Anatomy, Head and Neck: Internal Maxillary Arteries
Anatomy, Head and Neck: Internal Maxillary Arteries
Introduction
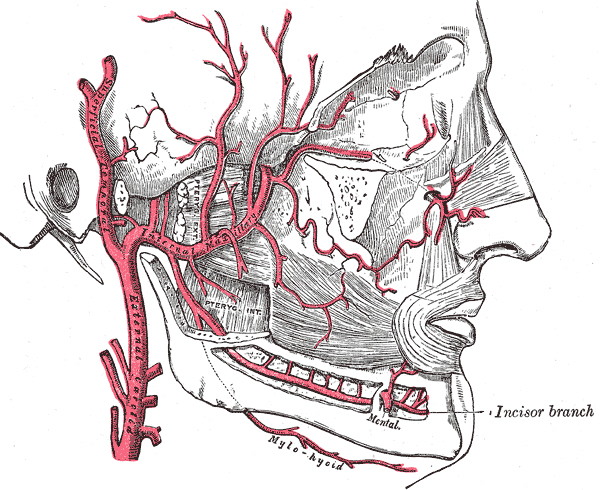
The maxillary artery is a branch of the external carotid artery and supplies many structures on the face. The maxillary artery arises posterior to the mandibular neck, traverses the parotid gland, and passes forward between the sphenomandibular ligament and ramus of the mandible. It then runs a superficial course lateral to the lateral pterygoid muscle. The maxillary artery supplies deep structures of the face including the mandible, pterygoid, infratemporal fossa and segments of the pterygopalatine fossa. In this review, we will go over the anatomy and look at an in-depth view of the branches of the maxillary artery.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The internal maxillary artery, simply known as the maxillary artery, is a terminal branch of the external carotid artery (ECA); which itself is a branch of the bilateral common carotid arteries at the C4 vertebral level where the common carotids bifurcate into the internal and external carotids. The external carotid supplies blood to structures in the superficial face, and superior superficial cranial structures. The branches of the external carotid artery include the superior thyroid artery, ascending pharyngeal artery, lingual artery, facial artery, occipital artery, posterior auricular artery, and the two terminal branches are the maxillary artery and superficial temporalis artery.
The maxillary artery provides many branches which supply structures within the face and cranium. Because of its many branches, the maxillary artery divides into three segments relative to the lateral pterygoid muscle. The mandibular or first division runs down to the mandible and runs along the apices of the teeth. It also ascends to the meninges, which is a protective membrane that encircles the brain and spinal cord. The first division of the maxillary artery is also considered to be posterior the lateral pterygoid muscle. The pterygoid division or second division runs lateral to the lateral pterygoid for the most part and supplies the surrounding structures. The first two divisions are considered to be within the infratemporal fossa.[1] The pterygopalatine or third division consists of all the terminal branches and runs anterior to the lateral pterygoid muscle. The third division is within the pterygopalatine fossa.[2] The maxillary artery originates within the parotid gland and travels anteriorly toward where it is between the neck of the mandible and sphenomandibular ligament at which point the artery is now in the infratemporal fossa and usually lateral to the lateral pterygoid muscle. From here, the artery travels obliquely to the pterygopalatine fossa through the pterygomaxillary fissure.
Mandibular (1 part) of the maxillary artery[3]:
- Deep auricular artery: enters the squamotympanic fissure
- Anterior tympanic artery: enters the squamotympanic fissure
- Middle meningeal artery: courses between the tensor veli palatine muscle and lateral pterygoid muscle to enter the foramen spinosum into the middle cranial cavity
- Contains an anterior branch which travels vertex and crosses the pterion. Contains a posterior branch which travels posterior and superior to reach the middle cranial fossa
- Accessory meningeal artery: enters the foramen ovale
- Inferior alveolar artery: enters the mandibular foramen
- Gives rise to the mylohyoid artery (branch of the inferior alveolar artery before it enters the mandible)
- Mental artery (terminal branch of the inferior alveolar artery)
Pterygoid (2 part) of the maxillary artery:
- Anterior, middle and posterior deep temporal arteries
- Buccal artery
- Masseteric artery
- Pterygoid branches
Pterygopalatine (3 part) of the maxillary artery[4]:
- Pharyngeal artery: enters the palatovaginal canal
- Greater palatine artery: enters the greater palatine foramen
- Gives rise to the lesser palatine branch
- Artery of the pterygoid canal
- Sphenopalatine artery: enters the sphenopalatine foramen
- Gives rise to the posterior lateral nasal arteries
- Gives rise to the posterior septal branches
- Posterior superior alveolar artery
- Infraorbital artery: enters inferior orbital fissure
- Gives rise to the anterior superior alveolar artery
Embryology
Part of the maxillary artery arises from the remnant of the first aortic arch. In general the first and second part of the aortic arch regress and do not remain to form into any permanent anatomical structures.
Blood Supply and Lymphatics
The first division of the maxillary artery:
- Deep auricular and anterior tympanic artery supplies the external acoustic meatus and deep surface of the tympanic membrane, respectively.
