Introduction
Cauliflower ear deformity descriptions date back to early Roman and Greek history. Literary and artistic collections from those periods are replete with accounts of the deformed or damaged ears of wrestlers, boxers, and other pugilists. Notably, the term "earmark" was coined during this period because wrestlers could be recognized by the characteristic appearance of their misshapen pinnae.[1]
Medical appreciation for this affliction has a similar storied past. Though case descriptions may be found in Hippocrates' works, formal research into the disease did not begin until the mid-1800s. A second idiopathic mechanism was thought at the time to be responsible for cauliflower ear deformity besides direct trauma. The idiopathic hypothesis is derived from observations of people of advanced age or with mental health conditions.
The more conventional understanding of cauliflower ear developed in the 20th century, relating the pathology to a maladaptive and overly exuberant inflammatory response to the presence of an auricular hematoma or abscess (see Image. Auricular Hematoma).[2][3] However, patients often find cauliflower ear deformity to be both unsightly and inconvenient, regardless of the cause. The condition may interfere with earphone-wearing, which is popular in modern times. Thus, preventing and treating this condition are important for emergency healthcare providers and surgical specialists.
Auricular Histology
The outer ear comprises several layers crucial for its function and protection. The skin covers both the external ear canal and auricle. The outer ear skin has essential structures, including hair follicles, sebaceous glands, and sweat glands, offering defense against environmental factors and aiding in temperature regulation. The epidermis is comprised of stratified squamous epithelium, providing a barrier against pathogens and preventing water loss. The dermis is situated below the epidermis, housing blood vessels, nerves, and connective tissue, providing structural support, and supplying nutrients to the overlying layers.
The auricle's core structural component is elastic cartilage, responsible for its shape and flexibility. Chondrocytes lie within a matrix of collagen and elastin fibers, though cartilage is poorly vascularized. The perichondrium is a layer of fibrous tissue surrounding the cartilage. This layer offers structural support to the elastic cartilage, supplies oxygen and nutrients to cartilage cells through its rich vascular supply, and contains chondroblasts responsible for cartilage repair and growth. The perichondrium also serves as an attachment site for the overlying skin, anchoring it in place and ensuring the auricle's integrity.
Notably, the outer ear's anatomy exhibits distinct features. The concave (inner or anterior) side has a thin subcutaneous layer and is closely attached to the auricular perichondrium. In contrast, the auricle's convex (outer or posterior) side has a thicker subcutaneous stratum and a muscle layer superficial to the perichondrium. The auricle remains susceptible to environmental influences and trauma despite its protective layers.[4][5] Structural disruption can lead to complications like cauliflower ear deformity.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Cauliflower ear is an auricular deformity typically arising as a complication of auricular hematoma formation from blunt trauma. Severe cases often result from repeated, inadequately treated hematomas over time, with the condition commonly observed in individuals involved in activities predisposing to ear trauma, such as wrestling or boxing. Tangential, shearing blows are more likely to cause hematoma formation compared to orthogonally-directed trauma.[6]
The hematoma elevates the auricular perichondrium from the underlying cartilage, resulting in cartilage devascularization. Untreated hematomas may lead to necrosis, infection, or cauliflower ear deformity (see Images. Mild Cauliflower Ear, Severe Cauliflower Ear). Cauliflower ear deformity develops from fibrocartilage hyperproliferation and fibrosis, triggered by the inflammatory response to compromised auricular cartilage circulation.[7][8][9] Other inflammatory and infectious conditions, such as relapsing polychondritis, leprosy, and phaeohyphomycosis, may also lead to cauliflower ear deformity, albeit far less commonly than trauma.[10][11][12]
Epidemiology
The exact prevalence of cauliflower ear deformity in the general population has not been reported in the literature. However, various studies describe the condition's frequency in diverse athlete groups. Generally, the risk of developing cauliflower ear increases with the level of competition in high-risk sports like wrestling, boxing, martial arts, or rugby. Older athletes who continue to compete are also more likely to develop cauliflower ear than younger competitors.[13] A study reported auricular hematoma's prevalence to be 96% among national-champion-level Finnish martial artists, with cauliflower ear seen in 84% of men.[14] A similar paper from Germany found that 55.5% of high-level judo practitioners have cauliflower ears, with male athletes more likely than women to develop the condition and sustain severe deformities.
