Introduction
Schizencephaly is a rare congenital neuronal migration disorder characterized by the presence of a full-thickness cleft, lined with heterotopic gray matter and filled with cerebrospinal fluid (CSF), which connects the pial surface of the cerebral hemisphere with the ependymal surface of the lateral ventricle.[1][2]
Schizencephaly was first described by Wilmarth in 1887.[2] The term was coined from the Greek word "schizen" 'to divide' and introduced by Yakovlev and Wadsworth in 1946, based on their work on cadavers, that classified schizencephaly into two types.[3] These are:
- Type I (closed-lip): Cleft is fused, preventing CSF passage.
- Type II (open-lip): A cleft is present, which permits CSF to pass between the ventricular cavity and subarachnoid space.
Schizencephaly can be either unilateral or bilateral and has a prevalence of 1.48 per 100,000 live births.[2][4]
Recent literature classifies schizencephaly into three types, as the full-thickness cleft containing CSF is not mandatory for the definition.[5]
- Type 1 (trans-mantle): No CSF-containing cleft on magnetic resonance imaging (MRI), but contains a trans-mantle column of abnormal gray matter.
- Type 2 (closed-lip): Presence of cleft containing CSF, but the lining lips of abnormal gray matter are abutting and opposed to each other.
- Type 3 (open-lip): Presence of cleft containing CSF. The lining lips of abnormal gray matter are not abutting each other.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The exact etiopathogenesis of schizencephaly is not yet clearly understood in the scientific world.
Possible etiological factors include:
- Exposure to teratogenic agents or viral infections prenatally
- Genetic factors
- Stroke in utero
- Young maternal age[6]
Some environmental exposures have been implicated:
- Teratogens such as alcohol, warfarin, or cocaine
- Viral infection, especially cytomegalovirus (CMV), and recently Zika virus
- Attempted abortion
- Hypoxia in the eighth week of gestation
- Amniocentesis, or chorionic villus biopsy
- Maternal trauma[7]
Fetal intracranial hemorrhage caused by abnormal type IV collagen has also been implicated.[8]
Some genetic mutations have been reported as possible etiological factors for schizencephaly. The main genes identified in this regard are the following:
Epidemiology
Schizencephaly is a rare cerebral malformation with an estimated incidence of 0.54 to 1.54 per 100,000 live births.[2] The estimated prevalence is 1.48/100 000 births.[4] It is almost always sporadic. Only a few familial cases have been described, and there is no known gender predilection.[11] Schizencephaly can be more commonly seen in abandoned or adopted children, and that supports the possibility of exposure to in-utero insults.[7] It was also reported to occur more frequently in the fetuses of younger mothers.[4]
Pathophysiology
Schizencephaly results from abnormal neuronal migration a few weeks after gestation.
There are a few hypotheses that try to explain the pathogenesis of schizencephaly.[12] These include the following:
- In-utero exposure to CMV results in an inflammatory process that leads to a middle cerebral artery (MCA) stroke. This is supported by the fact that the majority of schizencephaly lesions occur in the MCA territory.
- Environmental factors like maternal age (below 20 years), no first-trimester antenatal medical care, and drug or alcohol abuse can contribute to the maldevelopment of the brain in schizencephaly.
- Genetic factors can also contribute to the development of schizencephaly and other associated anomalies like polymicrogyria, septum pellucidum and/or corpus callosum agenesis, optic nerve atrophy, arachnoid cysts, and cerebellar anomalies. EMX2 gene regulates the structural development of the prosencephalon. Patients with a heterozygotic mutation of this are prone to develop this condition, even though such a cause is rare.
Schizencephaly has also been described as a part of genetic syndromes like Vici syndrome (corpus callosum agenesis, albinism, immune deficiency, cardiomyopathy), which occurs due to EPG5 gene mutation.
