidance and Management of Complications, and Revision Surgery of the Lower Face and Neck. Clinics in plastic surgery. 2018 Oct:45(4):623-634. doi: 10.1016/j.cps.2018.06.010. Epub 2018 Aug 10 [PubMed PMID: 30268247]
Chung KH, Cho MS, Jin H. Perioperative Hypertension Management during Facelift under Local Anesthesia with Intravenous Hypnotics. Archives of plastic surgery. 2017 Jul:44(4):276-282. doi: 10.5999/aps.2017.44.4.276. Epub 2017 Jul 15 [PubMed PMID: 28728322]
Cristel RT, Irvine LE. Common Complications in Rhytidectomy. Facial plastic surgery clinics of North America. 2019 Nov:27(4):519-527. doi: 10.1016/j.fsc.2019.07.008. Epub 2019 Sep 4 [PubMed PMID: 31587771]
Maharaj S, Mungul S, Laher A. Botulinum toxin A is an effective therapeutic tool for the management of parotid sialocele and fistula: A systematic review. Laryngoscope investigative otolaryngology. 2020 Feb:5(1):37-45. doi: 10.1002/lio2.350. Epub 2020 Jan 23 [PubMed PMID: 32128429]
Level 1 (high-level) evidenceHohman MH, Bhama PK, Hadlock TA. Epidemiology of iatrogenic facial nerve injury: a decade of experience. The Laryngoscope. 2014 Jan:124(1):260-5. doi: 10.1002/lary.24117. Epub 2013 Apr 18 [PubMed PMID: 23606475]
Level 2 (mid-level) evidenceBaker DC, Conley J. Avoiding facial nerve injuries in rhytidectomy. Anatomical variations and pitfalls. Plastic and reconstructive surgery. 1979 Dec:64(6):781-95 [PubMed PMID: 515227]
Gunter AE, Llewellyn CM, Perez PB, Hohman MH, Roofe SB. First Bite Syndrome Following Rhytidectomy: A Case Report. The Annals of otology, rhinology, and laryngology. 2021 Jan:130(1):92-97. doi: 10.1177/0003489420936713. Epub 2020 Jun 21 [PubMed PMID: 32567395]
Level 3 (low-level) evidenceGoin MK, Burgoyne RW, Goin JM, Staples FR. A prospective psychological study of 50 female face-lift patients. Plastic and reconstructive surgery. 1980 Apr:65(4):436-42 [PubMed PMID: 7360810]