Introduction
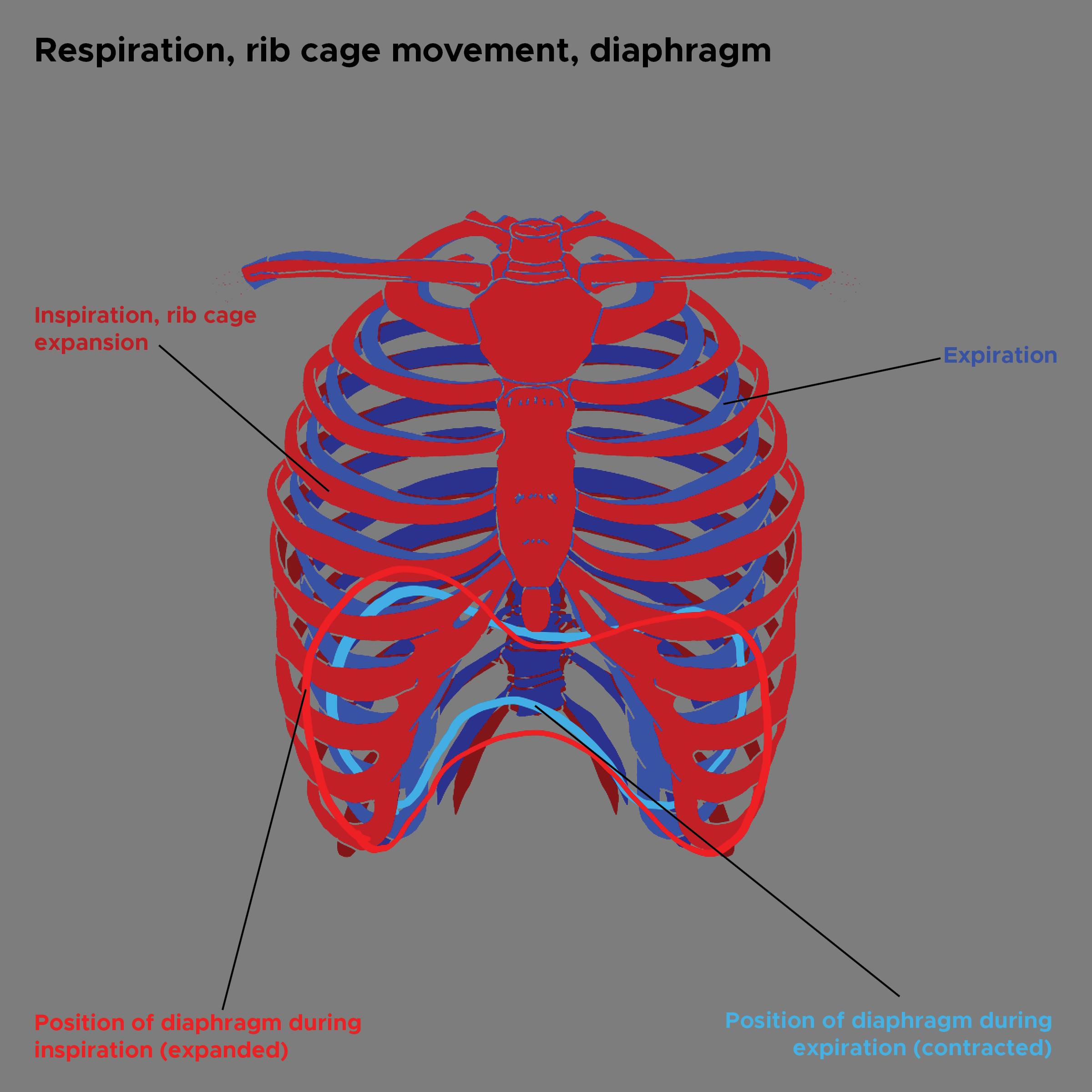
Pulmonary ventilation, more commonly called breathing, is the air movement into and out of the lungs. Inhalation is the act of drawing air into the lungs, while exhalation is the expulsion of that air. Breathing involves Boyle’s law, which states that the pressure of a gas decreases as the volume increases if the temperature is held constant.[1] Increasing the thoracic cavity volume causes a decrease in the intrathoracic pressure and an influx of air. Meanwhile, decreasing the volume of the thoracic cavity generally occurs through the relaxation of the muscles of inspiration, which causes an increase in intrathoracic pressure and results in exhalation (see Image. Respiration Rib Cage Movement, Diaphragm). The thoracic wall is essential to this process and comprises the sternum, 12 pairs of ribs, 12 thoracic vertebrae, and the muscles, fascia, and skin that connect to this bony cage.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The thoracic wall protects the heart, lungs, great vessels, and some abdominal organs. Additionally, the bony structures provide attachment points for muscles and allow for the mechanical function of ventilation. Ribs are curved, flat bones that attach posteriorly to vertebrae and anteriorly to the sternum. Ribs originate at each thoracic vertebra. The head of each rib has 1 or 2 facets for articulation, with the costal facets on the bodies of thoracic vertebrae. Ribs 1, 10, 11, and 12 have a single facet on their head that only articulates with its respective vertebra. Ribs 2 through 9 all have 2 facets on their heads; the superior facet articulates with the vertebra above the rib, while the inferior facet articulates with the respectively named vertebra. In addition, ribs 1 through 10 have tubercles with facets that articulate with each vertebra's costal facet of the transverse process.