- The middle meningeal artery is a major branch of the internal maxillary artery and has very significant clinical scenarios discussed later. This artery mainly supplies the dura, bone, and cranial cavity of the middle cranial fossa. It is attached to the periosteal or outer layer of the dura.[5] The accessory meningeal artery also supplies similar structures. The ascending pharyngeal and occipital artery (branches of the external carotid) also give rise to posterior meningeal arteries supplying the dura within the posterior cranial fossa. The posterior meningeal artery coming from the ascending pharyngeal artery travels through the hypoglossal canal to reach the posterior cranial fossa.
- The inferior alveolar artery supplies all the lower teeth, lower lip, and chin (through the mental artery). The mylohyoid artery supplies the mylohyoid.[1]
The second division of the maxillary artery:
- The anterior, middle, and posterior deep temporalis artery supply blood to the temporalis muscle. The temporalis muscle also obtains some blood supply from the superficial temporalis artery (branch of the ECA).
- Buccal artery supplies the buccinators muscle, and the masseteric artery supplies the masseter muscle.
- The pterygoid branches are small branches from the maxillary artery, which supply both the lateral pterygoid and medial pterygoid muscle.
The third division of the maxillary artery:
- The pharyngeal artery supplies the posterior aspect of the roof of the nasal cavity, sphenoid sinus, and Eustachian tube.
- The greater palatine artery provides blood to the hard palate, and the lesser palatine artery gives supply to the soft palate.
- The sphenopalatine artery terminates into the posterior lateral nasal artery and posterior septal branches. The posterior lateral nasal artery supplies the lateral wall of the nasal cavity, and the posterior septal branches supply the nasal septum of which some branches anastomose with the greater palatine artery.
- The posterior superior alveolar artery supplies the lower mandible, molar, premolars, and surrounding gingiva.
- The infraorbital artery supplies the lower eyelid and upper lip. The anterior superior alveolar artery supplies the incisors and canines.[2]
Venous drainage:
The venous drainage for most of the structures supplied the maxillary artery is through the pterygoid plexus, which is between the medial and lateral pterygoid as well as between the lateral pterygoid and temporalis muscle. This venous plexus drains much of the blood from structures of the infratemporal fossa and pterygopalatine fossa. Other veins which also drain into the pterygoid plexus include the inferior ophthalmic vein and emissary veins from the cavernous sinus. These emissary veins travel through the foramen ovale, through the foramen lacerum and sphenoidal foramen to reach the pterygoid plexus.[1][4][2]
Muscles
There are many muscles within the infratemporal fossa and pterygopalatine fossa as well as many muscles which the multiple branches of the maxillary artery supply. For this review, the focus will be placed primarily on the lateral and medial pterygoid muscles because of their importance to the division of the maxillary artery.
Lateral pterygoid muscle:
The lateral pterygoid muscle contains two heads, an upper and lower head. The upper head, which is the smaller of the two parts originates from the roof of the infratemporal fossa, and the lower head originates from the lateral surface of the lateral plate of the pterygoid process. Both heads insert into the capsule of the temporomandibular joint. The fibers of the muscle run almost horizontally; thus, the action of the lateral pterygoid lies primarily with jaw protrusion as well as some side to side movement of the jaw.[6]
Medial pterygoid muscle:
The medial pterygoid also has two heads but are named deep and superficial heads. The deep head has its origin from the medial surface of the lateral plate of the pterygoid process, and the superficial head originates from the tuberosity of the maxilla. The two heads insert into the medial surface near the angle of the mandible. The function of the muscle lies mainly with the elevation of the jaw and some side to side movement.[6][1]
Physiologic Variants
There are many physiologic variants within the maxillary artery and its course along with lateral pterygoid muscle, relative to whether it travels lateral to the lateral pterygoid or medial to the lateral pterygoid. Some studies have shown that there is a 66% chance it travels laterally and 33% that it travels medially. Other variants include a deep auricular and anterior tympanic artery branching from a common trunk versus individually coming off the maxillary artery. Another variation consists of the middle meningeal artery and accessory meningeal artery coming from a common trunk versus independently branching off the maxillary artery. Interestingly enough one study has found that cadavers with a medially coursing maxillary artery generally have the middle meningeal and accessory meningeal coming off the maxillary as separate arteries while a laterally coursing maxillary artery has shown the middle and accessory meningeal arteries coming off as a common trunk. Another interesting finding was while the majority of people have mirror tracks of the maxillary artery, a minimal number of patients could have one side of the maxillary artery traveling laterally to the muscle and medially on the contralateral side.[4]
