Introduction
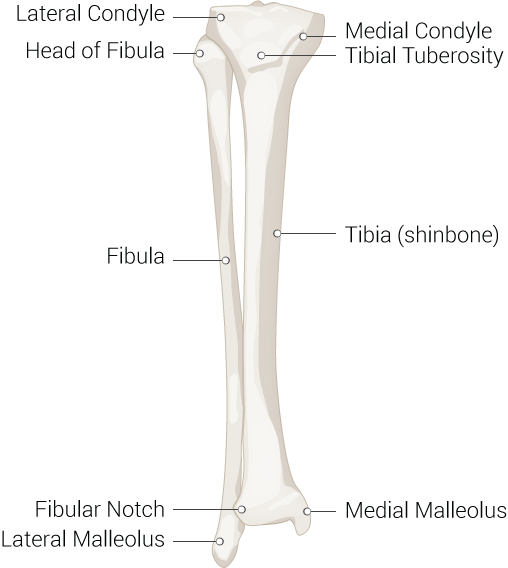
The fibula is a long bone in the lower extremity that is positioned on the lateral side of the tibia. The fibula is much smaller and thinner than the tibia. It is located just behind the tibial head at the knee joint and then runs down the lateral aspect of the leg until it reaches the ankle joint. A ridge on the medial surface of the fibula forms the interosseous border where the fibula is connected to the tibia via the interosseous membrane. This connection forms a syndesmotic joint, meaning it has very little mobility.[1][2][3]
The structure of the fibula can be broken down into the head, neck, shaft, and distal end of the fibula. As the head becomes narrow distally, the fibular neck is formed. The fibular shaft lies distal to the neck and has three surfaces, lateral, medial, and posterior. The shape of the fibular shaft is determined by the muscle attachments. Initially, it is a triangular shape and distally becomes more irregularly shaped. The distal end of the fibula forms the lateral malleolus which articulates with the lateral talus, creating part of the lateral ankle. The posterior and lateral tibia form the posterior and medial malleolus, respectively.
Like the tibia, the fibula is ossified in three areas, in the middle and at either end of the epiphysis. Ossification of the fibula begins in the shaft at around the eighth week of gestation and then extends to either end. The process of ossification is complete by the second decade of life. Both ends of the fibula remain cartilaginous.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
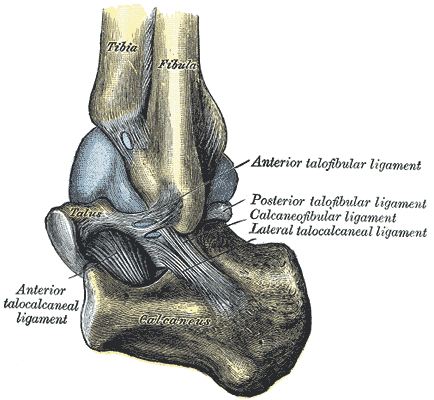
Unlike the tibia, the fibula is not a weight-bearing bone. Its main function is to combine with the tibia and provide stability to the ankle joint. The distal end of the fibula has several grooves for ligament attachments which then stabilize and provide leverage during the ankle movements. The lateral (fibular) collateral ligament attaches to the lateral side of the fibular head. This ligament provides knee stability. However, the fibula itself has a little role in providing knee stability.
Blood Supply and Lymphatics
The blood supply to the fibula is from the fibular artery (also known as the peroneal artery) which has many small branches which supply the diaphysis. The epiphysis and the proximal fibular head are supplied by branches of the anterior tibial artery. The periosteum also receives numerous small branches from the fibular artery and supplies the rest of the bone. It is important to know the blood supply of the fibula because this bone is often used as a graft for reconstruction of the mandible.
Nerves
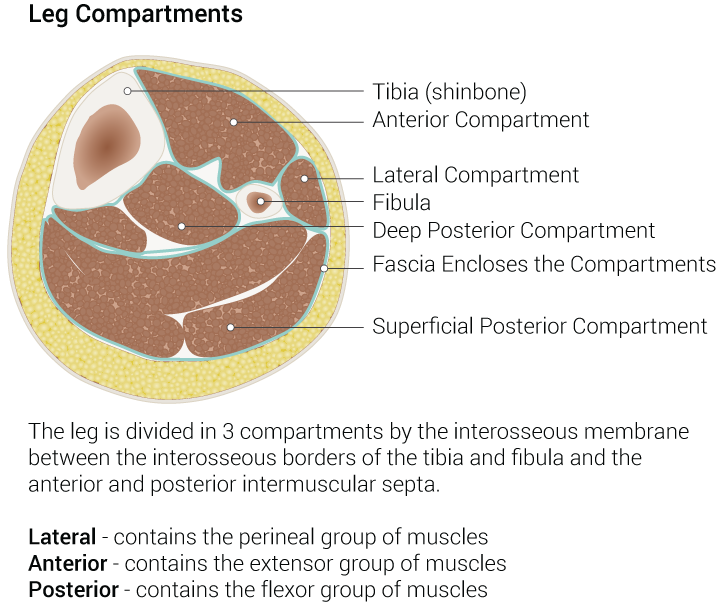
The fibula's lateral surface, deep fascia, and intermuscular septum form the borders of the lower limbs lateral compartment. Within this compartment runs the superficial fibular nerve, which is responsible for plantar flexion and eversion. The fibula's posterior surface, deep fascia, and interosseous membrane form the borders of the lower limbs posterior compartment. The tibial nerve runs through this compartment and is responsible for plantar and digit flexion. The fibula's medial surface partially borders the lower limbs anterior compartment.
