 Anatomy, Shoulder and Upper Limb, Forearm Radial Artery
Anatomy, Shoulder and Upper Limb, Forearm Radial Artery
Introduction
The radial artery is 1 of 2 distal continuations of the brachial artery, the other being the ulnar artery. The radial artery supplies the anterior forearm compartment. The radial and ulnar arteries originate as axillary artery bifurcations in the cubital fossa and are major forearm perforators. Following its bifurcation, the radial artery runs along the forearm's lateral aspect between the brachioradialis and flexor carpi radialis (FCR).[1] The blood vessel splits into the superficial and deep palmar branches immediately proximal to the wrist, forming an anastomosis with the distal ulnar artery branches in the hand. The radial artery is superficial, easily palpated proximal to the wrist crease immediately lateral to the FCR tendon.
The radial artery is clinically important, as locating this vessel or its pulsations can guide various diagnostic and therapeutic procedures. Understanding radial anatomy and physiology can help clinicians treat various cardiovascular and musculoskeletal conditions.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Course
The radial artery originates from the brachial artery at the cubital fossa, medial to the biceps tendon, and courses anterior to the radial neck (see Image. Forearm Arteries). This vessel traverses the forearm's lateral aspect, deep to the brachioradialis muscle, accompanied by radial veins (venae comitantes). The radial artery is enclosed by superficial and deep fasciae, except proximally, where it overlaps with the brachioradialis muscle belly. The middle segment runs adjacent to the superficial branch of the radial nerve. The vessel continues distally between the brachioradialis and pronator teres, then between the brachioradialis and FCR.
In the distal 3rd of the forearm, the radial artery lies between the brachioradialis and FCR tendons, positioned anterior to the radius and pronator quadratus. The artery descends through the lateral intermuscular septum, which separates the forearm's flexor and extensor compartments. This location allows the vessel’s pulsations to be palpable in the distal forearm.
The distal segment of the radial artery curves over the wrist joint, passing beyond the styloid process into the 1st interosseous space. This vessel then travels deep to the abductor pollicis longus tendon and courses between the extensor pollicis longus and brevis in the anatomic snuffbox. Within this region, the vessel is closely related to the scaphoid and trapezium bones and is crossed by the cephalic vein and branches of the radial nerve. In the hand, the artery passes between the heads of the 1st dorsal interosseous muscle before turning medially through the adductor pollicis muscles.[2] The radial artery forms various anastomoses with the ulnar artery in the hand.
The radial artery's anatomical course and its surface location in the distal forearm make the vessel accessible for various clinical procedures, such as placing an arterial line, sampling blood, and harvesting for coronary artery bypass grafting (CABG). The vessel's anastomoses with the ulnar artery underscores its importance in maintaining adequate blood supply to the hand.[3]
Layers
Arterial walls consist of 3 tissue layers. The outermost layer is the tunica adventitia (tunica externa). The adventitia is composed of connective tissue, collagen, and elastic fibers, which allow arterial wall distension when luminal pressure changes.[4] The tunica media is the middle layer, comprised of circumferentially oriented smooth muscle and elastic fibers. The tunica intima is the innermost layer, consisting of an elastic membrane and smooth endothelial lining.
Functions
The radial artery primarily supplies blood to the wrist and hand, especially the lateral hand and 3 digits, as it has few proximal forearm branches. This vessel also contributes to the blood supply of several forearm muscles, the radial nerve, and the elbow joint.[5]
Embryology
Theories regarding upper limb arterial development are controversial. However, embryonic studies aided by 3-dimensional reconstructive imaging and molecular and genetic research provide a comprehensive picture of arterial formation. Vasculogenesis initiates blood vessel development through signaling pathways that stimulate hemangioblasts and endothelial cells to create primitive tubular networks. The cells involved differentiate into arterial and venous endothelial cells, creating the primary capillary plexus. This plexus undergoes angiogenesis, a remodeling and sprouting process regulated by a balance of activators and inhibitors in the signaling pathways. The capillary plexus extends throughout the upper limb by the 28th day of embryonic development.
