Definition/Introduction
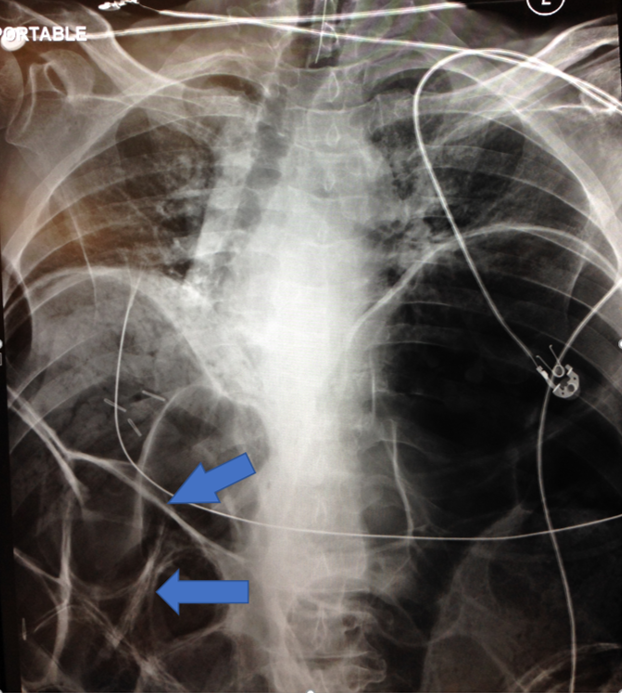
The Rigler sign, also known as the double-wall sign, indicates the presence of free air within the peritoneal cavity (pneumoperitoneum). The sign imprints a visible pattern on a plain abdominal radiograph in the supine position. This sign occurs due to the separation between free air and intraluminal contents by the intestinal wall, which highlights the air’s radiolucency and the wall’s radiopacity. Both the serosal and luminal surfaces of the bowel are visible (see Image. Rigler Sign).[1]
In 1942, American radiologist Leo G Rigler (1896-1979) described the Rigler sign for pneumoperitoneum based on patterns observed in 4 cases reported in 1941. He noted that this sign was present when large quantities of free air were in the peritoneal cavity.[2]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Pneumoperitoneum can be detected in small quantities, as little as 1 mL, on upright chest or abdominal radiography under specific conditions.[3] Computed tomography (CT) scans offer greater sensitivity and specificity than conventional radiographic techniques and are generally more accessible and cost-effective.[4] As many patients requiring abdominal radiography for suspected pneumoperitoneum are too ill to stand or sit, the plain supine projection is often used. However, this modality has lower diagnostic accuracy for pneumoperitoneum (56%) compared to other projections, such as left lateral decubitus (96%), chest (85%), and upright (60%).[5]
Other studies show that radiography can detect pneumoperitoneum in only 69% to 89% of cases with visceral perforation.[6][7] The sensitivity and specificity of abdominal radiography for detecting pneumoperitoneum are lower compared to CT scans.[8][9] The widespread use of modern CT scan technology has made abdominal radiography less common in developed healthcare systems, and conventional abdominal radiology is often omitted in the evaluation of most adult patients with acute abdominal pain.[10]
Clinical Significance
The Rigler sign is the second most common indicator of pneumoperitoneum, with the right upper quadrant subdiaphragmatic free air being the most common. Studies report that the prevalence of the Rigler sign is lower than that of right upper quadrant subdiaphragmatic free air (46% versus 32%).[11] Clear recognition of the Rigler sign typically requires a large quantity of free air, around 1000 mL. A pseudo-Rigler sign can occur when 2 loops of gas-distended bowel contact each other, thereby enhancing the radiopacity of the intestinal wall against the air-filled loops and potentially misleading the diagnosis of pneumoperitoneum.[12] If the Rigler sign is present, abdominal/pelvic CT scanning and surgical consultation are warranted in the appropriate clinical context.[10]
Media
(Click Image to Enlarge)
References
Ly JQ. The Rigler sign. Radiology. 2003 Sep:228(3):706-7 [PubMed PMID: 12954891]
Lewicki AM. The Rigler sign and Leo G. Rigler. Radiology. 2004 Oct:233(1):7-12 [PubMed PMID: 15333763]
Gans SL, Stoker J, Boermeester MA. Plain abdominal radiography in acute abdominal pain; past, present, and future. International journal of general medicine. 2012:5():525-33. doi: 10.2147/IJGM.S17410. Epub 2012 Jun 13 [PubMed PMID: 22807640]
Stapakis JC,Thickman D, Diagnosis of pneumoperitoneum: abdominal CT vs. upright chest film. Journal of computer assisted tomography. 1992 Sep-Oct; [PubMed PMID: 1522261]
Roh JJ, Thompson JS, Harned RK, Hodgson PE. Value of pneumoperitoneum in the diagnosis of visceral perforation. American journal of surgery. 1983 Dec:146(6):830-3 [PubMed PMID: 6650772]
Winek TG, Mosely HS, Grout G, Luallin D. Pneumoperitoneum and its association with ruptured abdominal viscus. Archives of surgery (Chicago, Ill. : 1960). 1988 Jun:123(6):709-12 [PubMed PMID: 3285808]
Level 2 (mid-level) evidenceBansal J, Jenaw RK, Rao J, Kankaria J, Agrawal NN. Effectiveness of plain radiography in diagnosing hollow viscus perforation: study of 1,723 patients of perforation peritonitis. Emergency radiology. 2012 Apr:19(2):115-9. doi: 10.1007/s10140-011-1007-y. Epub 2011 Dec 6 [PubMed PMID: 22143167]
Catalano O, [Computed tomography in the study of gastrointestinal perforation]. La Radiologia medica. 1996 Mar; [PubMed PMID: 8628938]
Level 2 (mid-level) evidenceLaméris W, van Randen A, van Es HW, van Heesewijk JP, van Ramshorst B, Bouma WH, ten Hove W, van Leeuwen MS, van Keulen EM, Dijkgraaf MG, Bossuyt PM, Boermeester MA, Stoker J, OPTIMA study group. Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ (Clinical research ed.). 2009 Jun 26:338():b2431. doi: 10.1136/bmj.b2431. Epub 2009 Jun 26 [PubMed PMID: 19561056]
Gans SL, Pols MA, Stoker J, Boermeester MA, expert steering group. Guideline for the diagnostic pathway in patients with acute abdominal pain. Digestive surgery. 2015:32(1):23-31. doi: 10.1159/000371583. Epub 2015 Jan 28 [PubMed PMID: 25659265]
Levine MS, Scheiner JD, Rubesin SE, Laufer I, Herlinger H. Diagnosis of pneumoperitoneum on supine abdominal radiographs. AJR. American journal of roentgenology. 1991 Apr:156(4):731-5 [PubMed PMID: 2003436]
Level 2 (mid-level) evidencede Lacey G, Bloomberg T, Wignall BK. Pneumoperitoneum: the misleading double wall sign. Clinical radiology. 1977 Jul:28(4):445-8 [PubMed PMID: 872511]