Introduction
Dextrocardia is a rare congenital disorder in which the heart resides on the right side of the thoracic cavity (see Image. Dextrocardia, Chest Radiograph). This condition is often associated with other development anomalies and, in most cases, is diagnosed incidentally. Dextrocardia can occur by itself or be accompanied by a reversal in the position of other organs (termed situs inversus totalis).[1] Dextrocardia also involves a change in the orientation of the heart, with its base to the apex axis being directed to the right, in contrast to the normal heart orientation, where the apex is directed to the left. This change in orientation differentiates it from cardiac dextroposition, where the heart is displaced to the right side due to extracardiac causes, such as a diaphragmatic hernia, right pneumonectomy, or right lung hypoplasia.[2] In typical dextrocardia, the intracardiac anatomy is also reversed, called situs inversus (see Image. Situs Inversus, Magnetic Resonance Image). When dextrocardia is associated with a normal position of other thoracoabdominal structures, the condition is called situs solitus.[3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The exact etiology of dextrocardia is unknown. However, it is thought to be secondary to the abnormal position of the organs during embryonic development. Kartagener syndrome is an inherited ciliary motility disorder caused by autosomal recessive mutation and is associated with chronic sinusitis, bronchiectasis, and dextrocardia.[4] Heterotaxy is another inherited condition that leads to malposition of internal organs and vessels and is caused by a lateralization defect during embryonic development.[5] Individuals with heterotaxy might also have other associated congenital conditions involving the abdominal organs, intestinal malrotation, systemic venous abnormalities, anomalous pulmonary venous connections, and asplenia.[6]
Epidemiology
Dextrocardia is a very rare condition, and studies have revealed incidence rates of dextrocardia to be around 1 in 12,000 pregnancies.[7] Kartagener syndrome has an incidence rate of about 1 in 30,000 live births, and situs inversus totalis was seen in around 50% of patients with primary ciliary dyskinesia.[8] Isolated dextrocardia was seen in 0.6% of patients with primary ciliary dyskinesia.[9] There has been no ethnic or gender-related predilection described for dextrocardia.
Pathophysiology
Dextrocardia occurs as a result of abnormalities in the embryological development of the heart. The heart is the first organ to develop in an embryo. The fetal heart develops from an embryonic heart tube, formed by the fusion of the endocardial tubes. The heart tube attaches to the cranial aspect of the arterial trunk, and the caudal aspect is connected to the venous channels. Once the heart tube is formed, the next important step in developing the heart is looping. Looping determines the position of the ventricle in relationship to the atria. The heart tube may loop to the right (termed as D-loop) or loop to the left (termed as L-loop). With a D-loop, the morphologic right ventricle lies to the right of the left ventricle, whereas with an L-loop, the morphologic right ventricle is positioned left of the left ventricle.[10][11][12] If a D-bulboventricular loop fails to migrate into the left hemithorax, it can result in dextrocardia with the heart in the right hemithorax. Similarly, if an L-bulboventricular loop completes the rotation in the right hemithorax, the heart can be situated in the right hemithorax. The circumstances leading to these aberrations in embryonic development are not entirely clear; however, an association with a defect in dynein or ciliary motility has been implicated.[13]
History and Physical
Dextrocardia by itself (also termed as isolated dextrocardia) is asymptomatic, whereas dextrocardia with situs inversus and Kartagener syndrome can have a multitude of symptoms depending on the accompanying abnormalities. The history of these patients might reveal the following symptoms:
- Cyanosis
- Dyspnea
- Failure to thrive
- Fatigue
- Jaundice
- Pallor
- Decreased exercise tolerance
- Repeated sinus or lung infections
- Hydrocephalus
- Arrhythmias, especially atrioventricular blocks
- Intestinal obstruction [14][15][16]
The physical examination of a patient with dextrocardia might reveal cyanosis, clubbing, a prominent apical impulse on the right side of the chest, and easily audible heart sounds on the right side of the chest.
Evaluation
Dextrocardia is often diagnosed incidentally on the routine radiological examination, which reveals an abnormal location of the heart. Electrocardiogram (EKG) can also reveal the presence of dextrocardia as evidenced by right axis deviation, inversion of all complexes in lead I, upright P-wave in augmented vector left, and an absent R-wave progression in the anterior leads.[17] Limb reversal might produce similar EKG findings; however, with a normal EKG pattern in the precordial leads. An echocardiogram, computed tomography (CT) scan, and magnetic resonance imaging (MRI) of the chest might help evaluate for dextrocardia and associated anomalies.[18][19] Nasal brush biopsy and nasal nitric oxide measurements are diagnostic tests for Kartagener syndrome.[20] CT scan of the chest might reveal bronchiectasis and dextrocardia in these patients. Genetic testing and electron microscopy are other available modalities to confirm the diagnosis of primary ciliary dyskinesia.
