Introduction
Patellar instability is a spectrum of conditions ranging from intermittent subluxations to dislocation. Patients typically present with obvious deformity and an inability to extend the knee. The recurrence rate following a first-time dislocation is around 15-60%.[1] Generalized patellar instability is thought to represent up to 3% of clinical presentations involving the knee. In most cases, it can be managed conservatively with physiotherapy and bracing, except in the presence of a fracture or recurrent episodes.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Acute patellar dislocations typically occur as a result of trauma, usually a non-contact twisting injury to the knee, or from a direct blow to the medial aspect of the knee. A common mechanism is external tibial rotation with the foot fixed on the ground. Patellar dislocations can also occur in patients with generalized ligamentous laxity. However, those patients mostly tend to have recurrent subluxations of their patella as opposed to a frank dislocation.
Anatomic variations such as patella alta and trochlear dysplasia can predispose individuals to patellar dislocation. Ligamentous laxity is more commonly seen in females, or secondary to connective tissue disorders such as Marfan Syndrome or Ehlers-Danlos, increases the risk of dislocation. Muscular imbalance, particularly weakness of the vastus medialis oblique also plays a role in patellar instability.
Habitual dislocations are characterized by painless dislocations every time the knee flexes, which is usually a result of abnormal tightness of the vastus lateralis muscle and the iliotibial band.
Congenital dislocations can also occur, most commonly in patients with Down syndrome; this is the result of a small patella in combination with a hypoplastic condyle, and typically requires surgical intervention for reduction.
Epidemiology
Patellar dislocation accounts for approximately 2 to 3% of knee injuries. This injury tends to affect young and active individuals, with adolescent females and athletes at a higher risk. Incidence is reported as 5.8 per 100,000 but could be as high as 29 per 100,000 in the adolescent population.[2] Acute dislocations tend to occur relatively equally in males and females. Patella dislocations are most common in the second and third decades of life.
Pathophysiology
Patellar dislocations tend to occur in a lateral direction, partly because the direction of pull of the quadriceps muscle is slightly lateral to the mechanical axis of the limb. Medial instability is rare and more likely to result from congenital conditions, quadriceps atrophy, or iatrogenically. Intra-articular dislocation is also uncommon, but can occur following trauma where the patella is avulsed from the quadriceps tendon and is then rotated. Superior dislocations can occur in elderly patients where forced hyperextension causes the patella to lock on an anterior femoral osteophyte.
Individuals with an increased Q angle are predisposed to dislocation. The Q angle is measured by drawing a line from the anterior superior iliac spine (ASIS) through the center of the patella, and a second line from the center of the patella to the tibial tubercle. Normal Q angle measurement is typically higher in females than in males, 18 degrees compared to 14 degrees. Measurements that exceed those normals predispose the patient to patellar instability.
There are several static and dynamic stabilizers of the patella. The medial patellofemoral ligament (MPFL) is the primary static restraint to lateral patellar instability during the first 20 degrees of knee flexion. This ligament is almost always torn with patellar dislocations. The bony structure of the patellofemoral joint is another static stabilizer, especially during deeper knee flexion angles. Anatomical factors that predispose to dislocation include patella alta (high riding patella), trochlear dysplasia or lateral femoral condyle hypoplasia, and excessive lateral patella tilt. Distortion of the normal patellorfemoral joint anatomy places the patella at higher risk for instability and dislocation. The main dynamic stabilizer of the patella is the vastus medialis obliquus (VMO) muscle. This is the most distal portion of the quadriceps muscle, and exerts a medially directed pull which helps maintain the patella well positioned. Weakness or dysplasia of this muscle increases the risk for dislocations.
History and Physical
Patients typically describe pain and deformity of the knee following a non-contact twisting injury, or a direct blow to the anterior or medial aspect of the knee. They often describe the knee giving way and feeling a ‘pop’, and commonly report swelling in the acute setting. In chronic cases, pain is usually anterior or anteromedial, and patients may report giving way, clicking and catching, with the symptoms being worse during flexion and kneeling.
On examination of an acute dislocation, joint effusion or hemarthrosis is a typical finding, but is less likely in the case of chronic dislocation. Alignment abnormalities can also be noted such as femoral anteversion, patella alta, tibial torsion, genu recurvatum, genu valgum or varum, pes planus, and general ligamentous laxity. The knee and surrounding structures can also be palpated, checking for tenderness or irregularities along all the poles of the patella (superior, inferior, medial and lateral), especially the medial pole. If pain permits, flexion and extension should be checked, feeling for any crepitus or restriction of movement. Assessment of the collateral and cruciate ligaments is also necessary.