[2]. Ribs 11 and 12 have no tubercle and, therefore, do not articulate with the transverse process of their respective vertebra.
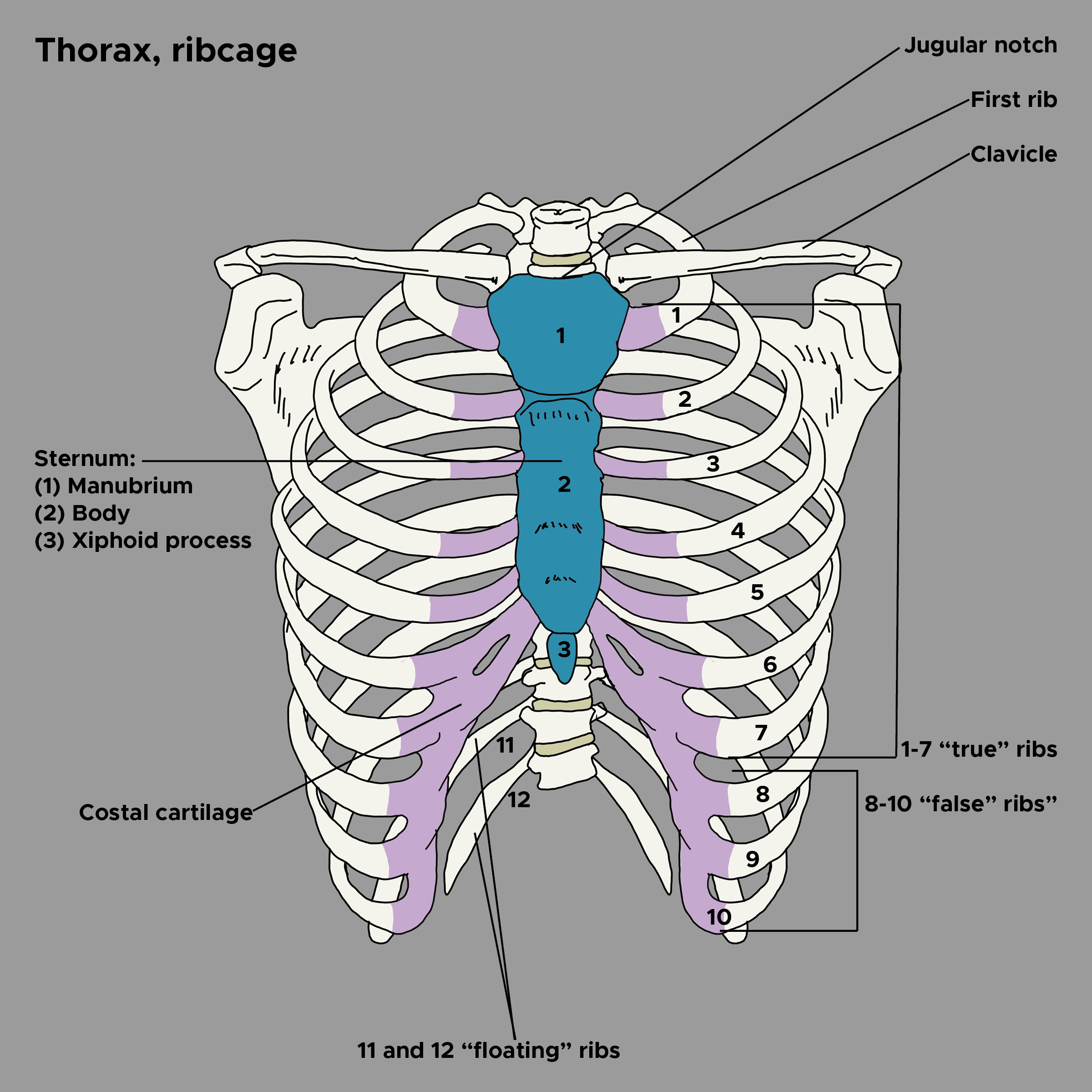
The sternum comprises 3 parts: the manubrium, body, and xiphoid process.[3] The manubrium is the widest portion and contains the jugular or sternal and clavicular notch. The sternal angle, or angle of Louis, is where the manubrium joins the body of the sternum. The second rib attaches at this point. The xiphoid process is attached inferiorly to the body of the sternum and provides an attachment point for the diaphragm and rectus abdominis muscles, but no ribs. Ribs 1 through 7 are considered true, or vertebrocostal, ribs and attach directly to the sternum. Ribs 8 through 10 are considered false, or vertebrochondral, ribs in which the cartilage of each rib attaches to the cartilage of the rib above it, which terminates where the seventh rib attaches to the sternum. Ribs 11 and 12 are considered floating, vertebral, or free ribs because they terminate in the posterior abdominal musculature and do not attach to the sternum. The costal cartilage of ribs 1 through 10 facilitates the elastic recoil of the thoracic wall, contributing to passive exhalation (see Image. Bones and Cartilage of Thorax).
Embryology
