Introduction
Syncope may be caused by inadequate regulation of the heart and vessels function by the autonomic nervous and neuroendocrine systems. A tilt table test is a diagnostic procedure for patients with syncope of unknown origin. During the test, the patient is exposed to orthostatic stress, which may be exaggerated during the negative-passive phase of the test by nitroglycerin, clomipramine, and isoprenaline administration. A negative result tilt table test is characterized by a moderate increase in heart rate and the maintaining of the systolic blood pressure above 90 mmHg without symptoms during the planned duration of the study. The tilt table test may provoke a neurocardiogenic reflex with its vasodepressor and cardioinhibitory components. However, some other positive responses may be distinguished, for example, initial orthostatic hypotension, orthostatic hypotension, delayed orthostatic hypotension, and postural orthostatic tachycardia. The patient may present chronotropic incompetence when their heart rate does not increasemore than 5/min above baseline values. The neurocardiogenic reflex may occur suddenly or may be preceded by orthostatic hypotension or delayed orthostatic hypotension. Today, a tilt table test is believed to reveal susceptibility to reflex hypotension rather than the cause of the syncope.[1][2][3]
During the test, the patient may present pseudo-syncope often manifested by a sudden silence, head dropping, and closed eyes, which can not be opened, even with force. In such a case, the patient can maintain an upright position, and blood pressure and heart rate are within normal limits.[4][5]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
During a tilted position, blood flows into splanchnic and lower extremities veins. The blood volume in the central compartment is diminished. The nervous system increases the release of catecholamines and later activates the renin-angiotensin-aldosterone system and may increase the release of other neuropeptides like vasopressin, endothelin, and adrenomedullin to maintain homeostasis. The insufficiency of the autonomic nervous system and neurohumoral mechanism may lead to a decrease in blood pressure. Moreover, unknown mechanisms may trigger neurocardiogenic reflex, which may result in vasodilatation and cardio inhibition. Peripheral and central mechanisms may cause neurocardiogenic reflex.[6]
The reduced fluid intake increases the susceptibility to hemodynamic disturbances during the test. Furthermore, venous catheterization and the medical environment may facilitate the occurrence of the neurocardiogenic reflex.
The syncope may be preceded by prodromal symptoms like sweating, blurred vision, hot and cold flashes, weakness, loss of hearing, and nausea. Sometimes the loss of consciousness is sudden without prodromal symptoms even if the blood pressure and heart rate slowly decreased before syncope. The duration of unconsciousness is usually up to 20 seconds, but it may sometimes be longer, especially when tilt table downtime is prolonged or there is a very long pause of up to 60 seconds. During syncope, the patient's eyes are usually open, and urine incontinence, jerking movements, eye deviations, and vocalizations may occur. The patient is not able to maintain an upright position. If belts do not hold them, patients will fall. After regaining consciousness, a patient may recall some dreams, especially after a more extended period of unconsciousness.[7]