Treatment / Management
Most patients with dextrocardia are asymptomatic and lead a normal life. Managing dextrocardia varies depending on the presence of other congenital anomalies. In patients who have other associated cardiac malformations, such as defects of the walls of the heart, malposition of blood vessels, Tetralogy of Fallot, septal defects, and severe valvular abnormalities, surgical reconstruction might need to be considered.[21][22](B3)
- Patients with heart blocks and abnormalities of the cardiac electrical system need to be evaluated for pacemaker placement.[23]
- Although there is no cure for primary ciliary dyskinesia available at the moment, management for these patients should involve mucolytics and expectorants to clear the secretions.
- Antibiotics might be required to fight off respiratory illness due to bacterial infections, especially in patients with accompanying asplenia.[24]
- In patients with severe bronchiectasis affecting the quality of life, lung resection surgery should be considered.[25]
- Neonates may present with intestinal obstruction, requiring surgical management to prevent life-threatening complications.[26]
- Patients with dextrocardia and complex congenital heart malformations might require heart transplantation with the reconstruction of the venous pathways to accommodate a normal donor heart.[27] (B3)
Differential Diagnosis
The differential diagnosis for a heart located on the right side of the thoracic cavity is very narrow. However, dextrocardia must be differentiated from:
- Cardiac dextroposition: The heart is displaced to the right side as a result of extracardiac causes, such as a diaphragmatic hernia, right pneumonectomy, or right lung hypoplasia.
- Kartagener syndrome: Dextrocardia situs inversus is accompanied by primary ciliary dyskinesia.
- Dextroversion: The heart is abnormally positioned to the right and rotated.
- Transposition of the great vessels: The major vessels of the heart connect in reverse with a reversal of the heart chambers.
- Heterotaxy: Mirrored internal organs do not develop or function properly.
- Endocardial cushion defect
Prognosis
The prognosis of patients with dextrocardia depends on the presence or absence of other accompanying congenital defects and the type of congenital anomalies. As mentioned, patients with isolated dextrocardia have a normal lifespan without complications. Newborns with dextrocardia and asplenia are easily susceptible to bacterial infections (especially infections from encapsulated organisms such as Streptococcus pneumoniae, Haemophilus influenzae, and Meningococcus) and life-threatening bacteremia; these patients might need to be on antibiotic prophylaxis.
Complications
Complications of dextrocardia include:
- Failure to thrive
- Respiratory failure
- Congestive heart failure
- Severe infections, especially from encapsulated organisms
- Infertility in males with Kartagener syndrome
- Recurrent sinusitis and pneumonia
- Intestinal obstruction due to malrotation
Consultations
Genetic counseling may be helpful for patients and their affected families to understand more about the disease and its associated conditions.
Deterrence and Patient Education
Dextrocardia is a clinical condition characterized by the location of the heart on the right side of the chest cavity. Though isolated dextrocardia is a benign condition, it can often be associated with other congenital anomalies, which can lead to several problems, such as failure to thrive, recurrent infections, and breathing difficulties in newborns and neonates. Adults with dextrocardia might also have accompanying infertility. Upon suspicion, a thorough evaluation that involves imaging and genetic analysis is necessary to assess for other accompanying abnormalities.
Enhancing Healthcare Team Outcomes
