Introduction
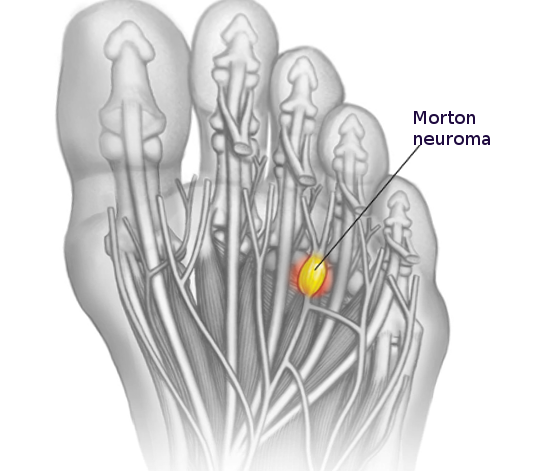
Morton neuroma is a compressive neuropathy of the forefoot interdigital nerve. Neuropathy is mainly due to compression and irritation at the plantar aspect of the transverse intermetatarsal ligament. It is not a true neuroma as the condition is degenerative rather than neoplastic. It is also referred to as Morton metatarsalgia, interdigital neuritis, Morton entrapment, interdigital neuralgia, interdigital neuroma, interdigital nerve compression syndrome, and intermetatarsal neuroma. The most common locations for interdigital neuromas are between the 3rd and 4th metatarsal heads, termed Morton neuroma.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The exact etiological cause of Morton neuroma is not known, but four major hypotheses have been described. The chronic trauma theory, the most widely accepted hypothesis, states that the mechanical effects of walking cause chronic micro-traumas to the intermetatarsal plantar digital nerves, which become compressed between two metatarsal heads and the metatarsophalangeal joints.[4]
The entrapment theory, one of the earliest proposed theories, states that interdigital neuromas occur due to compression of the interdigital nerve against the anterior end of the deep transverse metatarsal ligament and plantar soft tissue structures. The intermetatarsal bursa theory states that bursitis in the intermetatarsal region causes compression and inflammation with subsequent fibrosis of the affected common plantar digital nerve. Interestingly, bursae are close to the neurovascular bundle in the second and third intermetatarsal spaces where Morton neuromas are most common, but Morton neuromas are rare in the fourth intermetatarsal space where the bursa rarely ever contacts the neurovascular bundle.[5] The fourth theory is the ischemic theory, based on histopathological findings of the common plantar digital artery exhibiting degenerative changes prior to the fibrous thickening of the nerve.[6] Common causes include narrow toe-box footwear, hyperextension of the toes in high-heeled shoes, deviation of the toes, inflammation of the intermetatarsal bursa, thickening of the transverse metatarsal ligament, forefoot trauma, high-impact sporting activities, metatarsophalangeal joint pathology, and lipoma.[7][8]
Epidemiology
Morton neuroma is common in middle-aged women, and the incidence is at least five times more common in females when compared to men.[9] The exact incidence is unknown. Rarely are both feet affected. Finding two neuromas on the same foot is common.[10]
Pathophysiology
Morton neuroma is common in the third interspace because it is narrower compared to other spaces. As the common digital nerve to the third space receives branches from both medial and lateral plantar nerves, it has increased thickness and is prone to compression and trauma. Trauma from a crush injury, penetrating injury, thickened transverse metatarsal ligament, enlarged bursa in the interspace, and repetitive trauma from running have all been linked to the development of Morton neuroma. The compression and repetitive trauma to the nerve results in vascular changes, endoneurial edema, and excessive bursal thickening leading to perineural fibrosis.[11]
Histopathology
Grossly there is a fusiform swelling near the bifurcation of the plantar interdigital nerve with thickening of adjacent tenosynovial tissues. Microscopically, the common plantar digital artery displays disruption of the arterial wall, thrombosis, and incomplete recanalization, which are findings that support the ischemic theory.[12] In addition, there is fibrosis surrounding and within the nerves, Schwann cell and fibroblast propagation, and damage to myelinated nerve fibers.