Pathophysiology
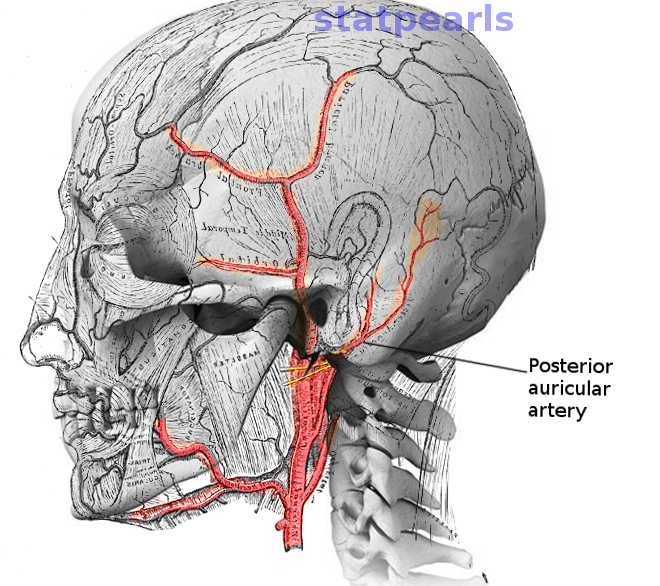
Debate surrounds the precise mechanism behind cauliflower ear deformity. While mid-1970s experiments on rabbits suggested that hematomas in the intercartilaginous space were responsible for the condition, subsequent research indicated that blood accumulation in the subperichondrial space could also disrupt blood flow from the posterior auricular and superficial temporal arteries to the anterior ear, resulting in auricular cartilage necrosis (see Image. Posterior Auricular Artery).[15] The posterior auricular artery is the auricle's primary arterial source and is responsible for perfusing both the posterior ear surface and the conchal bowl. The superficial temporal artery feeds the remainder of the anterior surface.[16] Over time, the hematoma is replaced by chondroblasts to form neocartilage. This process initiates fibrosis and contracture cascades, ultimately leading to cauliflower ear development.
The subperichondrial hematoma hypothesis is most commonly taught. However, the scant evidence available in humans seems to point to intracartilaginous auricular hematoma being more common, at least in recurrent cases, which are more likely to produce cauliflower ear.[17] Regardless of the hematoma's precise location, the skin of the auricle's anterior aspect tightly adheres to the underlying perichondrium with little intervening subcutaneous tissue to mitigate blunt trauma. Cauliflower ear appears most commonly in the scaphoid and triangular fossae's superior aspect and may also involve the concha. Perichondrial shearing and hematoma formation less frequently affect the posterior auricle due to the thicker subcutaneous layer and the presence of areolar and muscle tissue in this region. Consequently, cauliflower ear is rarely seen posteriorly.[18]
Histopathology
Postoperative cauliflower ear specimen examinations reveal fibrous tissue containing blood vessels lying between the normal elastic cartilage's anterior and posterior layers.[19] Heterotopic ossification may also occur in long-standing, chronic cases, making surgical auricular resculpting more challenging.[20] Cartilage formation occurs on either side of the hematoma if no treatment is sought 2 weeks after blood pooling starts. Soft tissue replaces the hematoma at 3 weeks. By the 8th week, fibrocartilage replaces the soft tissue. By the 14th week, bony formation, calcification, and further cartilage growth occur.
History and Physical
History
Individuals with cauliflower ears typically present with visible deformity in the auricle's cartilaginous region. The deformity may impact hearing by obstructing the ear canal or causing compression of the surrounding structures. Patients may also experience functional limitations, such as difficulty wearing glasses or helmets due to the altered ear shape. A sensation of fullness or pressure in the ear may also be elicited, with some individuals reporting difficulty sleeping on the affected side due to discomfort.
The ear lesion may be further described to be initially soft and tender immediately after the inciting event, as it contains blood or fluid. The affected area becomes firmer and more misshapen over time due to fibrocartilage hyperproliferation, possibly with residual discomfort.