Though not a common occurrence, understanding the incidence, presentation, etiology, and management of dextrocardia is essential for all clinicians; identification of this disorder might be pivotal to recognizing rare presentations of Kartagener syndrome or heterotaxy. Due to the possibility of other congenital anomalies associated with dextrocardia, diagnosing dextrocardia could be a bridge to diagnosing other cardiac abnormalities. Due to the advances in medicine, patients with complex congenital heart disease often live a long, healthy life. Understanding the pathophysiology behind this condition is vital for anesthetic considerations when these patients undergo cardiac or noncardiac surgery. Thus, awareness and knowledge about dextrocardia and its implications are essential in improving patient care. Patients with dextrocardia benefit from care by an interprofessional team of primary care clinicians, radiologists, cardiologists, cardiothoracic surgeons, and infectious disease specialists.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
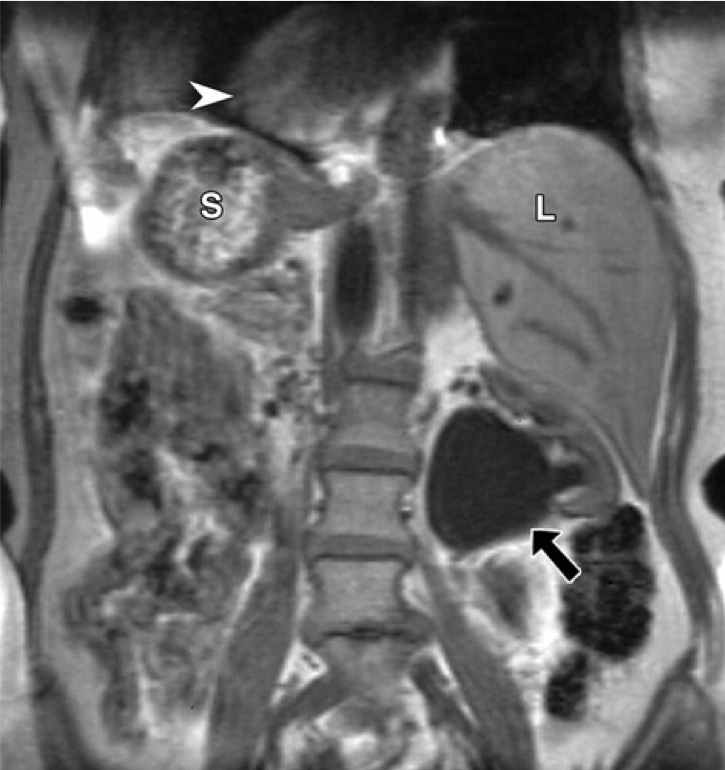
Situs Inversus, Magnetic Resonance Image. This image shows situs Inversus in a 56-year-old woman with left flank pain. Coronal unenhanced fat-suppressed T1-weighted MR image of the abdomen reveals a left ureteropelvic junction obstruction (arrow). The liver (L) is located in the left upper quadrant, and the stomach (S) and spleen (not shown) are located in the right upper quadrant; dextrocardia (arrowhead) is also noted.
Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2022;22(6):1439-1456. doi: 10.1148/rg.226025016.
References
Channabasappa SM, Mohan HS, Sarma J. A patient with situs inversus totalis presenting for emergency laparoscopic appendectomy: Consideration for safe anesthetic management. Anesthesia, essays and researches. 2013 Jan-Apr:7(1):127-9. doi: 10.4103/0259-1162.114019. Epub [PubMed PMID: 25885734]
GRANT RP. The syndrome of dextroversion of the heart. Circulation. 1958 Jul:18(1):25-36 [PubMed PMID: 13547381]
Leung AK, Robson WL. Dextrocardia with situs [corrected] solitus. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2006 Aug 1:175(3):244 [PubMed PMID: 16880440]
Level 3 (low-level) evidenceQueiroz RM, Filho FB. Kartagener's syndrome. The Pan African medical journal. 2018:29():160. doi: 10.11604/pamj.2018.29.160.14927. Epub 2018 Mar 19 [PubMed PMID: 30050624]
Kim SJ. Heterotaxy syndrome. Korean circulation journal. 2011 May:41(5):227-32. doi: 10.4070/kcj.2011.41.5.227. Epub 2011 May 31 [PubMed PMID: 21731561]
Wolla CD, Hlavacek AM, Schoepf UJ, Bucher AM, Chowdhury S. Cardiovascular manifestations of heterotaxy and related situs abnormalities assessed with CT angiography. Journal of cardiovascular computed tomography. 2013 Nov-Dec:7(6):408-16. doi: 10.1016/j.jcct.2013.11.008. Epub 2013 Nov 7 [PubMed PMID: 24331937]
Bohun CM, Potts JE, Casey BM, Sandor GG. A population-based study of cardiac malformations and outcomes associated with dextrocardia. The American journal of cardiology. 2007 Jul 15:100(2):305-9 [PubMed PMID: 17631088]
Level 2 (mid-level) evidenceGupta S, Handa KK, Kasliwal RR, Bajpai P. A case of Kartagener's syndrome: Importance of early diagnosis and treatment. Indian journal of human genetics. 2012 May:18(2):263-7. doi: 10.4103/0971-6866.100787. Epub [PubMed PMID: 23162311]
Level 3 (low-level) evidenceKennedy MP, Omran H, Leigh MW, Dell S, Morgan L, Molina PL, Robinson BV, Minnix SL, Olbrich H, Severin T, Ahrens P, Lange L, Morillas HN, Noone PG, Zariwala MA, Knowles MR. Congenital heart disease and other heterotaxic defects in a large cohort of patients with primary ciliary dyskinesia. Circulation. 2007 Jun 5:115(22):2814-21 [PubMed PMID: 17515466]