History and Physical
The most common symptoms are plantar pain between metatarsal heads that are aggravated by walking and wearing tight-fitting, high-heeled shoes and relieved by resting and removing shoes. Patients describe the pain as burning, stabbing, or tingling with electric sensations. Some patients describe the sensation as walking on a stone or marble. Numbness between the toes is present in less than half of the patients. With prolonged walking, the pain can radiate to the hindfoot or leg, causing cramps.
Evaluation
Diagnosis is usually based on history and clinical examination. Palpation in the affected space may reproduce the symptoms. Compression of the forefoot in the mediolateral direction while palpating the affected space often results in a significant crunching or clicking feeling, commonly known as the "Mulder's click." Some surgeons inject the affected webbed space with a diagnostic injection of lidocaine. A maximum of 1 ml to 2 ml of the anesthetic agent should be injected. Plain, weight-bearing radiographs should be taken to rule out any bony masses, deformities, subluxation, dislocation, or arthritis. Additionally, gapping of the distal intermetatarsal space and/or divergence of adjacent digits may be noted, and this is known as Sullivan's sign.[13]
A radio-opaque foreign body can also be visualized. An ultrasound scan performed by an experienced radiologist can be a useful diagnostic aid. A steroid injection under ultrasound guidance can be given at the same time. MRI can be obtained based on the clinical scenario, especially to rule out other pathologies.[8][14] MRI imaging demonstrates a dumbell-shaped soft tissue lesion within the intermetatarsal space. The T1 signal is often low, the T2 signal is frequently low or intermediate, and enhancement is variable. The sonographic evaluation also similarly demonstrates a noncompressible dumbell-shaped soft tissue lesion with hypoechogenicity within the intermetatarsal space. A "Mulder's click" can potentially be elicited on palpation with the probe.
Treatment / Management
Non-operative Treatment
Wearing a wide, soft-soled, laced shoe with a low heel can effectively relieve pressure on the nerve. Some surgeons recommend a firm-soled shoe instead. Soft metatarsal support with a metatarsal pad, or neuroma pad, placed just proximal to the metatarsal heads, can help to spread the metatarsal heads and relieve mechanical pressure on the neuroma. In the presence of synovitis, instability, or deformity of the toe, a Budin splint or canopy toe strapping can decrease secondary neuralgia. Anti-inflammatory medications, tricyclic antidepressants such as amitriptyline, and anti-seizure medications such as gabapentin can be administered to lessen the severity of related nerve symptoms. Blind or ultrasound-guided steroid injections can occasionally help, but their effect is rarely long-lasting. Atrophy of the subcutaneous fat and plantar fat pad, discoloration of the skin, and disruption of the joint capsule adjacent to the injected site causing deformity of the toe, are some of the reported side effects. Radiofrequency ablation, cryotherapy, and alcohol nerve injections have been proposed as less invasive and more conservative methods of treating neuromas.[1][15][16](A1)
Surgical Treatment
If non-operative management fails, then surgery is indicated to treat recalcitrant cases. The neuroma is excised using a dorsal or plantar approach. The dorsal approach is better tolerated by patients as the plantar scar can be painful. A 3 cm to 4 cm incision is made just proximal to the involved webspace in the midline to prevent injury to the dorsal cutaneous nerves. The incision is deepened to the transverse metatarsal ligament, which is transected. The common digital nerve is identified in the proximal portion of the wound and is traced distally to its bifurcation, and any soft tissue adhesions, if present, are released around the nerve. At this point, nerve decompression or neurolysis has been performed, and some surgeons will end the dissection here without any further intervention to the nerve itself. Previous reports in the literature noted satisfactory results with decompression alone.[17] (B2)
To intervene on the nerve, the common digital nerve is cut proximal to the metatarsal heads and then traced distally past the bifurcation, where both branches are transected. Some surgeons suture the cut ends of the nerve to the side of the metatarsal or one of the intrinsic muscles to prevent the formation of a painful stump neuroma. As little plantar fat as possible should be removed. A postoperative shoe is worn till the stitches are removed at about 7 to 14 days, and a compressive wrap is used for 2 to 6 weeks.