Some patients may deny the presence of loss of consciousness, but they admit that they do not recall the moment the tilt table lowered.
The patient may have nausea and vomiting after syncope. It usually lasts up to 15 to 30 minutes. Some patients report weakness after the test, which can last several hours, but often, the patient can stand up after 10 to 15 minutes.[8]
Indications
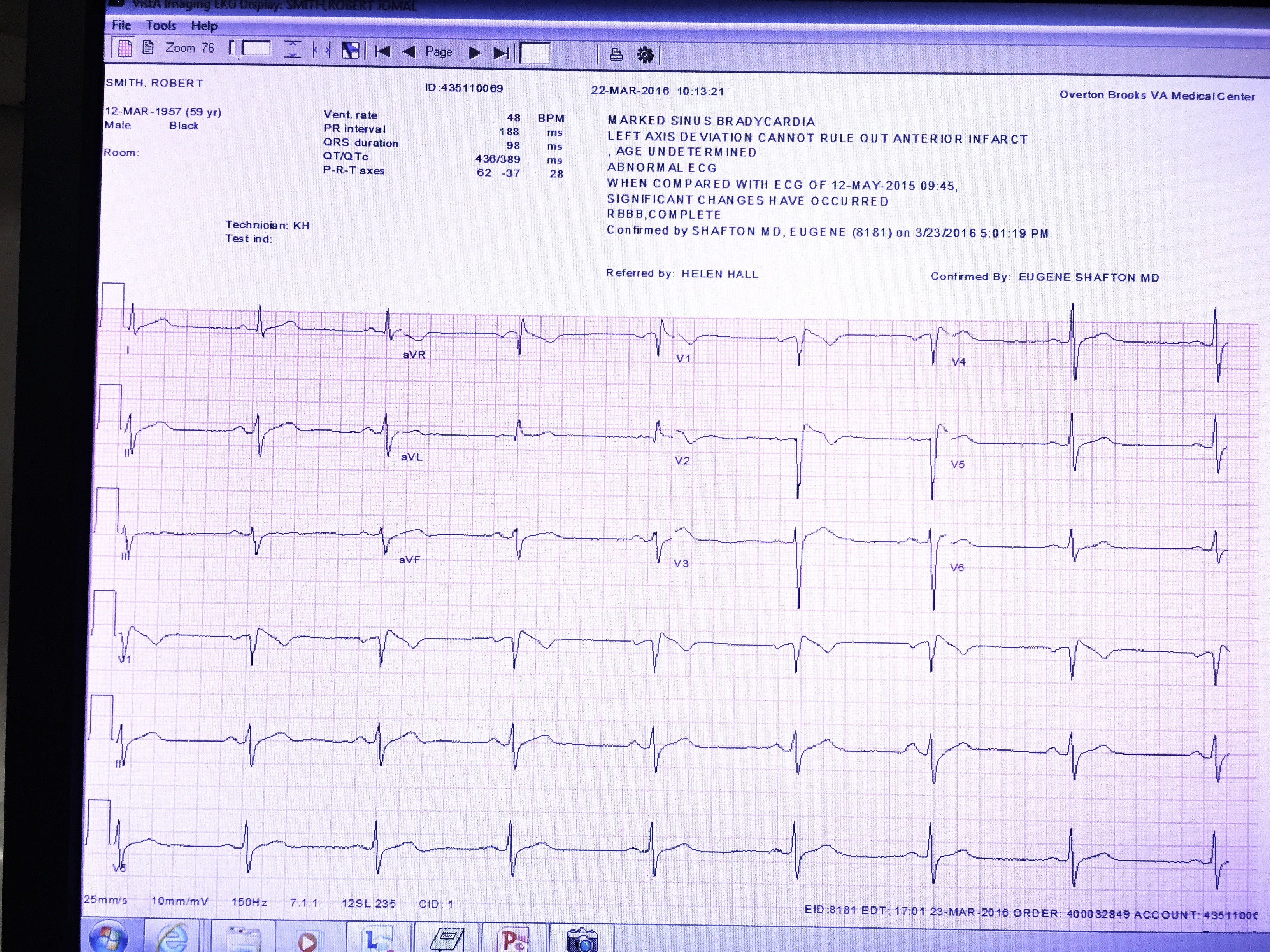
The tilt table test is an additional procedure performed after the initial evaluation of syncopal patients. The initial assessment consists of medical history, physical examination, orthostatic test (blood pressure in the supine position and after 1 to 3 minutes of standing), and a 12-lead electrocardiogram.[4][9][10]
The indications for the tilt table test include:
- Recurrent syncope of unknown origin
- Syncope of unknown origin with traumatic injury
- Even one syncopal event of unknown origin without a prodrome
- Suspicion of pseudo syncope or psychogenic syncope
- Jerking movements during the loss of consciousness to differentiate them from epilepsy
- A fall, which may mask syncope.
Contraindications
The contraindications for performing the tilt test include significant carotid artery stenosis, significant coronary artery stenosis, hypertrophic cardiomyopathy with outflow tract narrowing, severe anemia, known origin of the syncopal event, lack of syncopal events, falls, pre-syncopal events in medical history, and an unstable condition.
Equipment
The following equipment is required to perform the tilt table test: tilt table, blood pressure monitor, ECG monitor, nitroglycerin in spray or isoprenaline infusion, or clomipramine injection and cardioverter-defibrillator.
Personnel
The tilt table test can be performed by a trained nurse or medical doctor or both of them according to the local law. The providers should be certified and able to give basic life support (BLS) if needed.
Preparation
The patient should fast for at least 4 hours to avoid aspiration during vomiting in an unconscious state (which is rare). The examination may be performed when the patient is dressed in their usual clothes. The procedure and expectations should be explained to avoid unnecessary anxiety about the test. The patient should be informed about the risk of urinary incontinence or vomiting and have clothes to change into, if necessary.
Technique or Treatment
Before tilt table testing, the patient should stay in the supine position for at least 5 minutes. A long time in the supine position is required if venous catheterization is to be done before the test. The patient should be wrapped to avoid falls and traumatic injuries. Venous catheterization is not mandatory before tilt testing.