Histopathology
Since schizencephaly results from abnormal migration due to destructive changes, they are lined by abnormal gray matter.[3][13][14] The frontal lobe is the lobe most commonly involved, followed by the central sulcus in this condition.[15]
History and Physical
The clinical presentation of schizencephaly is a wide range. The patients might have normal cognition with seizure onset in adulthood. Motor deficits are more common than any other types of neurological deficits, and the patients can have hemiparesis with mild developmental delay or severe cognitive impairment with quadriparesis.[7]
Clinical presentation depends on the type.
- Type I (closed-lip) has a milder course which can be asymptomatic or diagnosed only in adult patients and presents with epileptic seizures and mild motor deficits.[12]
- Type II (open lip) has a severe course, manifested by epilepsy (often refractory), intellectual disability, varying degrees of paralysis, hemiparesis in unilateral schizencephaly, and quadriparesis in bilateral schizencephaly.[12]
The clinical features of patients with schizencephaly can be classified according to whether the finding is unilateral or bilateral.[2][16] Unilateral schizencephaly may present with contralateral hemiparesis and asymmetrical muscle tone. Bilateral schizencephaly may present with seizures, developmental delay, quadriparesis, and severe mental deficits.
Rarely, schizencephaly can present in adulthood with psychiatric manifestations such as paranoia, irritability, and impulsive spending.[17]
Evaluation
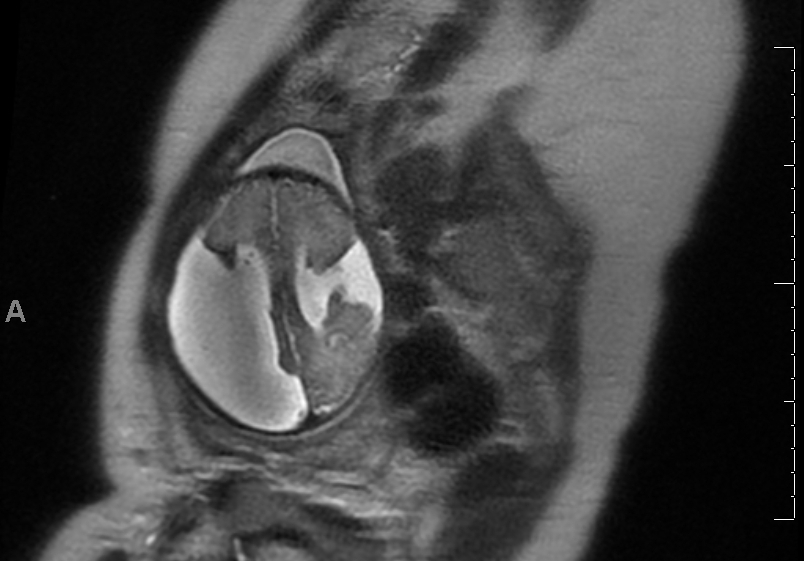
The diagnostic method of choice for imaging schizencephaly is magnetic resonance imaging (MRI). Imaging shows a fluid-filled linear cleft lined with heterotrophic gray matter that extends from the pial membrane of the cortex to the ependymal surface in the ventricle.[12][18] Type 1 can be seen as a nipple-like out-pouching at the ventricular surface.[5] It has been recently identified based on transcranial magnetic stimulation (TMS) and diffusion tensor imaging (DTI) that the cross-sectional area symmetricity of the pyramidal tract in pons is associated with the dexterity of the hand function in patients with schizencephaly.[19]
Computed tomography (CT) may also be useful, but it provides poorer images of the gray matter, which are the key factor in differentiating between schizencephaly and other fluid-associated central nervous system (CNS) abnormalities such as arachnoid cyst, porencephaly, and hydranencephaly. The diagnosis may be suspected prenatally if clefts are viewed within the cerebral hemispheres by two-dimensional ultrasonography (2DUS).[20]
The epileptogenic zone on EEG may demonstrate the area of the dysplastic cortex, which may be situated not only within the cleft but also in its vicinity or in the contralateral hemisphere.[12] In the latter case, which is located in the contralateral hemisphere in the same or similar location, it is called a mirror focus.