A history of recurrent trauma to the affected ear is often reported, usually during contact sports like wrestling, boxing, rugby, and, increasingly, mixed martial arts. Not all patients recall an auricular hematoma episode preceding the deformity. Cartilaginous ear piercing may also produce cauliflower ear resulting from subsequent blood collection or infection with abscess formation. Fibrocartilaginous overgrowth arises from a failure to completely drain the fluid collection or prevent a recurrence. Alternative diagnoses should be considered if prior trauma or infection is not elicited on history. Children and older individuals are at risk for nonaccidental trauma.[21][22]
Auricular keloids may have similar presentations to cauliflower ears. These lesions also generally arise at the site of an ear piercing, although not necessarily preceded by hematoma or infection. The lobule is another frequent site of keloidal scarring. Keloids arising from the auricle grow exophytically. However, cauliflower ear deformity differs from keloids due to cartilage involvement (see Image. Helical Keloid Scar, Auricular Lobule Keloid).
Physical Examination
Physical examination of cauliflower ear deformity begins with visual inspection for swelling, deformity, and discoloration. The affected area must be palpated gently to assess tenderness, firmness, and texture irregularities, noting fluid or fibrosis indicators. The ear canal must be examined for obstruction affecting hearing and signs of swelling or deformity. Otoscopy can help evaluate for tympanic membrane and middle ear involvement.
The skin overlying a cauliflower ear typically appears normal. A neoplasm should be considered in the presence of pigmentation abnormalities, erythema, or ulceration, possibly requiring biopsy and imaging. The affected area may feel firm, with little to no tenderness. The lesion may obstruct the ear canal and affect hearing tests.
Additional head trauma sequelae must be ruled out, particularly hearing loss and traumatic brain injury signs, given the condition's typically traumatic origin. Further evaluation, eg, with audiometry or head computed tomography, may be necessary if focal deficits are noted.
Evaluation
Cauliflower ear is a clinical diagnosis, requiring no formal testing or imaging. However, traumatic brain injury signs in the setting of recurrent head trauma warrant neuroimaging. Additionally, abnormalities of the overlying skin in a patient with risk factors for cutaneous malignancies, eg, chronic sun exposure, family history, and immunosuppression, require consideration for a biopsy.
Treatment / Management
Cauliflower ear management varies based on the timing of presentation and deformity severity. However, prevention is key through adequate ear protection during contact sports. Utilizing protective headgear significantly reduces the incidence of auricular hematomas and subsequent cauliflower ear deformities, as evidenced by studies of wrestlers demonstrating as much as a 50% reduction in hematoma frequency.[23][24][25](B2)
Early auricular hematoma identification and management are crucial for preventing cauliflower ear, with the best outcomes achieved through prompt intervention within 6 hours of injury before cartilage death occurs. Aspiration with an 18-gauge needle is typically performed to evacuate the hematoma before clot consolidation occurs. If the patient presents outside this window, an incision may be made along the medial helical rim or the junction between the concha and antihelix—whichever is closer to the hematoma—to facilitate clot evacuation and irrigation (see Image. Auricle Surface Anatomy).
Alternatively, the patient may wait approximately a week postinjury to let the clot liquefy again, allowing for successful needle aspiration. However, fibrocartilage deposition may start within that period. Thus, prompt management is usually preferred. Pressure must be applied to the treated area for a week after clot removal. The patient may also receive a course of prophylactic antibiotics. In cooperative patients, these procedures may be conducted under local anesthesia with a circumauricular block, supplemented by direct infiltration of the conchal bowl if necessary.[26]
The perichondrium can reattach to the auricular cartilage and restore circulation after hematoma removal. However, blood may continue to accumulate despite complete hematoma evacuation unless pressure is effectively applied to the auricle, and the potential space is closed. Various compression methods are described in the literature, including cotton bolsters, dental silicone, splints, casts, magnetic discs, buttons, and mattress sutures, with no single technique proven superior. However, a bolsterless suture technique allows athletes to resume normal activity faster.[27][28][29] Radiation therapy, studied in rabbits but not yet employed in humans, is explored for cauliflower ear prevention post-hematoma drainage, aiming to mitigate the inflammatory response and fibrosis, similar to its effect on keloid development.[30](B2)
Surgical intervention remains the treatment mainstay for patients who present outside the window when auricular hematoma drainage is feasible. Surgical referral is appropriate for any patient with cauliflower ear if the high-risk activity predisposing to the condition has been discontinued. The surgical approach for cauliflower ear correction varies, depending on the deformity’s severity and location. Mild cases may involve sculpting of deformed cartilage if the helix or antihelix is involved or resection if the conchal bowl is affected. The conchal bowl and the cartilaginous external auditory canal's posterolateral aspect minimally affect auricular shape and support.[31]
Access to the cartilage may be achieved through various incisions: along the medial helical rim, antihelix-conchal bowl junction, postauricular sulcus, or posterior helical aspect. Skin flaps can be raised through these incisions anteriorly and posteriorly, as needed (see Image. Surgical Repair of Cauliflower Ear). Sculpting techniques may involve a #15 blade scalpel, curettes, biopsy punches (4, 5, and 6 mm punches, used as curettes), or a high-speed otologic drill (often with a 4 mm diamond bur). The otologic drill is especially useful if heterotopic calcification is present.