Muscles
Many important muscles attach to the fibula which molds the fibular shaft into its unique shape.
- The biceps femoris tendon attaches to the fibular head.
- The fibularis longus and fibularis brevis tendons attach to the lateral fibula.
- The extensor digitorum longus and extensor hallucis longus tendons attach to the medial fibula.
- The fibularis tertius (FT) is a small muscle in the anterior compartment of the leg that inserts on the anterior surface of the distal fibula. FT functions to extend the ankle and evert subtalar joints.
Fibular muscle accessory tendon variations are quite common. The FT muscle can vary in size or be absent 20% of the time. The fibularis quartus muscle is seen in the lateral compartment approximately 12% to 22% of the time.
Surgical Considerations
Fibula bone grafts are the gold standard in mandibular reconstructive surgeries. This is because removing the fibula from its anatomical location will not greatly impact weight bearing, as that is mainly the function of the tibia. Additionally, the fibula is thin and long while maintaining great vascularity. This allows for easy graft uptake and osseointegration of dental implants. When using the fibula as a graft, only the shaft is used, and two ends of the fibula are left intact.[3]
Clinical Significance
Congenitally
There is strong support in recent literature to use the fibular shaft length to estimate infant bone age. This may be a more accurate alternative to the current methods of counting ossification centers or viewing hand/wrist or knee radiographs as means of estimating infant bone age.
Fibular hemimelia or fibular hypoplasia-aplasia is the most frequent long bone deficiency. This causes partial or complete absence of the fibula. This is usually diagnosed at birth when limb-length discrepancy and lack of digits are noted. Additionally, the absence of a lateral malleolus destabilizes the mortise in valgus. Thus, ankle fusion is usually needed.
Neurologically
The proximal end of the fibula has a slightly enlarged prominence which contains a facet that articulates with the lateral condyle of the tibia. Just lateral and posterior to the fibular neck runs the common fibular nerve (also known as the common peroneal nerve), which may become entrapped after trauma, direct injury or during its course near the fibular head. Common fibular nerve entrapment is the most prevalent entrapment neuropathy of the lower extremity. Symptoms may include foot drop and lateral limb sensory deficits, but given the lack of clear symptoms, misdiagnosis is common and may cause a delay in treatment.
Fractures
The fibula can develop an avulsion fracture when there is a sudden contraction of the biceps femoris muscle. This results in a significant pull on the fibula because the biceps femoris tendon attaches to the fibular head.
The distal fibula continues to become the lateral malleolus. The lateral malleolus is significantly more evident than the medial malleolus and can be palpated at the ankle. On the lateral aspect of the ankle, the distal fibula is also prone to fracture (usually spiral), that can occur during forced external rotation of the ankle. Another means of injury occurs during eversion of the foot (outward twisting of the foot) or direct trauma. The resulting fracture from an eversion injury is usually a transverse fracture of the fibula. A clinical decision-making tool called The Ottawa Ankle Rules (OAR) can be used in suspected lateral malleolus injuries. The OAR is beneficial in lessening unnecessary radiographs and are a reliable tool to exclude fractures in children over age 5.
Fibular fractures alone rarely cause compartment syndrome. However, when a tibial plateau fracture is present, there is a higher likelihood that the fibular fracture will contribute to the compartment syndrome. [4]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
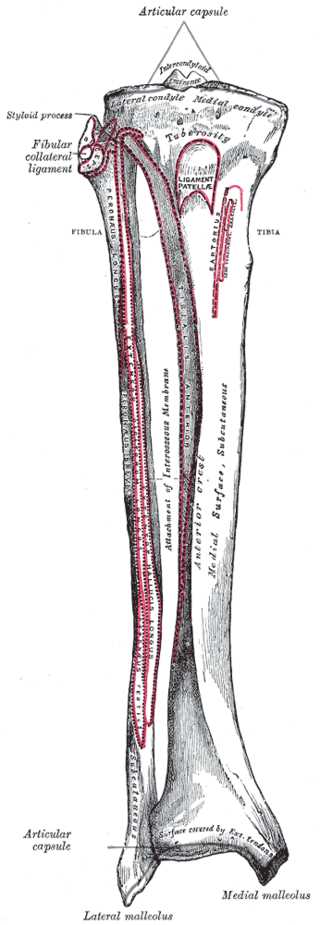
Right Leg Bone Anatomy. Anatomy includes tibia, fibula, styloid process, fibular collateral ligament, ligament patella, tuberosity, sartorius, peroneus longus, extensor, interosseous membrane, anterior crest, hallucis longus, lateral malleolus, and medial malleolus.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Garrett A, Geiger Z. Anatomy, Bony Pelvis and Lower Limb: Calf Deep Peroneal Nerve (Deep Fibular Nerve). StatPearls. 2023 Jan:(): [PubMed PMID: 30252289]
Gupton M, Imonugo O, Terreberry RR. Anatomy, Bony Pelvis and Lower Limb, Knee. StatPearls. 2023 Jan:(): [PubMed PMID: 29763193]
Oberna F, Czuczor M, Füzes A. [Mandibular angle and head reconstruction with fibular free flap]. Magyar onkologia. 2018 Sep 26:62(3):169-174 [PubMed PMID: 30256883]
Kiel J, Kaiser K. Tibial Anterior Compartment Syndrome. StatPearls. 2023 Jan:(): [PubMed PMID: 30085512]