Some patients can exhibit a positive J sign; excessive lateral patellar deviation going from flexion to extension. In a normal knee, the patella can be moved medially and laterally between twenty-five and fifty percent the width of the patella. In recurrent dislocators, it may move further (patellar glide). They may have a positive apprehension test; the knee is held relaxed in 20 to 30 degrees of flexion, and the patella is pushed laterally. A positive test is present when there is apprehension or guarding.
Evaluation
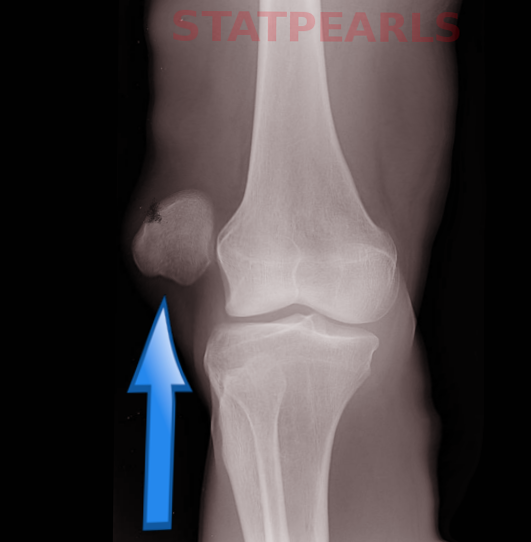
Plain Radiographs
It is necessary to get anteroposterior (AP) and lateral radiographs of the affected knee, as well as patellar (sunrise) views.[3] These will help identify fractures, the presence of loose bodies, malalignment or arthritic changes. Fractures or loose bodies usually originate from the medial aspect of the patella, and can sometimes involve the lateral femoral condyle. Anatomic risk factors for dislocation can also be noted on the radiographs such as patella alta; there may be disruption of the Blumensaat line whereby the lower pole of the patella should lie on a line drawn anteriorly from the intercondylar notch with the knee flexed to 30 degrees. The Insall-Salvati ratio is classically measured to determine patellar height, and is measured on the lateral view with the knee flexed to 30 degrees; it is the ratio measuring the length of the patellar tendon (LL; from the inferior patellar pole to the tibial tubercle) and the patellar length (LP; the longest diagonal length of the patella). A normal ratio is 1.0; a ratio greater than 1.2 suggests patella alta, while less than 0.8 suggests patella baja.
The lateral view can also allow assessment of trochlear dysplasia. The 'crossing sign' is present when the trochlear groove is in the same plane as the anterior border of the lateral condyle, suggestive of flattening. The 'double contour sign' is present if the patient has a convex trochlear groove or underdeveloped medial condyle. It occurs when the anterior border of the lateral condyle is in front of the anterior border of the medial condyle. The Merchant (sunrise) view is for assessment of patellar tilt; it is an axial view at 45 degrees of flexion. The sulcus and congruence angles can be measured on this view.
Computer Tomography Scans (CT)
CT scan allows measurement of the TT-TG distance which is an important parameter in evaluation and management of patellar dislocation. A line is drawn tangent to the posterior border of both femoral condyles. Then 2 lines are drawn perpendicular to this line. One line is from the apex of the tibial tubercle (A), and one line is from the deepest point of the trochlear groove (B). The distance between lines A and B is the TT-TG distance, and is normally less than 20mm. A measurement above 20mm is considered abnormal. The CT scan can also delineate the presence and extent of osteochondral fractures and can help plan any surgical intervention.
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging is very helpful in looking at the soft tissue structures of the knee. In cases of complete dislocation, there is typically a characteristic bruising pattern of the lateral femoral condyle and medial patella. There may be disruption of the MPFL (usually at the medial femoral epicondyle insertion).[4] This imaging modality is very helpful in diagnosing articular cartilage damage on the medial patellar facet, and is more sensitive in detecting osteochondral lesions. It can also aid in looking at the trochlear anatomy in cases of trochlear dysplasia. The Dejour's classification of trochlear dysplasia has 4 grades; type A is flatter than normal with a sulcus angle greater than 145 degrees, type B which is flat, type C which is convex, and type D which is convex with a supratrochlear spur.
Treatment / Management
Acute Dislocations
Acute management of an acute patella dislocation is prompt reduction of the dislocation. This procedure is usually performed in the emergency department with some sedation as needed. The reduction process involves flexing the hip, applying gentle pressure to the lateral pole of the patella, in a medial direction, while slowly extending the knee. It is also possible to perform the reduction maneuver with the patient sitting up with legs hanging off the side of the trolley.