Associated anomalies include septo-optic dysplasia (SOD), optic nerve hypoplasia, absence of septum pellucidum, pachygyria, polymicrogyria, heterotopia, and arachnoid cysts.[21]
Treatment / Management
The treatment for schizencephaly depends on multiple factors, including the signs and symptoms and severity of the condition.
Treatment generally consists of drugs to prevent seizures and/or physical therapy. In cases complicated by hydrocephalus, a surgically implanted shunt can divert fluid to another area of the body from which it can be absorbed.[22]
Management is mainly supportive, which includes rehabilitation for motor deficits, intellectual disability, and seizure management. Surgery can be a choice in cases with hydrocephalus or raised intracranial pressure.[12](B3)
Differential Diagnosis
The primary differential diagnosis is an arachnoid cyst. This is mainly differentiated in imaging studies from schizencephaly by the following features in the table below.[12]
| Feature | Schizencephaly | Arachnoid cyst |
| Heterotropic gray matter that lines the margins of the cleft | Absent | Present |
| Mass effect in the form of displacement of the longitudinal fissure, ventricular compression, or local obliteration of brain sulci and fissures | Absent | May be present |
| Thinning and bulging of adjacent cranial bone | Absent | May be present |
Other differentials include:
- Acquired cysts (post-traumatic, postoperative, post-hemorrhage, or postictal): These can be differentiated by areas of gliosis surrounding the lesions and based on medical history.
- Hydrocephalus
- Holoprosencephaly
- Focal cortical dysplasia may have a cleft on the cortex, not extending up to the ventricles.
- Grey matter heterotopia will be seen as a linear cleft, but periventricular grey matter generally bulges into the ventricle.
- Porencephaly extends from the cortex to ventricles but is lined by gliotic white matter; some authors would refer to schizencephaly as 'true porencephaly.'[8][23]
Prognosis
The prognosis depends on the size and type of the clefts.
- Type I (closed-lip) has a milder course. It can be asymptomatic or diagnosed only in adult patients and presents with epileptic seizures and mild motor deficits.[12]
- Type II (open lip) has a more severe presentation, manifested by epilepsy (often refractory), intellectual disability, varying degrees of paralysis, hemiparesis in unilateral schizencephaly, and quadriparesis in bilateral schizencephaly.[12]
Type II clefts are associated with poor seizure outcomes, and a larger cleft is associated with the development of epilepsy in an early stage of life compared to a smaller one. Hence, the type and size of schizencephaly should be considered in treating epilepsy.[24] Patients should be closely followed up with electroencephalography.[25]
Complications
Schizencephaly is a CNS malformation that most often presents as epilepsy. Though a majority of patients have well-controlled seizures, some patients may develop refractory epilepsy with uncontrolled breakthrough seizures and associated risks, including sudden unexpected death in epilepsy (SUDEP).[26][27] Seizures can present for the first time in adulthood.[28]
Individuals with schizencephaly with large fluid-filled spaces may develop elevated intracranial pressure with associated complications such as herniation, and these patients may require surgical intervention with or without ventriculoperitoneal shunt placement. These surgical methods can be associated with complications such as bleeding, subdural hygroma, empyema, hydrocephalus, and infections like meningitis. If shunting is performed, additional possible complications include endocarditis and shunt-related renal damage.[12]
Deterrence and Patient Education
The parents of patients with schizencephaly should be educated regarding the possible complications and the signs for which they should be vigilant. They should be aware of what to do if the kid develops seizures and how to identify any features of intracranial hypertension so that appropriate care can be given to the patient.
Pearls and Other Issues
Schizencephaly is a rare congenital neuronal migration disorder.
- Type I (closed-lip) can be asymptomatic or diagnosed in adult patients.