The plantar incision is mainly reserved for recurrent neuromas or when the patient has a proximal focal tender trigger point for neuralgia. It decreases the rate of missed neuroma, and it does not require an incision of the transverse metatarsal ligament. The plantar approach permits a more direct exposure of the nerve and allows its more proximal resection. The artery and vein can be better visualized and preserved. The main disadvantages are painful plantar scars and plantar keratosis in about 5% of cases.[18]
Differential Diagnosis
- Metatarsal stress fracture
- Hammertoe
- Rheumatoid or osteoarthritis
- Malignancy
- Ganglion cyst
Prognosis
Conservative Approaches
Conservative approaches to treatment have shown varying degrees of effectiveness.[19][20] Change of footwear, activity modification, and pharmacotherapy are often used to minimize pain and lessen symptoms. Employing multiple strategies has shown to be effective.[21] A systematic review and meta-analysis of non-surgical approaches were performed, comparing both non-invasive (manipulation/mobilization, wider footwear and metatarsal padding, extracorporeal shockwave therapy, and varus/valgus wedge) and invasive (corticosteroid injections, sclerosing injections, radiofrequency ablation, cryo-neurolysis, and botox injection) methods. The analysis found corticosteroid injections and manipulation/mobilization to have the strongest evidence for pain reduction.[22]
Surgical Cases
Various papers have investigated success rates after surgery.[23][24][25][26] Kasparek et al. evaluated 81 patients and noted excellent subjective results in 45% of patients and good results in 32% of patients. Approximately 8% of patients had noted a poor result.[23] The question of whether to perform neurolysis versus a neurectomy is debatable, but one study noted that neurolysis yields satisfactory results overall, but in the presence of a pseudo-tumor or considerably thickened nerve, a neurectomy may be a more viable option.[27]
A systematic review and meta-analysis of 35 articles, including 2998 patients with Morton neuromas, compared injection therapy (both alcohol and non–alcohol), neurolysis, and neurectomy. The analysis found that 43% of patients noted complete pain relief after injection therapy, 68% were pain-free after neurolysis, and 74% were pain-free after neurectomy.[28]
Complications
- Chronic pain (chronic regional pain syndrome)
- Recurrence of the deformity due to inadequate excision or converting a Morton neuroma into a true neuroma
- Complications related to surgery (infection, pain, bleeding)
- Complications associated with corticosteroid injections (skin/fat pad atrophy, skin discoloration)
Deterrence and Patient Education
Managing patient expectations is key. The patient should be educated about the variable success rates of physiotherapy, activity modification, using appropriate footwear, and the role of other modalities such as injections and cryotherapy. When surgery is being considered, a significant minority of patients report worsening pain after surgery.[23]
Pearls and Other Issues
If there has been inadequate proximal resection or failure of the nerve to retract, the neural stump can become enlarged and bulbous. The neural stump may also adhere to the adjacent bone and soft tissue, causing traction neuritis. It can cause pain and tenderness in the webbed space of previous neuroma excision at or proximal to the metatarsal heads. The clinical examination, investigations, and non-operative management are the same as for a primary neuroma. For surgery, both dorsal and plantar incisions are recommended. The dorsal incision has to be extended proximally to visualize the stump, but sometimes, exposure can be difficult. The plantar approach provides better exposure so that the nerve is identified and resected easily.