The modified Valente technique uses a postauricular sulcus skin excision, commonly used in otoplasty, to expose the auricular framework’s anterior aspect. An incision through the cartilage just medial to the helix releases helical tension caused by the cauliflower ear deformity, partially correcting the distortion. The skin is then lifted off the anterior auricle in a supraperichondrial plane, allowing access to the fibroneocartilage. Abnormal cartilage is excised, and the auricle is sculpted appropriately. Mustardé-type sutures are then placed through the posterior cartilage to restore normal pinna contour.[32]
Yotsuyanagi et al describe a more detailed cauliflower ear assessment to determine the appropriate surgical approach. The group categorizes cauliflower ear based on the deformity's location and the degree of auricular distortion, with some patients having more than 1 class of deformity concurrently.
Type I deformities do not significantly alter the auricular outline and include the following subtypes:
- Type IA: The deformity is restricted to the concha, approached via an incision at the antihelix-conchal bowl junction.
- Type IB: The deformity extends from the antihelix to the helix, approached via an incision along the helical rim’s medial margin or posterior helical incision.
- Type IC: The deformity extends throughout the auricle, approached by combining the incisions used for type IA and IB deformities.
- Type ID: A scar contracture prevents the skin from lying flat even after the cartilage deformity is resected. These deformities often require postauricular island flaps for reconstruction.
Type II deformities are characterized by significant auricular outline distortion and include the following subtypes:
- Type IIA: The auricular cartilage retains structural integrity. The approach is via the incisions used for type IA and IB deformities. These cases generally require conchal cartilage grafting harvested from both ears.
- Type IIB: The remaining cartilage cannot support a normal-appearing auricle. The approach is via postauricular or posterior helical incisions. Costal cartilage grafting replaces a substantial portion of the auricle.
Microtia repair techniques are employed for high-grade deformities, such as type IIB cauliflower ear. Reinforcement or replacement of some or all of the auricular framework with conchal or costal cartilage may be required if extensive cartilage distortion or ossification has occurred, and the auricle cannot be sculpted or sutured back into a normal shape.[33] These reconstructions are challenging and often produce disappointing results if attempted by providers without significant experience and clinical volume, as with microtia reconstruction.
Compression should be applied after the reconstruction, typically with a dressing and a splint, similar to auricular hematoma drainage. Some authors advocate leaving the splint in place for several months to help prevent hematoma formation and manage edema. Regular follow-up during the first year after surgery is important when scar contracture and auricular distortion are frequent. Prompt corticosteroid injections may prevent or mitigate these complications.
Differential Diagnosis
Conditions that can present with auricular distortion include the following:
- Abscess
- Chondritis
- Chondrodermatitis nodularis chronica helicis
- Chondroma
- Chondrosarcoma
- Dermatofibroma
- Ear canal squamous cell carcinoma
- Ear canal trauma
- Exostosis
- Foreign body
- Hemangioma
- Hematoma
- Keloid
- Osteoma
- Pseudocyst of the auricle
- Seroma
- Skin cancer: basal cell carcinoma, squamous cell carcinoma, non-pigmented melanoma, Merkel cell carcinoma, dermatofibrosarcoma
A thorough clinical and diagnostic assessment can distinguish cauliflower ear deformity from these conditions, which is essential for proper treatment selection.