- Type II (open lip) is a severe malformation that can manifest by refractory epilepsy, intellectual disability, and varying degrees of paralysis from hemiparesis to quadriparesis.
- Possible etiological factors include teratogenic exposures, viral exposures, genetic mutations, and intrauterine fetal stroke.
Risk factors of schizencephaly include young maternal age and the illicit use of alcohol and narcotic substances.
The diagnostic method of choice for imaging schizencephaly is magnetic resonance imaging (MRI).
The therapeutic management of both types of schizencephaly is conservative.
Surgical treatment is undertaken in some cases with concomitant hydrocephalus or intracranial hypertension.
Enhancing Healthcare Team Outcomes
The care of patients with schizencephaly should be with an interprofessional team approach. When a primary clinician evaluates a patient with developmental delay, referral to a pediatric neurologist is recommended. The interprofessional team may include a pediatrician, pediatric neurologist, pediatric neurosurgeon, nurse, and pharmacist. Each team member should contribute from their specialty and openly communicate with other team members if they note any concerns. In fact, open communication is crucial to the success of the interprofessional model; this also includes meticulous record-keeping for each interaction or intervention on the patient so all members of the care team can access the same updated information. Clinicians will guide the overall directions of care, employing various specialties as necessary. Nurses can counsel patients and/or parents and will assist in cases that require surgical intervention with patient preparation and during the procedure, as well as providing post-procedure care and monitoring. Pharmacists will verify dosing and counsel patients or parents on the medication that may accompany the management of this condition [Level 5]
Type 1 (closed-lip) schizencephaly symptoms may not manifest until adulthood.[12] Therefore, it is recommended that an adult neurologist should gain familiarity with the pathophysiology, presentation, diagnosis, and management of schizencephaly.
Media
(Click Image to Enlarge)
References
Tanwir A, Bukhari S, Shamim MS. Frontoethmoidal encephalocele presenting in concert with schizencephaly. Surgical neurology international. 2018:9():246. doi: 10.4103/sni.sni_242_18. Epub 2018 Dec 4 [PubMed PMID: 30603230]
Hung PC, Wang HS, Chou ML, Lin KL, Hsieh MY, Chou IJ, Wong AM. Schizencephaly in children: A single medical center retrospective study. Pediatrics and neonatology. 2018 Dec:59(6):573-580. doi: 10.1016/j.pedneo.2018.01.009. Epub 2018 Jan 6 [PubMed PMID: 29371079]
Level 2 (mid-level) evidenceYAKOVLEV PI, WADSWORTH RC. Schizencephalies; a study of the congenital clefts in the cerebral mantle; clefts with fused lips. Journal of neuropathology and experimental neurology. 1946 Apr:5():116-30 [PubMed PMID: 21026933]
Howe DT, Rankin J, Draper ES. Schizencephaly prevalence, prenatal diagnosis and clues to etiology: a register-based study. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2012 Jan:39(1):75-82. doi: 10.1002/uog.9069. Epub 2011 Dec 5 [PubMed PMID: 21647999]
Griffiths PD. Schizencephaly revisited. Neuroradiology. 2018 Sep:60(9):945-960. doi: 10.1007/s00234-018-2056-7. Epub 2018 Jul 19 [PubMed PMID: 30027296]