The mainstay of treatment for first-time dislocators without evidence of loose bodies or intra-articular damage is conservative, including analgesia, icing and NSAIDs to reduce pain and swelling, physiotherapy and activity modification. Bracing in a J brace or a patella stabilizing sleeve may be beneficial short term (2 to 4 weeks) to allow the soft tissues to heal. Subsequent, physiotherapy should be started with an emphasis on quadriceps and vastus medialis oblique strengthening, core strengthening and proprioception. The patient can be allowed to weight bear as tolerated.
There remains debate on the role of surgical management of acute first time dislocations. A recent Cochrane review revealed that, although there was some evidence in support of surgical management, the quality of the evidence was insufficient to support a change in current practice.[5] Some surgeons advocate performing arthroscopy in the presence of an osteochondral fracture, with open repair of the fragment if feasible.[6](A1)
Surgical Management
Surgical management can be a consideration in several situations[6]:(B3)
- A first time dislocation with osteochondral fracture/loose body
- MRI demonstrating disruption of MPFL
- Subluxed patella on Merchant radiograph view with a normal contralateral knee
- Failure to improve with conservative management with anatomical factors which predispose to dislocation
- Recurrent dislocations
There is evidence which suggests that early stabilization procedures can reduce the rate of subsequent dislocations but in the absence of clear subjective benefits at long term follow up.[7](A1)
Surgical management is usually via proximal and distal realignment. There are numerous surgical options available:
Arthroscopy with or without open debridement
Arthroscopic or open debridement with removal of any loose bodies may be necessary for displaced osteochondral fractures or loose bodies. Osteochondral fragment repair is favored if sufficient bone is available for fixation.
MPFL repair (re-attachment) or reconstruction (proximal realignment)
Proximal realignment constitutes repairing or reconstructing the MPFL. In brief, to repair the ligament, a longitudinal incision is made at the border of the VMO, just anterior to the medial epicondyle. The ligament is usually re-attached to the femur using bone anchors. If the patient has had recurrent dislocations, then reconstruction of the MPFL is necessary using gracilis or semitendinosus autografts, or allografts.
Isolated repair/reconstruction of the MPFL is not a recommendation in patients with bony abnormalities including TT-TG distance greater than 20mm, convex trochlear dysplasia, severe patella alta, advanced cartilage degeneration or severe femoral anteversion.[1]
Lateral release (distal realignment)
A lateral release cuts the retinaculum on the lateral aspect of the knee joint. The aim is to improve the alignment of the patella by reducing the lateral pull. It is not performed in isolation, but usually in combination with other more powerful realignment procedures.
Osteotomy (distal realignment)
An osteotomy is necessary when there is abnormal anatomy contributing to poor patella tracking and a high TT-TG distance. The most common procedure of this type is known as the Fulkerson osteotomy. This osteotomy involves cutting the anterior tibia at a certain angle to allow for anterior and medial displacement of the osteotomized fragment, moving the patellar tendon insertion on the tibia (along with the patella) more medially and anteriorly. This will reduce the Q angle and will decrease the risk of recurrence. If the patient has patella alta, an osteotomy allows the surgeon to effectively lower the patella by distal displacement of the osteotomized fragment.
In the presence of a rotational deformity, a derotational osteotomy of the femur may be considered. Those procedures are not appropriate in patients with open growth plates.
Trochleoplasty
Trochleoplasty is indicated in recurrent dislocators with a convex or flat trochlea. The trochlear groove is deepened to create a deeper groove for the patella to glide through; this may take place in conjunction with an MPFL reconstruction. Studies have suggest that trochleoplasty is not advisable in patients with open growth plates or severely degenerative joint. This procedure is uncommon but may be considered in severe cases.
Differential Diagnosis
- Anterior cruciate ligament injury
- Medial collateral ligament injury
- Meniscal injury
- Patellofemoral syndrome
- Medial synovial plica
- Chondromalacia
Prognosis
Physiotherapy can be necessary for as long as two to three months following an initial dislocation. Physiotherapy is vital, as if the medial retinaculum does not heal and the VMO does not adequately rehabilitate, recurrent dislocation will ensue. Studies suggest there is a 20 to 40% risk of re-dislocation, with even higher rates following a second dislocation.[8]
It is common for patients to remain symptomatic after the first dislocation. Atkin et al. found that at 6 months, 58% of patients experience limitation in strenuous activities.[9] Although the range of motion was regained, participation in sports was reduced in the first 6 months following injury; kneeling and squatting were particularly challenging. Failure to return to sport occurred in 55%. Maenpaa et al. found that over 50% of patients have complications following a first-time dislocation including re-dislocation, subluxation or patellofemoral pain.[10]
Patients with anatomic abnormalities as the main reason for their dislocation may also sustain a dislocation to the contralateral patella requiring treatment. Stability, however, tends to increase with advancing age of the patient.
Complications
Complications of acute patella dislocation include associated osteochondral fracture, the risk of recurrence, and degenerative arthritis.