Capillary maturation follows a proximodistal pattern of differentiation. Capillary plexus segments are either maintained, enlarged, or pruned in response to tissue demands. The maturation process is influenced by oxygenation and nutrient availability. The axillary and brachial arteries form by the 41st day. The forearm arteries and their branches are established by the 44th day, except for the distal radial artery. The presence of variant forearm arteries suggests that vessel formation has been disrupted between the 41st and 44th days of embryonic development.[6]
Blood Supply and Lymphatics
The branches of the radial artery are best organized by their anatomical location: forearm, wrist, or hand. The branches are listed below in order of their bifurcation points, from proximal to distal along the upper extremity.
Forearm
The radial artery's forearm branches include the radial recurrent, muscular, palmar carpal, and superficial palmar arteries. The radial recurrent artery originates inferior to the radial artery's origin, typically on the lateral aspect. This blood vessel travels proximally between branches of the radial nerve to anastomose at the elbow joint with the radial collateral artery, a branch of the deep artery of the arm.
Muscular branches perforate the radial forearm muscles as the radial artery courses distally. The palmar (volar) carpal branch arises near the distal aspect of the pronator quadratus, travels across the carpal bones, and anastomoses with the palmar carpal branch of the ulnar artery. The superficial palmar branch originates from the medial aspect of the radial artery over the radial styloid. This branch travels distally to anastomose with the ulnar artery's terminal branches to form the superficial palmar arch.
Wrist
The radial artery's branches in the carpal region include the dorsal carpal and 1st dorsal metacarpal arteries. The dorsal carpal branch arises distal to the radial styloid and travels superficially over the scaphoid. This artery anastomoses with the ulnar dorsal carpal branches to form the dorsal carpal arch. The 1st dorsal metacarpal artery originates at the level of the 1st metacarpal as the radial artery enters the palmar aspect of the hand to form the deep palmar arch. This branch is composed of 2 arteries that supply the medial aspect of the 1st digit and the lateral segment of the 2nd digit.
Hand
The radial artery's branches in the hand include the princeps pollicis, radialis indicis, and deep palmar arch (see Image. Arteries of the Hand). The princeps pollicis artery, or the principal artery of the thumb, arises as the radial artery courses medially. As its name implies, this branch supplies the thumb. The radialis indicis artery, or radial artery of the index finger, originates near the princeps pollicis and runs between the heads of the 1st dorsal interosseous muscle to supply the lateral aspect of the index finger. One anatomical variant has the radialis indicis branching from the princeps pollicis artery.
The deep palmar arch is formed primarily by the radial artery and lies across the metacarpal bases. This arterial arch gives rise to the princeps pollicis and 3 palmar metacarpal arteries before terminating in an anastomosis with the deep branch of the ulnar artery.
Nerves
Sympathetic nerves supply the radial artery, primarily through sympathetic branches of the C6 nerve root. The C7 nerve may also contribute to innervation on the radial side of the hand.
Describing autonomic nerves as having a sensory function presents a contradiction. The sympathetic nervous system, like the autonomic system in general, consists of a 2-neuron general visceral efferent (motor) pathway. However, sympathetic nerves also carry visceral sensory fibers. For example, cardiac sympathetic nerves provide sensory innervation to the heart, although some authorities suggest that the cardiac base may also receive vagal sensory input. This proposed vagal innervation has been cited as a potential explanation for precordial pain (a sympathetic function) radiating to the neck (a vagal function) in angina pectoris.
Muscles
The radial artery supplies the posterolateral aspect of the elbow joint, forearm, and wrist and perfuses the thumb and lateral index finger. The vessel passes deep to the brachioradialis, which narrows in the distal forearm before inserting on the styloid process of the radius. Beyond this point, the radial artery traverses the anatomical snuffbox (la tabatière anatomique de Cloquet) before passing between the 2 heads of the 1st dorsal interosseous muscle.