Gonzalez JC, Singhapakdi K, Martino AM, Rimawi BH, Bhat R. Unilateral Open-lip Schizencephaly with Tonsillar Herniation in a Preterm Infant. Journal of pediatric neurosciences. 2019 Oct-Dec:14(4):225-227. doi: 10.4103/jpn.JPN_75_19. Epub 2019 Dec 3 [PubMed PMID: 31908665]
Dies KA, Bodell A, Hisama FM, Guo CY, Barry B, Chang BS, Barkovich AJ, Walsh CA. Schizencephaly: association with young maternal age, alcohol use, and lack of prenatal care. Journal of child neurology. 2013 Feb:28(2):198-203. doi: 10.1177/0883073812467850. Epub 2012 Dec 23 [PubMed PMID: 23266945]
Level 2 (mid-level) evidenceHarada T, Uegaki T, Arata K, Tsunetou T, Taniguchi F, Harada T. Schizencephaly and Porencephaly Due to Fetal Intracranial Hemorrhage: A Report of Two Cases. Yonago acta medica. 2017 Dec:60(4):241-245. doi: 10.24563/yam.2017.12.005. Epub 2018 Feb 5 [PubMed PMID: 29434494]
Level 3 (low-level) evidenceBrunelli S, Faiella A, Capra V, Nigro V, Simeone A, Cama A, Boncinelli E. Germline mutations in the homeobox gene EMX2 in patients with severe schizencephaly. Nature genetics. 1996 Jan:12(1):94-6 [PubMed PMID: 8528262]
Hehr U, Pineda-Alvarez DE, Uyanik G, Hu P, Zhou N, Hehr A, Schell-Apacik C, Altus C, Daumer-Haas C, Meiner A, Steuernagel P, Roessler E, Winkler J, Muenke M. Heterozygous mutations in SIX3 and SHH are associated with schizencephaly and further expand the clinical spectrum of holoprosencephaly. Human genetics. 2010 Mar:127(5):555-61. doi: 10.1007/s00439-010-0797-4. Epub 2010 Feb 16 [PubMed PMID: 20157829]
Rege SV, Patil H. Bilateral giant open-lip schizencephaly: A rare case report. Journal of pediatric neurosciences. 2016 Apr-Jun:11(2):128-30. doi: 10.4103/1817-1745.187638. Epub [PubMed PMID: 27606022]
Level 3 (low-level) evidenceHalabuda A, Klasa L, Kwiatkowski S, Wyrobek L, Milczarek O, Gergont A. Schizencephaly-diagnostics and clinical dilemmas. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2015 Apr:31(4):551-6. doi: 10.1007/s00381-015-2638-1. Epub 2015 Feb 18 [PubMed PMID: 25690450]
Level 3 (low-level) evidenceYAKOVLEV PI, WADSWORTH RC. Schizencephalies; a study of the congenital clefts in the cerebral mantle; clefts with hydrocephalus and lips separated. Journal of neuropathology and experimental neurology. 1946 Jul:5(3):169-206 [PubMed PMID: 20993391]
Eller KM, Kuller JA. Fetal porencephaly: a review of etiology, diagnosis, and prognosis. Obstetrical & gynecological survey. 1995 Sep:50(9):684-7 [PubMed PMID: 7478420]
Level 2 (mid-level) evidenceRaybaud C, Girard N, Lévrier O, Peretti-Viton P, Manera L, Farnarier P. Schizencephaly: correlation between the lobar topography of the cleft(s) and absence of the septum pellucidum. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2001 Apr:17(4-5):217-22 [PubMed PMID: 11398940]
Denis D, Chateil JF, Brun M, Brissaud O, Lacombe D, Fontan D, Flurin V, Pedespan J. Schizencephaly: clinical and imaging features in 30 infantile cases. Brain & development. 2000 Dec:22(8):475-83 [PubMed PMID: 11111060]
Level 3 (low-level) evidencePatwal R, Pai NM, Ganjekar S, Arshad F, Alladi S, Sharma MK, Desai G, Chaturvedi SK. Schizencephaly and the Neurodevelopmental Model of Psychosis. Neurology India. 2022 Mar-Apr:70(2):740-743. doi: 10.4103/0028-3886.344662. Epub [PubMed PMID: 35532651]