Prognosis
Early treatment of auricular hematoma with drainage and pressure application greatly reduces the risk of developing a cauliflower ear or minimizes deformity. Longstanding cauliflower ears may have disappointing aesthetic outcomes, especially if the patient persists in activities predisposing to auricular trauma. Prevention through protective headgear or prompt hematoma drainage is recommended. Continued participation in activities like boxing or wrestling can exacerbate cauliflower ear. Surgical repair becomes more challenging with severe deformity. Thus, this intervention is ideally undertaken after discontinuing traumatic activities to avoid multiple surgeries.
Complications
Cauliflower ear complications are mainly aesthetic, though rare cases may involve pain or external auditory canal obstruction. Recurrence of deformity due to scar contracture is a postoperative risk, necessitating regular follow-up for up to a year. Prompt identification and treatment with corticosteroid injections and splinting are crucial.
Consultations
Emergent consultation with an otolaryngologist, oral and maxillofacial surgeon, facial plastic surgeon, or plastic surgeon is required if the physician is uncomfortable managing an auricular hematoma, seroma, or abscess. Cauliflower ear reconstruction is typically undertaken by a plastic or facial plastic surgeon.
Deterrence and Patient Education
Primary prevention of cauliflower ear entails protective measures during activities that increase auricular trauma risk, like wearing headgear or helmets with ear protection during contact sports. Educating athletes about auricular trauma risks and consistent protective equipment use is vital. Techniques to minimize direct ear trauma should also be promoted to reduce hematoma formation. Secondary prevention involves early recognition and prompt auricular hematoma management to prevent cauliflower ear development. Healthcare providers must be trained to identify hematoma signs, and patients should seek medical attention promptly after ear trauma. Prompt hematoma drainage is essential to prevent fibrocartilage deposition, with follow-up care including monitoring for recurrence and proper wound management.
Pearls and Other Issues
Cauliflower ear, a common sequela of auricular trauma, is best managed by prevention. The condition usually arises from chronic trauma and is associated with activities that predispose people to repeated auricular injury. The condition may be prevented by consistently using protective headgear during contact sports.
The diagnosis of cauliflower ear is clinical. Diagnostic tests are generally unnecessary unless signs of other underlying pathologies are present, including traumatic brain injury and skin cancer. Early recognition and prompt drainage of auricular hematomas are essential to prevent fibrocartilage deposition and deformity. Proper wound care and close monitoring for recurrence are crucial components of follow-up management to prevent infection and promote healing.