Surgical Considerations
Posterior epistaxis is more challenging to control, and generally, treatment with anterior packing (which can control anterior epistaxis) is inadequate. Often posterior epistaxis can stop spontaneously, however for patients whose bleeding cannot be controlled with balloon tamponade or for recurrent symptoms surgical endovascular embolization of the sphenopalatine artery and anterior ethmoid artery can lead to resolution of the problem.[4][7]
In recent years extracranial to intracranial bypass using the maxillary artery has gained traction mainly for the treatment of skull base tumors and complex cerebral aneurysms. This procedure requires a zygomatic osteotomy to allow proper exposure of the vessel. However, recent studies are showing a new and novel technique to reach the maxillary artery without the need for zygomatic osteotomy; this involves reaching the artery through the deep temporal vessels upon reflection of the temporalis muscle.[8][9][10]
Clinical Significance
A very significant clinical significance regarding the pterygoid plexus is the spreading of infection to the intracranial area. As previously noted, the pterygoid plexus is in connection with the cavernous sinus through small emissary veins which do not contain venous valves, which can allow infections within the dental area (which are drained by the pterygoid plexus) to travel to the cavernous sinus and cause intracranial infections from an extracranial source.[1]
Epidural hematomas form from trauma to the middle meningeal artery at the pterion. The artery is within the periosteal dura and thus leaking of the vessel is under high pressure and causes a hematoma formation between the layers of the dura. More often epidural hematomas occur in younger patients aged 20 to 30 years old and less often in 50 to 60-year-old patients because older patients have dura that more tightly adheres to the cranium and it is less likely for a hematoma to form between the layers of the dura. The patient initially experiences a brief loss of consciousness following a characteristic and almost pathognomonic “lucid interval,” where the patient can function. However, as the expanding hematoma continues to increase intracranial pressure, the patient then loses consciousness again with a high risk of mortality and morbidity. The most common modality used for evaluation of epidural hematoma is a non-contrast CT scan because it is more likely to show an acute bleed. The characteristic lens-shaped lesion, which does not cross suture lines, is how an epidural often presents. Epidural hematomas are considered neurosurgical emergencies and require immediate evacuation and relief of pressure off the brain. The gold standard is craniotomy; however, burr hole placement is also acceptable if the patient is not in a setting equipped to do a craniotomy.[11]
Media
(Click Image to Enlarge)
References
Casale J, Bordoni B. Anatomy, Head and Neck: Infratemporal Fossa. StatPearls. 2023 Jan:(): [PubMed PMID: 30725719]
Cappello ZJ, Potts KL. Anatomy, Pterygopalatine Fossa. StatPearls. 2023 Jan:(): [PubMed PMID: 30020641]
White HJ, Reddy V, Mesfin FB. Anatomy, Head and Neck: Foramen Spinosum. StatPearls. 2023 Jan:(): [PubMed PMID: 30571053]
Alvernia JE, Hidalgo J, Sindou MP, Washington C, Luzardo G, Perkins E, Nader R, Mertens P. The maxillary artery and its variants: an anatomical study with neurosurgical applications. Acta neurochirurgica. 2017 Apr:159(4):655-664. doi: 10.1007/s00701-017-3092-5. Epub 2017 Feb 13 [PubMed PMID: 28191601]
Natali AL, Reddy V, Leo JT. Neuroanatomy, Middle Meningeal Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 30137830]
Corcoran NM, Goldman EM. Anatomy, Head and Neck, Masseter Muscle. StatPearls. 2023 Jan:(): [PubMed PMID: 30969691]
Iimura J, Hatano A, Ando Y, Arai C, Arai S, Shigeta Y, Kojima H, Otori N, Wada K. Study of hemostasis procedures for posterior epistaxis. Auris, nasus, larynx. 2016 Jun:43(3):298-303. doi: 10.1016/j.anl.2015.09.015. Epub 2015 Oct 31 [PubMed PMID: 26527519]
Wang L, Cai L, Lu S, Qian H, Lawton MT, Shi X. The History and Evolution of Internal Maxillary Artery Bypass. World neurosurgery. 2018 May:113():320-332. doi: 10.1016/j.wneu.2018.02.158. Epub 2018 Mar 7 [PubMed PMID: 29524709]
Level 2 (mid-level) evidenceAkiyama O, Güngör A, Middlebrooks EH, Kondo A, Arai H. Microsurgical anatomy of the maxillary artery for extracranial-intracranial bypass in the pterygopalatine segment of the maxillary artery. Clinical anatomy (New York, N.Y.). 2018 Jul:31(5):724-733. doi: 10.1002/ca.22926. Epub 2017 Nov 29 [PubMed PMID: 28556192]
Yağmurlu K, Kalani MYS, Martirosyan NL, Safavi-Abbasi S, Belykh E, Laarakker AS, Nakaji P, Zabramski JM, Preul MC, Spetzler RF. Maxillary Artery to Middle Cerebral Artery Bypass: A Novel Technique for Exposure of the Maxillary Artery. World neurosurgery. 2017 Apr:100():540-550. doi: 10.1016/j.wneu.2016.12.130. Epub 2017 Jan 9 [PubMed PMID: 28089839]
Khairat A, Waseem M. Epidural Hematoma. StatPearls. 2023 Jan:(): [PubMed PMID: 30085524]