Blood pressure and ECG should be monitored. The best method to monitor blood pressure is to use continuous non-invasive blood pressure monitoring, but using a sphygmomanometer is allowed.
The tilt table test should be performed according to the chosen protocol. There are a few protocols that can be used. The best-known in medical practice is the Westminster protocol or the Italian protocol. During the tilt table test, the passive phase is recommended to last 20 to 45 minutes. Later, medication is given (most commonly 0.4 mg nitroglycerine sublingually) to increase the sensitivity of the test, but the provocation reduces the specificity, and the patient should be in an upright position for up to 15 minutes.
The tilt table test should be terminated at syncope or after protocol termination. Some patients have prolonged hypotension without loss of consciousness, and in this case, the termination of tilt testing during the pre-syncopal period may be considered, especially in elderly patients.In the case of a positive result during the tilt table test, the patient should be asked about reproducing symptoms in his or her daily life. The downtime should be shorter than 10 seconds. Lowering the tilt table for a longer period may result in a longer loss of consciousness. The changes in blood pressure and heart rate should be assessed.
Complications
The tilt table test is a safe procedure. However, myocardial infarction or stroke may develop in persons with significant coronary or carotid artery stenosis. This is very rare. Arrhythmic complications may be represented by prolonged bradycardia, which may be treated with atropine. Ventricular fibrillation is extremely rare. Some patients may vomit after tilt testing or have severe weakness lasting for several hours. A headache is common, especially after nitroglycerine use. A few seconds of extremity myoclonus is common after syncope is noted before returning to consciousness (convulsive syncope). This should not be confused by the providers for seizures.[11]
Clinical Significance
The cardioinhibitory component of neurocardiogenic reflex provoked during tilt testing is a significant concern for attending doctors because the decision to pace or not to pace needs to be considered. The proper management of patients with a cardioinhibitory form of neurocardiogenic reflex is still a matter of debate. Cases of pacemaker implantation in young people with a single syncopal event were reported during cardiology conferences. They were justified by the doctors who worry about the risk of cardiac arrest. However, this approach may lead to infectious complications, need for future reimplantation procedures, reduced quality of life, anxiety, and depression. The cardioinhibitory component may be related both to inhibition of sinus node presenting as sinus bradycardia or sinus standstill or inhibition of an atrioventricular node presenting as an atrioventricular block. The patients with an atrioventricular block during neurocardiogenic reflex provoked by tilt table tests have shorter prodromal symptom duration. They tend to have a longer PR interval on an electrocardiogram at baseline. At present, the appropriateness of pacing the patients with tilt table test induced asystole should be assessed in a clinical context. Elderly patients may be considered to be paced because of the risk of overlapping sick sinus syndrome or concealed dysfunction of the atrioventricular node. Pacing in patients at an age younger than 40 years is usually not indicated.
Enhancing Healthcare Team Outcomes
Clinicians should be aware that the tilt table is not 100% sensitive in making a diagnosis of syncope; other methods of evaluating the patient should also be undertaken.
The VASIS classification may be used when a neurocardiogenic reflex is provoked. In this case, mixed reaction, cardioinhibitory (asystole at least 3 seconds or bradycardia lower than 40/min lasting at least 10 seconds), and a vaso-depressive form may be recognized. However, other forms of hemodynamic instability may be present, including initial orthostatic hypotension, delayed orthostatic hypotension, or postural orthostatic tachycardia (increase in heart rate greater than 30/min or above 130/min). The neurocardiogenic reflex may be provoked by orthostatic hypotension or delayed orthostatic hypotension.[12][13][14][15]