Healthcare providers should educate patients, especially athletes, about the risks of auricular trauma and the importance of seeking medical attention promptly following ear injury. Techniques to minimize direct ear trauma, such as avoiding prolonged friction or shearing forces, can help reduce the risk of hematoma formation.
Enhancing Healthcare Team Outcomes
Patients with cauliflower ear may present to the emergency department physician, nurse practitioner, primary care provider, or sports physician, who may provide initial treatment and counseling. A referral to a specialist in otorhinolaryngology or plastic surgery is required for definitive treatment. While the diagnosis is simple, cauliflower ear management can be complicated. The key to preventing the condition is patient education regarding wearing protective headgear while playing contact sports. Complete drainage and a pressure dressing should be applied if an auricular hematoma occurs. Recurrences are common if the hematoma is not managed appropriately. Restoration of the premorbid auricular appearance after developing a cauliflower ear deformity is challenging and requires a specialist surgical team.[34][35]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)

Surgical Repair of Cauliflower Ear. A) Preoperative view. Note the anterior malposition of the helical rim and the excess bulk within the scaphoid fossa. B) The auricular skin is elevated off the underlying cartilage anteriorly and posteriorly via an incision at the junction of the helix and scapha. The perichondrium is scarred and does not elevate easily. C) The skin flaps are replaced, and a quilting suture is passed after reshaping the cartilage with a scalpel, a curette, and a drill. D) Postoperative view at 1 month.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
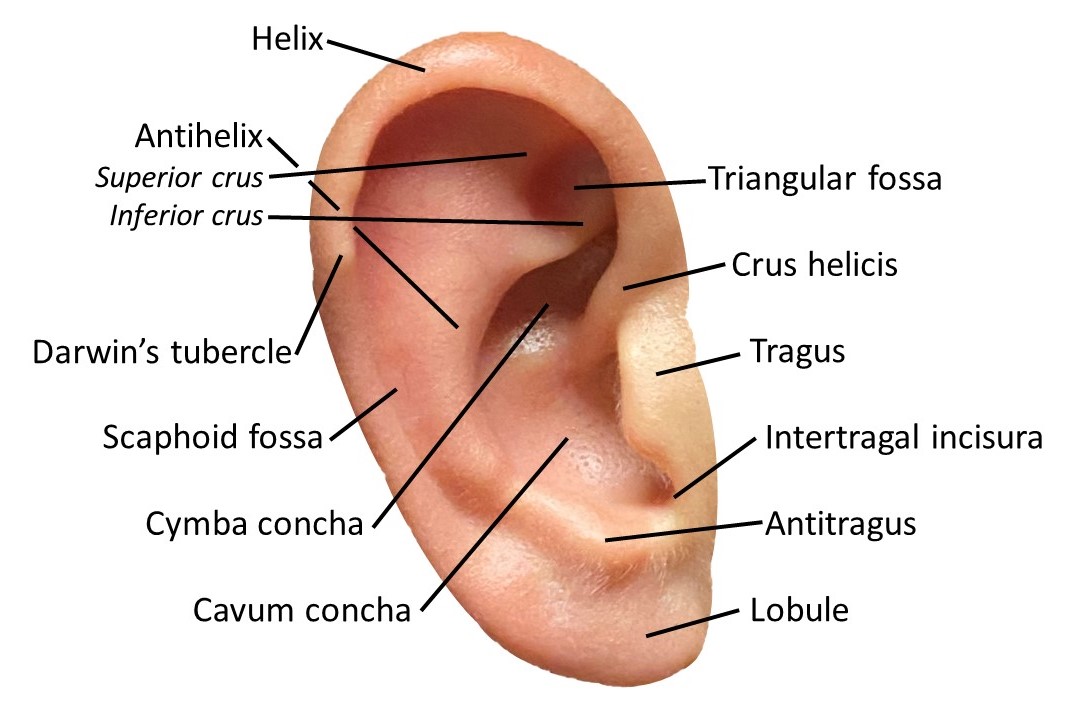
Auricle Surface Anatomy. This image shows the ear auricle's parts, including the helix and its crus, antihelix and its superior and inferior crura, Darwin tubercle, triangular and scaphoid fossae, tragus, conchal cymba and cavum, intertragal incisura, antitragus, and lobule.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Mudry A, Pirsig W. Auricular hematoma and cauliflower deformation of the ear: from art to medicine. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2009 Jan:30(1):116-20. doi: 10.1097/MAO.0b013e318188e905. Epub [PubMed PMID: 18800018]
Mohan V, Bhavani S, Subramanian SK, Maiti A. Calcified cauliflower ear in relapsing polychondritis. BMJ case reports. 2017 Apr 21:2017():. pii: bcr-2017-219424. doi: 10.1136/bcr-2017-219424. Epub 2017 Apr 21 [PubMed PMID: 28432170]
Level 3 (low-level) evidenceIngvaldsen CA, Tønseth KA. Auricular haematoma. Tidsskrift for den Norske laegeforening : tidsskrift for praktisk medicin, ny raekke. 2017 Jan:137(2):105-107. doi: 10.4045/tidsskr.15.1279. Epub 2017 Jan 24 [PubMed PMID: 28127072]
Sand M, Sand D, Brors D, Altmeyer P, Mann B, Bechara FG. Cutaneous lesions of the external ear. Head & face medicine. 2008 Feb 8:4():2. doi: 10.1186/1746-160X-4-2. Epub 2008 Feb 8 [PubMed PMID: 18261212]
Zucchelli E, Birchall M, Bulstrode NW, Ferretti P. Modeling Normal and Pathological Ear Cartilage in vitro Using Somatic Stem Cells in Three-Dimensional Culture. Frontiers in cell and developmental biology. 2020:8():666. doi: 10.3389/fcell.2020.00666. Epub 2020 Jul 28 [PubMed PMID: 32850801]