Kamble V, Lahoti AM, Dhok A, Taori A, Pajnigara N. A rare case of schizencephaly in an adult with late presentation. Journal of family medicine and primary care. 2017 Apr-Jun:6(2):450-452. doi: 10.4103/jfmpc.jfmpc_43_17. Epub [PubMed PMID: 29302567]
Level 3 (low-level) evidenceYoon JY, Kim DS, Kim GW, Ko MH, Seo JH, Won YH, Park SH. Motor Organization in Schizencephaly: Outcomes of Transcranial Magnetic Stimulation and Diffusion Tensor Imaging of Motor Tract Projections Correlate with the Different Domains of Hand Function. BioMed research international. 2021:2021():9956609. doi: 10.1155/2021/9956609. Epub 2021 Sep 6 [PubMed PMID: 34527746]
Rios LT, Araujo Júnior E, Nardozza LM, Caetano AC, Moron AF, Martins Mda G. Prenatal and Postnatal Schizencephaly Findings by 2D and 3D Ultrasound: Pictorial Essay. Journal of clinical imaging science. 2012:2():30. doi: 10.4103/2156-7514.96546. Epub 2012 May 23 [PubMed PMID: 22754744]
Bhatnagar S, Kuber R, Shah D, Kulkarni V. Unilateral closed lip schizencephaly with septo-optic dysplasia. Annals of medical and health sciences research. 2014 Mar:4(2):283-5. doi: 10.4103/2141-9248.129065. Epub [PubMed PMID: 24761255]
Level 3 (low-level) evidenceWatanabe J, Okamoto K, Ohashi T, Natsumeda M, Hasegawa H, Oishi M, Miyatake S, Matsumoto N, Fujii Y. Malignant Hyperthermia and Cerebral Venous Sinus Thrombosis After Ventriculoperitoneal Shunt in Infant with Schizencephaly and COL4A1 Mutation. World neurosurgery. 2019 Jul:127():446-450. doi: 10.1016/j.wneu.2019.04.156. Epub 2019 Apr 25 [PubMed PMID: 31029817]
Senol U, Karaali K, Aktekin B, Yilmaz S, Sindel T. Dizygotic twins with schizencephaly and focal cortical dysplasia. AJNR. American journal of neuroradiology. 2000 Sep:21(8):1520-1 [PubMed PMID: 11003289]
Level 3 (low-level) evidenceKim HJ, Koo YS, Yum MS, Ko TS, Lee SA. Cleft size and type are associated with development of epilepsy and poor seizure control in patients with schizencephaly. Seizure. 2022 May:98():95-100. doi: 10.1016/j.seizure.2022.04.002. Epub 2022 Apr 6 [PubMed PMID: 35462301]
Şah O, Türkdoğan D, Küçük S, Takış G, Asadov R, Öztürk G, Ünver O, Ekinci G. Neurodevelopmental Findings and Epilepsy in Malformations of Cortical Development. Turkish archives of pediatrics. 2021 Jul:56(4):356-365. doi: 10.5152/TurkArchPediatr.2021.20148. Epub 2021 Jul 1 [PubMed PMID: 35005731]
Park SH, Kim TJ, Ko SB. Super-refractory status epilepticus in a pregnant woman with schizencephaly. Epileptic disorders : international epilepsy journal with videotape. 2021 Jun 1:23(3):523-526. doi: 10.1684/epd.2021.1286. Epub [PubMed PMID: 34080976]
Jordan RD, Coscia M, Lantz P, Harrison W. Sudden Unexpected Death in Epilepsy: A Report of Three Commonly Encountered Anatomic Findings in the Forensic Setting With Recommendations for Best Practices. The American journal of forensic medicine and pathology. 2022 Sep 1:43(3):259-262. doi: 10.1097/PAF.0000000000000773. Epub 2022 May 28 [PubMed PMID: 35642769]
Battah A, DaCosta TR, Shanker E, Dacosta TJ, Farouji I. Schizencephaly as an Unusual Cause of Adult-Onset Epilepsy: A Case Report. Cureus. 2022 Jun:14(6):e25848. doi: 10.7759/cureus.25848. Epub 2022 Jun 11 [PubMed PMID: 35836438]
Level 3 (low-level) evidence