Physiologic Variants
The radial artery typically bifurcates in the antecubital fossa at the level of the radial neck and continues distally in the anterior forearm. Documented brachial artery variants include a high origin from the axillary or brachial artery, an origin beneath the pronator teres, or, in some cases, congenital absence.[7][8][9]
Rodríguez-Niedenführ et al used multiple terms to describe the concept of "high bifurcation." Haladaj et al reported that the previous nomenclature for high bifurcation included a double brachial artery, high brachial artery bifurcation, and the continuation of the superficial brachial artery as the radial artery. Haladaj et al propose the term "brachial radial artery" to mean that the radial artery had a high origin. In their study, a high radial artery origin was present in 9.2% of 120 cadavers, with 18.1% originating in the axillary cavity and the remaining 81.8% in the medial bicipital groove.[10]
In some individuals, the radial artery lies superficial in the forearm rather than beneath the brachioradialis. This variation increases the risk of arterial injury if the vessel is mistaken for the cephalic vein and used for infusion of a caustic substance. Strong pulsations help distinguish the radial artery from veins and aid in vessel localization during procedures. A superficial ulnar artery may also be present in some individuals.
Surgical Considerations
Radial Artery Laceration: Repair versus Ligation
Janice et al's 2015 study compared operative and nonoperative approaches to forearm lacerations, discovering that penetrating injuries may cause limb-threatening ischemia. Surgical management is necessary to restore blood flow. Given the rich anastomotic connections between the radial and ulnar arteries in the hand, isolated lacerations of either artery are not typically critical. Ligating a distal forearm artery is acceptable if the palmar arch provides adequate perfusion while hemostasis is inadequate.[11] Surgical repair is necessary for complex lacerations involving both the radial and ulnar arteries. The literature suggests that the magnitude of concomitant nerve, not arterial, injury accounts for functional disability.[12]
Coronary Artery Bypass Graft
Leonard et al's review compared the efficacies of the radial artery and saphenous vein when used as CABG conduits. The radial artery demonstrated superior patency in clinical trials and better clinical outcomes in observational studies.[13] Meanwhile, Debs et al showed that the frequency of functional radial artery graft occlusion was 12.0% compared to 19.7% when the saphenous vein was used. The study also showed that the incidence of complete radial artery graft occlusion was 8.9%, whereas complete saphenous vein graft occlusion occurred in 18.6%.[14]
Arteriovenous Fistulae
The radial artery is often used to create an arteriovenous fistula (AVF) for dialysis. Jennings et al reported that the proximal radial artery provided an excellent AVF site, reducing the risk of dialysis-related steal syndrome.[15] Although AVFs are generally recommended to be placed as distally as possible in the upper extremity, Wu et al documented a 12.3% primary failure rate for AVFs formed at the proximal radial artery.[16]
Carpal Tunnel Syndrome
Carpal tunnel syndrome is commonly due to a transverse carpal ligament abnormality, leading to median nerve compression. Other causes include diabetes mellitus, tumors, pregnancy, ganglionic compression, and overuse syndromes. An aberrant radial artery may lead to carpal tunnel syndrome with an incidence of less than 3%.[17] Such a vessel may arise as an anomalous superficial palmar branch of the radial artery, coursing through the carpal tunnel and compressing encased structures like the median nerve due to its large diameter.[18]
Clinical Significance
Pulse Palpation
Palpating the radial artery proximal to the wrist crease and immediately lateral to the FCR tendon is a common method for assessing pulse intensity and rate. The artery's pulsations may also be appreciated in the anatomical snuffbox as the vessel crosses the lateral aspect of the wrist. The tendon of the extensor pollicis longus muscle lies in the medial boundary of the snuffbox, while the extensor pollicis brevis and abductor pollicis longus tendons occupy the region's lateral border.[19] Brachial artery palpation may be necessary if the ulnar artery is not palpable and the radial pulse is weak.