Level 2 (mid-level) evidencePerloff JK. The cardiac malpositions. The American journal of cardiology. 2011 Nov 1:108(9):1352-61. doi: 10.1016/j.amjcard.2011.06.055. Epub 2011 Aug 20 [PubMed PMID: 21861958]
De la Cruz MV, Anselmi G, Munos-Castellanos L, Nadal-Ginard B, Munoz-Armas S. Systematization and embryological and anatomical study of mirror-image dextrocardias, dextroversions, and laevoversions. British heart journal. 1971 Nov:33(6):841-53 [PubMed PMID: 5120229]
Angelini P. Embryology and congenital heart disease. Texas Heart Institute journal. 1995:22(1):1-12 [PubMed PMID: 7787459]
Level 3 (low-level) evidenceFarraj KL, Zeltser R. Embryology, Heart Tube. StatPearls. 2025 Jan:(): [PubMed PMID: 29763109]
Arunabha DC, Sumit RT, Sourin B, Sabyasachi C, Subhasis M. Kartagener's syndrome: a classical case. Ethiopian journal of health sciences. 2014 Oct:24(4):363-8 [PubMed PMID: 25489202]
Level 3 (low-level) evidenceMaldjian PD, Saric M. Approach to dextrocardia in adults: review. AJR. American journal of roentgenology. 2007 Jun:188(6 Suppl):S39-49; quiz S35-8 [PubMed PMID: 17515336]
Dilorenzo M, Weinstein S, Shenoy R. Tetralogy of fallot with dextrocardia and situs inversus in a 7-year-old boy. Texas Heart Institute journal. 2013:40(4):481-3 [PubMed PMID: 24082385]
Level 3 (low-level) evidenceYusuf SW, Durand JB, Lenihan DJ, Swafford J. Dextrocardia: an incidental finding. Texas Heart Institute journal. 2009:36(4):358-9 [PubMed PMID: 19693317]
Level 3 (low-level) evidenceHuhta JC, Hagler DJ, Seward JB, Tajik AJ, Julsrud PR, Ritter DG. Two-dimensional echocardiographic assessment of dextrocardia: a segmental approach. The American journal of cardiology. 1982 Dec:50(6):1351-60 [PubMed PMID: 7148713]
Esmaeil H, Al-Fadhli J, Dashti A, Al-Sarraf N. Ischemic mitral regurgitation in a patient with dextrocardia and situs inversus totalis. Journal of surgical case reports. 2019 Nov:2019(11):rjz329. doi: 10.1093/jscr/rjz329. Epub 2019 Nov 20 [PubMed PMID: 31768245]
Level 3 (low-level) evidenceKapania EM, Stern BM, Sharma G. Ciliary Dysfunction. StatPearls. 2025 Jan:(): [PubMed PMID: 28846277]
Ji YQ, Sun PW, Hu JX. Diagnosis and surgical treatment of congenital dextrocardia. Di 1 jun yi da xue xue bao = Academic journal of the first medical college of PLA. 2002 Jun:22(6):536-8 [PubMed PMID: 12297479]
NARA Y, ITOH T, KAMADA K, OHSAWA T, WADA J. A CASE OF INTERVENTRICULAR SEPTAL DEFECT WITH DEXTROCARDIA AND SITUS INVERSUS TREATED BY SURGERY. Japanese circulation journal. 1963 Sep:27():663-7 [PubMed PMID: 14045014]
Level 3 (low-level) evidenceGuo G, Yang L, Wu J, Sun L. Implantation of VVI pacemaker in a patient with dextrocardia, persistent left superior vena cava, and sick sinus syndrome: A case report. Medicine. 2017 Feb:96(5):e6028. doi: 10.1097/MD.0000000000006028. Epub [PubMed PMID: 28151908]
Level 3 (low-level) evidence. Prevention and therapy of bacterial infections for children with asplenia or hyposplenia. Paediatrics & child health. 1999 Sep:4(6):417-31 [PubMed PMID: 20212952]
Lin H, Cao Z, Zhao X, Ye Q. Left middle lobectomy for bronchiectasis in a patient with Kartagener syndrome: a case report. Journal of cardiothoracic surgery. 2016 Mar 9:11():37. doi: 10.1186/s13019-016-0426-y. Epub 2016 Mar 9 [PubMed PMID: 26960394]
Level 3 (low-level) evidenceGupta R, Soni V, Valse PD, Goyal RB, Gupta AK, Mathur P. Neonatal intestinal obstruction associated with situs inversus totalis: two case reports and a review of the literature. Journal of medical case reports. 2017 Sep 18:11(1):264. doi: 10.1186/s13256-017-1423-z. Epub 2017 Sep 18 [PubMed PMID: 28918753]
Level 3 (low-level) evidenceChang YL, Wei J, Chang CY, Chuang YC, Sue SH. Cardiac transplantation in situs inversus: two cases reports. Transplantation proceedings. 2008 Oct:40(8):2848-51. doi: 10.1016/j.transproceed.2008.07.115. Epub [PubMed PMID: 18929882]
Level 3 (low-level) evidence