Enhancing Healthcare Team Outcomes
Morton neuroma is best managed non-surgically with an interprofessional team of healthcare professionals, including a podiatrist, orthopedic surgeon, sports physician, nurse practitioner, and primary care provider. The patient may require pain medications, but the key is changes in shoe wear. The nurse should encourage the patient to wear appropriate, well-padded, non-constrictive shoewear. Obese patients may benefit from weight loss, so a dietary consult is appropriate. The patient may benefit from physical therapy and the use of warm compresses and ice to ease the pain.[29][30] [Level 5]
Outcomes
Most patients with Morton neuroma have a good recovery with non-surgical treatment. A few patients may require surgery if the neuroma is localized and can be excised. However, even after surgery, the recurrence rate of neuroma and/or pain is very high. The key is to change footwear and lose weight.[31][32] [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Ruiz Santiago F,Prados Olleta N,Tomás Muñoz P,Guzmán Álvarez L,Martínez Martínez A, Short term comparison between blind and ultrasound guided injection in morton neuroma. European radiology. 2018 Jul 31 [PubMed PMID: 30062527]
Ganguly A,Warner J,Aniq H, Central Metatarsalgia and Walking on Pebbles: Beyond Morton Neuroma. AJR. American journal of roentgenology. 2018 Apr [PubMed PMID: 29470159]
Lorenzon P,Rettore C, Mechanical Metatarsalgia as a Risk Factor for Relapse of Morton's Neuroma After Ultrasound-Guided Alcohol Injection. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2018 Sep - Oct [PubMed PMID: 29779991]
Kim JY,Choi JH,Park J,Wang J,Lee I, An anatomical study of Morton's interdigital neuroma: the relationship between the occurring site and the deep transverse metatarsal ligament (DTML). Foot [PubMed PMID: 17880876]
Bossley CJ,Cairney PC, The intermetatarsophalangeal bursa--its significance in Morton's metatarsalgia. The Journal of bone and joint surgery. British volume. 1980 May; [PubMed PMID: 7364832]
NISSEN KI, Plantar digital neuritis; Morton's metatarsalgia. The Journal of bone and joint surgery. British volume. 1948 Feb; [PubMed PMID: 18864949]
Di Caprio F,Meringolo R,Shehab Eddine M,Ponziani L, Morton's interdigital neuroma of the foot: A literature review. Foot and ankle surgery : official journal of the European Society of Foot and Ankle Surgeons. 2018 Apr [PubMed PMID: 29409221]
Edenfield KM,Michaudet C,Nicolette GW,Carek PJ, Foot and Ankle Conditions: Midfoot and Forefoot Conditions. FP essentials. 2018 Feb [PubMed PMID: 29381043]
Santiago FR,Muñoz PT,Pryest P,Martínez AM,Olleta NP, Role of imaging methods in diagnosis and treatment of Morton's neuroma. World journal of radiology. 2018 Sep 28 [PubMed PMID: 30310543]
LiMarzi GM,Scherer KF,Richardson ML,Warden DR 4th,Wasyliw CW,Porrino JA,Pettis CR,Lewis G,Mason CC,Bancroft LW, CT and MR Imaging of the Postoperative Ankle and Foot. Radiographics : a review publication of the Radiological Society of North America, Inc. 2016 Oct [PubMed PMID: 27726748]
Naraghi R,Bremner A,Slack-Smith L,Bryant A, The relationship between foot posture index, ankle equinus, body mass index and intermetatarsal neuroma. Journal of foot and ankle research. 2016 [PubMed PMID: 27980684]
Jain S,Mannan K, The diagnosis and management of Morton's neuroma: a literature review. Foot [PubMed PMID: 23811947]
Mak MS,Chowdhury R,Johnson R, Morton's neuroma: review of anatomy, pathomechanism, and imaging. Clinical radiology. 2021 Mar; [PubMed PMID: 33168237]
Naraghi R,Bremner A,Slack-Smith L,Bryant A, Radiographic Analysis of Feet With and Without Morton's Neuroma. Foot [PubMed PMID: 27837053]