General surgical complications include infection, neurovascular injury, deep vein thrombosis or pulmonary embolism.
Complications specific to MPFL surgery include saphenous nerve neuritis and rupture.
Following osteotomy, patients often complain of pain over the screw site. There may be a loss of ability to kneel comfortably. There is also a risk of proximal tibial fracture.[11]
Even following surgery, there remains a risk of recurrent lateral patellar instability.
Postoperative and Rehabilitation Care
Postoperative rehabilitation depends on the surgery completed. A lateral release is quickest to recover from, with osteotomies taking considerably longer. Recovery from surgery can last from 6 months to a year, and physiotherapy is vital after a period of immobilization.
Deterrence and Patient Education
Patients should be discouraged from returning too early to contact sports before they have undergone sufficient physiotherapy to aid the strengthening of surrounding muscles and the core. Slip-on knee braces may be of benefit in the early rehabilitative phase. The importance of adherence to a physiotherapy plan after initial dislocation should be a point of emphasis, because good compliance may minimize the risk of further dislocation and the need for operative intervention.
Pearls and Other Issues
- It is essential to establish the etiology of the dislocation, particularly in those that have recurrent dislocations as this can alter the management plan
- Acute dislocations can be managed conservatively with bracing and physiotherapy with a focus on quadriceps, VMO and core strengthening
- Be wary of the patient with a large hemarthrosis and normal radiographs as they may have a sizeable osteochondral fragment that requires early fixation
- Surgery, where needed, is typically tailored to the patient's anatomical profile and their predisposing factors
- Most surgical procedures are not indicated in patients with open physes
- Despite surgery, there remains a small risk of recurrence
Enhancing Healthcare Team Outcomes
Close liaison between emergency medicine doctors, orthopedic teams, radiology, and physiotherapy is vital to managing patellar dislocations safely. This is especially true in the early stages when additional CT/MRI scans may be required to rule out more serious injuries. Once the patient is on the non-operative management path, physiotherapists are crucial in ensuring patients strengthen muscles correctly as this may be all that is needed to manage an acute dislocation. Working within an interprofessional team will enhance patient care and outcomes.
Media
References
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM. Epidemiology and natural history of acute patellar dislocation. The American journal of sports medicine. 2004 Jul-Aug:32(5):1114-21 [PubMed PMID: 15262631]
Jain NP, Khan N, Fithian DC. A treatment algorithm for primary patellar dislocations. Sports health. 2011 Mar:3(2):170-4 [PubMed PMID: 23016004]
Beaconsfield T, Pintore E, Maffulli N, Petri GJ. Radiological measurements in patellofemoral disorders. A review. Clinical orthopaedics and related research. 1994 Nov:(308):18-28 [PubMed PMID: 7955681]
Elias DA,White LM,Fithian DC, Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002 Dec; [PubMed PMID: 12461254]
Level 2 (mid-level) evidenceSmith TO, Donell S, Song F, Hing CB. Surgical versus non-surgical interventions for treating patellar dislocation. The Cochrane database of systematic reviews. 2015 Feb 26:(2):CD008106. doi: 10.1002/14651858.CD008106.pub3. Epub 2015 Feb 26 [PubMed PMID: 25716704]
Level 1 (high-level) evidenceTsai CH, Hsu CJ, Hung CH, Hsu HC. Primary traumatic patellar dislocation. Journal of orthopaedic surgery and research. 2012 Jun 6:7():21. doi: 10.1186/1749-799X-7-21. Epub 2012 Jun 6 [PubMed PMID: 22672660]
Level 3 (low-level) evidenceSillanpää PJ, Mattila VM, Mäenpää H, Kiuru M, Visuri T, Pihlajamäki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. The Journal of bone and joint surgery. American volume. 2009 Feb:91(2):263-73. doi: 10.2106/JBJS.G.01449. Epub [PubMed PMID: 19181969]
Level 1 (high-level) evidenceMäenpää H, Huhtala H, Lehto MU. Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta orthopaedica Scandinavica. 1997 Oct:68(5):424-6 [PubMed PMID: 9385239]
Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. The American journal of sports medicine. 2000 Jul-Aug:28(4):472-9 [PubMed PMID: 10921637]
Mäenpää H, Lehto MU. Patellar dislocation. The long-term results of nonoperative management in 100 patients. The American journal of sports medicine. 1997 Mar-Apr:25(2):213-7 [PubMed PMID: 9079176]
Fulkerson JP. Fracture of the proximal tibia after Fulkerson anteromedial tibial tubercle transfer. A report of four cases. The American journal of sports medicine. 1999 Mar-Apr:27(2):265 [PubMed PMID: 10102112]
Level 3 (low-level) evidence