The Allen and Modified Allen Tests
The hand is perfused by both the radial and ulnar arteries, which form a rich arterial plexus in the region. Compromised circulation in one artery may result in compensation by the other to ensure that the hand's blood supply is adequate.
The Allen test, first described by Edgar Van Nuys Allen in 1929, evaluates arterial blood flow to the hand. To perform the test, the patient elevates both arms above the head for 30 seconds to drain blood from the hands. The patient then clenches both fists tightly while the examiner occludes the radial arteries in both hands. Afterward, the patient rapidly opens both hands, and the examiner compares the color of the palms. Normal color should replace the initial pallor as the ulnar arteries restore perfusion. The test is then repeated with the ulnar arteries occluded instead. The time for normal color to return indicates the degree of collateral blood flow. A positive test indicates adequate circulation, with normal color returning to both hands when either artery is occluded alone. Persistent pallor suggests insufficient collateral blood supply.
The modified Allen test is an alternative proposed by Irving Wright that is considered superior to the original Allen test (see Video. Modified Allen Test). First, the patient either clenches their fist tightly or repeatedly opens and closes the hand before making a fist. The examiner then simultaneously compresses the radial and ulnar arteries, ceasing blood flow to the hand. Afterward, the elbow is extended fully, avoiding excessive extension that may yield a false positive result. The hand should appear pale when the fist is unclenched. The examiner then releases ulnar artery pressure and observes hand coloration, which should return within 10 seconds.
The test is repeated, with pressure released from the radial rather than the ulnar artery. Color is restored promptly in patients with good hand collateral circulation. Prolonged pallor after releasing arterial compression results from compromised flow in either artery, often from an occlusion.
The modified Allen test may be used to evaluate hand arterial blood flow adequacy in patients undergoing vascular access or surgery. Relevant procedures include arterial blood gas sampling, cannulation, catheterization, and radial artery graft harvest. The radial artery can be a suitable CABG source due to its caliber. Performing an Allen or modified Allen test before these procedures helps determine the risk of hand ischemia.
These tests also help assess whether radial artery ligation can be performed during emergencies. For example, reanastomosis is the preferred method for restoring blood flow in a lacerated radial artery. However, the unavailability of a vascular surgeon during a vascular emergency often necessitates radial artery ligation, which requires evaluating collateral circulation with the Allen or modified Allen test. The intact ulnar artery should enable the medial fingers to return to normal color. The primary concern is whether the princeps pollicis and radialis indicis arteries provide sufficient retrograde perfusion to the thumb and index finger. An alternative approach should be sought if these digits remain pale after releasing ulnar artery compression.
Arteriolar Constriction in a Cold Environment
Cold environments trigger arteriolar constriction in the hand, a process regulated by the sympathetic nervous system. Epinephrine and norepinephrine stimulate α1 receptors on arteriolar smooth muscle, inducing contraction and vasoconstriction. This valuable physiological adaptation minimizes heat loss from the fingers and toes. However, excessive vasoconstriction in extreme conditions may result in frostbite and subsequent gangrene, leading to digital loss.
Fracture of the Scaphoid
The radial artery supplies the scaphoid bone through its dorsal carpal branch. A fall on an outstretched hand may fracture this wrist bone. Aging-related bone mass decline increases the likelihood of this injury in older individuals, who also have a higher risk of falls. Immediate diagnosis and initial wrist splinting are essential for proper management.
However, a scaphoid fracture may not become evident on a radiograph for up to 10 days when the bone has degenerated enough for the fracture to be visible. A scaphoid fracture may be diagnosed by gently putting manual pressure on the thumb's carpometacarpal joint in the anatomical snuffbox. The maneuver elicits pain if the scaphoid is fractured. Failure to splint the wrist following a scaphoid fracture may compromise blood supply to the fractured segment, leading to permanent nonunion. The avascularized bone can degenerate, causing chronic pain and disability.