Masala S,Cuzzolino A,Morini M,Raguso M,Fiori R, Ultrasound-Guided Percutaneous Radiofrequency for the Treatment of Morton's Neuroma. Cardiovascular and interventional radiology. 2018 Jan [PubMed PMID: 28956110]
Lizano-Díez X,Ginés-Cespedosa A,Alentorn-Geli E,Pérez-Prieto D,González-Lucena G,Gamba C,de Zabala S,Solano-López A,Rigol-Ramón P, Corticosteroid Injection for the Treatment of Morton's Neuroma: A Prospective, Double-Blinded, Randomized, Placebo-Controlled Trial. Foot [PubMed PMID: 28617064]
Level 1 (high-level) evidenceMischitz M,Zeitlinger S,Mischlinger J,Rab M, Nerve decompression according to A.L. Dellon in Morton's neuroma - A retrospective analysis. Journal of plastic, reconstructive [PubMed PMID: 32171681]
Level 2 (mid-level) evidenceLee J,Kim J,Lee M,Chu I,Lee S,Gwak H, Morton's Neuroma (Interdigital Neuralgia) Treated with Metatarsal Sliding Osteotomy. Indian journal of orthopaedics. 2017 Nov-Dec [PubMed PMID: 29200487]
Rasmussen MR,Kitaoka HB,Patzer GL, Nonoperative treatment of plantar interdigital neuroma with a single corticosteroid injection. Clinical orthopaedics and related research. 1996 May [PubMed PMID: 8620640]
Level 2 (mid-level) evidenceEspinosa N,Seybold JD,Jankauskas L,Erschbamer M, Alcohol sclerosing therapy is not an effective treatment for interdigital neuroma. Foot & ankle international. 2011 Jun [PubMed PMID: 21733418]
Level 2 (mid-level) evidenceChemical characterization of isocyanate-protein conjugates., Tse CS,Pesce AJ,, Toxicology and applied pharmacology, 1979 Oct [PubMed PMID: 16045848]
Level 1 (high-level) evidenceMatthews BG,Hurn SE,Harding MP,Henry RA,Ware RS, The effectiveness of non-surgical interventions for common plantar digital compressive neuropathy (Morton's neuroma): a systematic review and meta-analysis. Journal of foot and ankle research. 2019; [PubMed PMID: 30809275]
Level 1 (high-level) evidenceStudies on the tissue-disposition and fate of N-[14C]ethyl-N-nitrosourea in mice., Johansson-Brittebo E,Tjälve H,, Toxicology, 1979 Aug [PubMed PMID: 23851648]
Level 2 (mid-level) evidenceA method for removing precipitate from ultrathin sections resulting from glutaraldehyde-osmium tetroxide fixation., Ellis EA,Anthony DW,, Stain technology, 1979 Sep [PubMed PMID: 22134434]
Level 2 (mid-level) evidenceEffect of phenobarbital on cerebral energy state and metabolism. Enzymatic activities., Benzi G,Agnoli A,Dagani F,Ruggieri S,Villa RF,, Stroke, 1979 Nov-Dec [PubMed PMID: 19802669]
Level 2 (mid-level) evidenceLocal versus regional procurement and distribution of granulocytes., Friedenberg WR,Marx JJ Jr,Weir GJ,Banerjee TK,Chang S,Becker G,, Transfusion, 1979 Nov-Dec [PubMed PMID: 18594745]
Villas C,Florez B,Alfonso M, Neurectomy versus neurolysis for Morton's neuroma. Foot [PubMed PMID: 18549753]
Level 2 (mid-level) evidenceLu VM,Puffer RC,Everson MC,Gilder HE,Burks SS,Spinner RJ, Treating Morton's neuroma by injection, neurolysis, or neurectomy: a systematic review and meta-analysis of pain and satisfaction outcomes. Acta neurochirurgica. 2021 Feb; [PubMed PMID: 32056015]
Level 1 (high-level) evidencePark YH,Jeong SM,Choi GW,Kim HJ, The role of the width of the forefoot in the development of Morton's neuroma. The bone [PubMed PMID: 28249977]
Richardson DR,Dean EM, The recurrent Morton neuroma: what now? Foot and ankle clinics. 2014 Sep [PubMed PMID: 25129354]
Habashy A,Sumarriva G,Treuting RJ, Neurectomy Outcomes in Patients With Morton Neuroma: Comparison of Plantar vs Dorsal Approaches. The Ochsner journal. 2016 Winter [PubMed PMID: 27999504]
Bucknall V,Rutherford D,MacDonald D,Shalaby H,McKinley J,Breusch SJ, Outcomes following excision of Morton's interdigital neuroma: a prospective study. The bone [PubMed PMID: 27694592]