Media
References
Kocyigit SE, Soysal P, Bulut EA, Aydin AE, Dokuzlar O, Isik AT. What is the relationship between frailty and orthostatic hypotension in older adults? Journal of geriatric cardiology : JGC. 2019 Mar:16(3):272-279. doi: 10.11909/j.issn.1671-5411.2019.03.005. Epub [PubMed PMID: 31080470]
De Maria B, Bari V, Cairo B, Vaini E, Esler M, Lambert E, Baumert M, Cerutti S, Dalla Vecchia L, Porta A. Characterization of the Asymmetry of the Cardiac and Sympathetic Arms of the Baroreflex From Spontaneous Variability During Incremental Head-Up Tilt. Frontiers in physiology. 2019:10():342. doi: 10.3389/fphys.2019.00342. Epub 2019 Apr 2 [PubMed PMID: 31001137]
Rodrigues V, Gomes TF, Silva AS, Rocha R, Ferrão A. Platypnoea-Orthodeoxia Syndrome: An Intriguing Diagnosis. European journal of case reports in internal medicine. 2019:6(2):001030. doi: 10.12890/2019_001030. Epub 2019 Feb 22 [PubMed PMID: 30931267]
Level 3 (low-level) evidenceCheshire WP Jr, Goldstein DS. Autonomic uprising: the tilt table test in autonomic medicine. Clinical autonomic research : official journal of the Clinical Autonomic Research Society. 2019 Apr:29(2):215-230. doi: 10.1007/s10286-019-00598-9. Epub 2019 Mar 5 [PubMed PMID: 30838497]
Heyer GL, Harvey RA, Islam MP. Signs of autonomic arousal precede tilt-induced psychogenic nonsyncopal collapse among youth. Epilepsy & behavior : E&B. 2018 Sep:86():166-172. doi: 10.1016/j.yebeh.2018.03.009. Epub 2018 Jul 25 [PubMed PMID: 30055943]
Stewart JM, Shaban MA, Fialkoff T, Tuma-Marcella B, Visintainer P, Terilli C, Medow MS. Mechanisms of tilt-induced vasovagal syncope in healthy volunteers and postural tachycardia syndrome patients without past history of syncope. Physiological reports. 2019 Aug:7(13):e14148. doi: 10.14814/phy2.14148. Epub [PubMed PMID: 31250563]
Heyer GL. Atypical Prodromal Symptoms Help to Distinguish Patients With Psychogenic Nonsyncopal Collapse Among Youth Referred for Fainting. Pediatric neurology. 2019 Jun:95():67-72. doi: 10.1016/j.pediatrneurol.2019.02.006. Epub 2019 Feb 13 [PubMed PMID: 30922770]
Wagoner AL, Tarbell SE, Shaltout HA, Diz DI, Weese-Mayer DE, Fortunato JE. Chronic nausea and orthostatic intolerance: Diagnostic utility of orthostatic challenge duration, Nausea Profile Questionnaire, and neurohumoral measures. Neurogastroenterology and motility. 2018 Nov:30(11):e13433. doi: 10.1111/nmo.13433. Epub 2018 Aug 13 [PubMed PMID: 30101470]
Buszko K, Kujawski S, Newton JL, Zalewski P. Hemodynamic Response to the Head-Up Tilt Test in Patients With Syncope as a Predictor of the Test Outcome: A Meta-Analysis Approach. Frontiers in physiology. 2019:10():184. doi: 10.3389/fphys.2019.00184. Epub 2019 Mar 7 [PubMed PMID: 30899228]
Level 1 (high-level) evidenceKim YH, Paik SH, V ZP, Jeon NJ, Kim BJ, Kim BM. Cerebral Perfusion Monitoring Using Near-Infrared Spectroscopy During Head-Up Tilt Table Test in Patients With Orthostatic Intolerance. Frontiers in human neuroscience. 2019:13():55. doi: 10.3389/fnhum.2019.00055. Epub 2019 Feb 19 [PubMed PMID: 30837856]
Shmuely S, Bauer PR, van Zwet EW, van Dijk JG, Thijs RD. Differentiating motor phenomena in tilt-induced syncope and convulsive seizures. Neurology. 2018 Apr 10:90(15):e1339-e1346. doi: 10.1212/WNL.0000000000005301. Epub 2018 Mar 16 [PubMed PMID: 29549227]
Momodu II, Okafor CN. Orthostatic Syncope (Archived). StatPearls. 2025 Jan:(): [PubMed PMID: 30725970]
Ninni S, Kouakam C, Szurhaj W, Baille G, Klug D, Lacroix D, Derambure P. Usefulness of head-up tilt test combined with video electroencephalogram to investigate recurrent unexplained atypical transient loss of consciousness. Archives of cardiovascular diseases. 2019 Feb:112(2):82-94. doi: 10.1016/j.acvd.2018.08.004. Epub 2018 Dec 29 [PubMed PMID: 30600217]
Hutt Centeno E, Mayuga KA. What can I do when first-line measures are not enough for vasovagal syncope? Cleveland Clinic journal of medicine. 2018 Dec:85(12):920-922. doi: 10.3949/ccjm.85a.17112. Epub [PubMed PMID: 30526751]
van Campen CLMC, Rowe PC, Visser FC. Low Sensitivity of Abbreviated Tilt Table Testing for Diagnosing Postural Tachycardia Syndrome in Adults With ME/CFS. Frontiers in pediatrics. 2018:6():349. doi: 10.3389/fped.2018.00349. Epub 2018 Nov 16 [PubMed PMID: 30505831]