Media
(Click Image to Enlarge)
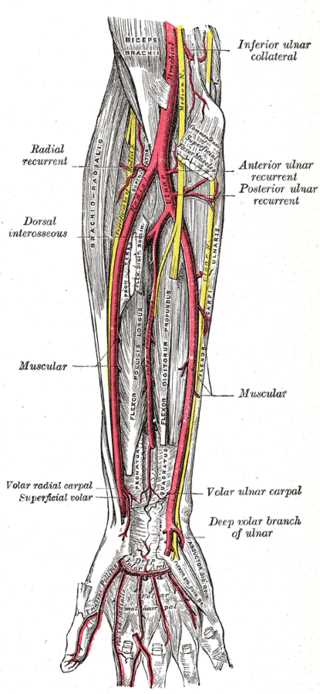
Forearm Arteries. This image highlights the ulnar artery's deep palmar branch and the radial, ulnar, anterior and posterior ulnar recurrent, dorsal interosseous, volar interosseous (termination), dorsal ulnar carpal, dorsal radial carpal arteries, muscular, radial recurrent, volar radial carpal, superficial volar, and volar ulnar carpal arteries. The arm's inferior ulnar collateral and profunda brachii arteries and the ulnar artery's deep volar branch in the hand are also shown.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)

Arteries of the Hand. Shown here are the ulnar artery, radial artery, deep palmar arch, superficial palmar arch, common palmar digital arteries, proper palmar digital arteries, radial artery of the index finger (radialis indicis), and digital artery to the thumb (princeps pollicis).
StatPearls Publishing Illustration
(Click Video to Play)
Modified Allen Test. The modified Allen test evaluates whether the ulnar artery can adequately supply blood to the hand if the radial artery is ligated, such as during a radial forearm flap harvest.
Contributed by MH Hohman, MD, FACS
References
Beutel BG, Worley C, Zisquit J, Nedeff N. Allen Test. StatPearls. 2025 Jan:(): [PubMed PMID: 29939593]
Narsinh KH, Mirza MH, Duvvuri M, Caton MT Jr, Baker A, Winkler EA, Higashida RT, Halbach VV, Amans MR, Cooke DL, Hetts SW, Abla AA, Dowd CF. Radial artery access anatomy: considerations for neuroendovascular procedures. Journal of neurointerventional surgery. 2021 Dec:13(12):1139-1144. doi: 10.1136/neurintsurg-2021-017871. Epub 2021 Sep 22 [PubMed PMID: 34551992]
Alasmari WA. The morphometric anatomy and clinical importance of the radial artery. Folia morphologica. 2021:80(4):839-844. doi: 10.5603/FM.a2020.0139. Epub 2020 Nov 26 [PubMed PMID: 33241849]
Tucker WD, Arora Y, Mahajan K. Anatomy, Blood Vessels. StatPearls. 2025 Jan:(): [PubMed PMID: 29262226]
Berezovsky DR, Bordoni B. Anatomy, Shoulder and Upper Limb, Forearm Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 31424739]
Kumka M, Purkiss S. A rare case of unilateral variations of forearm arteries: anatomy, embryology and clinical implications. The Journal of the Canadian Chiropractic Association. 2015 Sep:59(3):253-60 [PubMed PMID: 26500359]
Level 3 (low-level) evidenceRodríguez-Niedenführ M, Vázquez T, Nearn L, Ferreira B, Parkin I, Sañudo JR. Variations of the arterial pattern in the upper limb revisited: a morphological and statistical study, with a review of the literature. Journal of anatomy. 2001 Nov:199(Pt 5):547-66 [PubMed PMID: 11760886]
Level 1 (high-level) evidenceFunk GF, Valentino J, McCulloch TM, Graham SM, Hoffman HT. Anomalies of forearm vascular anatomy encountered during elevation of the radial forearm flap. Head & neck. 1995 Jul-Aug:17(4):284-92 [PubMed PMID: 7672968]