Pandya NJ. Experimental production of "cauliflower ear" in rabbits. Plastic and reconstructive surgery. 1973 Nov:52(5):534-7 [PubMed PMID: 4745576]
Singh LK, Mamidipalli SS, Das S, Tikka SK, Arora R. Cauliflower ear in late onset psychosis. Asian journal of psychiatry. 2019 Jan:39():6-7. doi: 10.1016/j.ajp.2018.10.025. Epub 2018 Nov 8 [PubMed PMID: 30458404]
Krogmann RJ, Jamal Z, King KC. Auricular Hematoma. StatPearls. 2024 Jan:(): [PubMed PMID: 30285394]
Haik J, Givol O, Kornhaber R, Cleary M, Ofir H, Harats M. Cauliflower ear - a minimally invasive treatment method in a wrestling athlete: a case report. International medical case reports journal. 2018:11():5-7. doi: 10.2147/IMCRJ.S152145. Epub 2018 Jan 18 [PubMed PMID: 29403318]
Level 3 (low-level) evidenceRapini RP, Warner NB. Relapsing polychondritis. Clinics in dermatology. 2006 Nov-Dec:24(6):482-5 [PubMed PMID: 17113965]
Palaniappan V, Kaliaperumal K. Cauliflower Ear in Lepromatous Leprosy. The American journal of tropical medicine and hygiene. 2021 Sep 27:105(6):1444-1445. doi: 10.4269/ajtmh.21-0661. Epub 2021 Sep 27 [PubMed PMID: 34583343]
Chandrakala C, Tharini GK. Cauliflower Ear: A Rare Manifestation of Phaeohyphomycosis. Indian journal of dermatology. 2019 Nov-Dec:64(6):497-498. doi: 10.4103/ijd.IJD_101_18. Epub [PubMed PMID: 31896852]
Nitsch A, Marx H, Fischer CS, Bakir S, Ekkernkamp A, Wassilew GI, Haralambiev L. Prevalence of cauliflower ear in high level judoka. Scientific reports. 2023 Oct 13:13(1):17351. doi: 10.1038/s41598-023-42635-8. Epub 2023 Oct 13 [PubMed PMID: 37833272]
Manninen IK, Blomgren K, Elokiuru R, Lehto M, Mäkinen LK, Klockars T. Cauliflower ear among Finnish high-level male wrestlers and judokas is prevalent and symptomatic deformity. Scandinavian journal of medicine & science in sports. 2019 Dec:29(12):1952-1956. doi: 10.1111/sms.13530. Epub 2019 Aug 16 [PubMed PMID: 31359522]
Ohlsén L, Skoog T, Sohn SA. The pathogenesis of cauliflower ear. An experimental study in rabbits. Scandinavian journal of plastic and reconstructive surgery. 1975:9(1):34-9 [PubMed PMID: 1162288]
Level 3 (low-level) evidencePark C, Lineaweaver WC, Rumly TO, Buncke HJ. Arterial supply of the anterior ear. Plastic and reconstructive surgery. 1992 Jul:90(1):38-44 [PubMed PMID: 1615090]
Ghanem T, Rasamny JK, Park SS. Rethinking auricular trauma. The Laryngoscope. 2005 Jul:115(7):1251-5 [PubMed PMID: 15995516]
Level 3 (low-level) evidenceGreywoode JD, Pribitkin EA, Krein H. Management of auricular hematoma and the cauliflower ear. Facial plastic surgery : FPS. 2010 Dec:26(6):451-5. doi: 10.1055/s-0030-1267719. Epub 2010 Nov 17 [PubMed PMID: 21086231]
Fujiwara M, Suzuki A, Nagata T, Fukamizu H. Cauliflower ear dissection. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2011 Nov:64(11):e279-82. doi: 10.1016/j.bjps.2011.04.018. Epub 2011 May 25 [PubMed PMID: 21612992]
Mashiko T, Minabe T, Shiokawa I, Mineda K, Yoshimura K. Heterotopic ossification in cauliflower ear. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2014 Mar:67(3):e93-4. doi: 10.1016/j.bjps.2013.10.015. Epub 2013 Oct 26 [PubMed PMID: 24184070]