Level 3 (low-level) evidenceZheng Y, Shao L, Mao JY. Bilaterally symmetrical congenital absence of radial artery: a case report. BMC surgery. 2014 Mar 21:14():15. doi: 10.1186/1471-2482-14-15. Epub 2014 Mar 21 [PubMed PMID: 24650137]
Level 3 (low-level) evidenceHaładaj R, Wysiadecki G, Dudkiewicz Z, Polguj M, Topol M. The High Origin of the Radial Artery (Brachioradial Artery): Its Anatomical Variations, Clinical Significance, and Contribution to the Blood Supply of the Hand. BioMed research international. 2018:2018():1520929. doi: 10.1155/2018/1520929. Epub 2018 Jun 11 [PubMed PMID: 29992133]
Thai JN, Pacheco JA, Margolis DS, Swartz T, Massey BZ, Guisto JA, Smith JL, Sheppard JE. Evidence-based Comprehensive Approach to Forearm Arterial Laceration. The western journal of emergency medicine. 2015 Dec:16(7):1127-34. doi: 10.5811/westjem.2015.10.28327. Epub 2015 Dec 11 [PubMed PMID: 26759666]
Brown KR, Jean-Claude J, Seabrook GR, Towne JB, Cambria RA. Determinates of functional disability after complex upper extremity trauma. Annals of vascular surgery. 2001 Jan:15(1):43-8 [PubMed PMID: 11221943]
Level 2 (mid-level) evidenceLeonard JR, Abouarab AA, Tam DY, Girardi LN, Gaudino MFL, Fremes SE. The radial artery: Results and technical considerations. Journal of cardiac surgery. 2018 May:33(5):213-218. doi: 10.1111/jocs.13533. Epub 2018 Feb 5 [PubMed PMID: 29405454]
Deb S, Cohen EA, Singh SK, Une D, Laupacis A, Fremes SE, RAPS Investigators. Radial artery and saphenous vein patency more than 5 years after coronary artery bypass surgery: results from RAPS (Radial Artery Patency Study). Journal of the American College of Cardiology. 2012 Jul 3:60(1):28-35. doi: 10.1016/j.jacc.2012.03.037. Epub [PubMed PMID: 22742399]
Level 1 (high-level) evidenceJennings WC, Mallios A, Mushtaq N. Proximal radial artery arteriovenous fistula for hemodialysis vascular access. Journal of vascular surgery. 2018 Jan:67(1):244-253. doi: 10.1016/j.jvs.2017.06.114. Epub 2017 Sep 11 [PubMed PMID: 28912005]
Wu CC, Jiang H, Cheng J, Zhao LF, Sheng KX, Chen JH. The outcome of the proximal radial artery arteriovenous fistula. Journal of vascular surgery. 2015 Mar:61(3):802-8. doi: 10.1016/j.jvs.2014.08.112. Epub [PubMed PMID: 25720933]
Level 1 (high-level) evidenceKokkalis ZT, Tolis KE, Megaloikonomos PD, Panagopoulos GN, Igoumenou VG, Mavrogenis AF. Aberrant Radial Artery Causing Carpal Tunnel Syndrome. The archives of bone and joint surgery. 2016 Jun:4(3):282-4 [PubMed PMID: 27517078]
Gwynne-Jones DP, Hartnett NI. Aberrant radial artery seen in the carpal tunnel at carpal tunnel decompression: case report. The Journal of hand surgery. 2008 Jul-Aug:33(6):885-7. doi: 10.1016/j.jhsa.2008.02.005. Epub [PubMed PMID: 18656760]
Level 3 (low-level) evidenceEpperson TN, Varacallo MA. Anatomy, Shoulder and Upper Limb, Brachial Artery. StatPearls. 2025 Jan:(): [PubMed PMID: 30725830]