Brown CL, Yilanli M, Rabbitt AL. Child Physical Abuse and Neglect. StatPearls. 2024 Jan:(): [PubMed PMID: 29262061]
Johnson MJ, Fertel H. Elder Abuse. StatPearls. 2024 Jan:(): [PubMed PMID: 32809718]
Shilpa K, Leelavathy B, Lakshmi DV, Divya G. Unilateral Cauliflower Ear due to Leprosy or Trauma - A Diagnostic Challenge. Indian journal of leprosy. 2016 Jul-Sep:88(3):189-192 [PubMed PMID: 30207644]
Noormohammadpour P, Rostami M, Nourian R, Mansournia MA, Sarough Farahani S, Farahbakhsh F, Kordi R. Association Between Hearing Loss And Cauliflower Ear in Wrestlers, a Case Control Study Employing Hearing Tests. Asian journal of sports medicine. 2015 Jun:6(2):e25786. doi: 10.5812/asjsm.6(2)2015.25786. Epub 2015 Jun 20 [PubMed PMID: 26448842]
Level 2 (mid-level) evidenceMandavia R, Kapoor K, Ouyang J, Osmani H. Evaluating ear cartilage piercing practices in London, UK. The Journal of laryngology and otology. 2014 Jun:128(6):508-11. doi: 10.1017/S0022215114001121. Epub 2014 Jun 9 [PubMed PMID: 24909453]
Kravchik L, Ng M, VanHoy TB. Ear Nerve Block. StatPearls. 2024 Jan:(): [PubMed PMID: 30860741]
Kelleher JC, Sullivan JG, Baibak GJ, Dean RK. The wrestler's ear. Plastic and reconstructive surgery. 1967 Dec:40(6):540-6 [PubMed PMID: 6077715]
Vuyk HD, Bakkers EJ. Absorbable mattress sutures in the management of auricular hematoma. The Laryngoscope. 1991 Oct:101(10):1124-6 [PubMed PMID: 1921641]
Roy S, Smith LP. A novel technique for treating auricular hematomas in mixed martial artists (ultimate fighters). American journal of otolaryngology. 2010 Jan-Feb:31(1):21-4. doi: 10.1016/j.amjoto.2008.09.005. Epub 2009 Mar 26 [PubMed PMID: 19944894]
Level 2 (mid-level) evidenceHwang K, Kim CW, Lee SI, Park IS, Kim WC, Loh JJ. Could ionizing radiation forestall cauliflower ear? Annals of plastic surgery. 2001 Feb:46(2):141-5 [PubMed PMID: 11216608]
Yotsuyanagi T, Yamashita K, Urushidate S, Yokoi K, Sawada Y, Miyazaki S. Surgical correction of cauliflower ear. British journal of plastic surgery. 2002 Jul:55(5):380-6 [PubMed PMID: 12372365]
D'Ascanio L, Gostoli E, Ricci G, De Luca P, Latini G, Brenner MJ, Di Stadio A. Modified Valente Technique for Cauliflower Ear: Outcomes in Children at Two-Year Follow-Up : New Surgical Technique for Cauliflower Ear. Aesthetic plastic surgery. 2024 Mar 18:():. doi: 10.1007/s00266-024-03914-5. Epub 2024 Mar 18 [PubMed PMID: 38499875]
Putri IL, Bogari M, Khoirunnisa A, Dhafin FR, Kuswanto D. Surgery of Severe Cauliflower Ear Deformity. Plastic and reconstructive surgery. Global open. 2023 Apr:11(4):e4953. doi: 10.1097/GOX.0000000000004953. Epub 2023 Apr 19 [PubMed PMID: 37091928]
Summers A. Managing auricular haematoma to prevent 'cauliflower ear'. Emergency nurse : the journal of the RCN Accident and Emergency Nursing Association. 2012 Sep:20(5):28-30 [PubMed PMID: 23256352]
Cuesta L, Betlloch I, Bañuls J, Toledo F. "Cauliflower ear" in a teenager: a possible sign of child abuse. Pediatric dermatology. 2012 Mar-Apr:29(2):226-7. doi: 10.1111/j.1525-1470.2011.01416.x. Epub 2011 Dec 9 [PubMed PMID: 22150252]
Level 3 (low-level) evidence