The thoracic wall forms part of the axial skeleton and comprises segmental bone, muscle, and connective tissue. These elements are derived from the paraxial mesoderm, which forms somites from which the sclerotome, myotome, and dermatome separate. The sclerotome originates from the vertebrae and transverse elements, which begin elongating into ribs during the fifth week of gestation. Ossification begins during the fetal period but is not completed until adulthood.[4] The myotome gives rise to the muscles of the thoracic wall. The sternum forms from sternal bars that meet in the midline and begin to fuse during the seventh week of gestation. Fusion starts superiorly and ends inferiorly by the tenth week.[5]
Blood Supply and Lymphatics
Each intercostal space receives its blood supply from 3 arteries: a posterior intercostal artery and a pair of anterior intercostal arteries. The posterior arteries of the first 2 intercostal spaces are fed from the superior (supreme) intercostal artery, which comes off the subclavian artery.[6] The remaining pairs of posterior intercostal arteries and a pair of subcostal arteries emerge directly from the thoracic aorta.[7] These posterior arteries enter the costal groove near the angle of each rib, where they travel between the intercostal vein and nerve. The posterior and anterior intercostal arteries anastomose laterally. The internal thoracic artery is another branch of the subclavian artery that supplies the anterior intercostal arteries of spaces 1 through 6 before dividing into the superior epigastric and musculophrenic arteries.[8] The musculophrenic artery supplies the anterior intercostal arteries of spaces 7 through 9. The 2 most inferior intercostal spaces are supplied from the posterior intercostal arteries and their collateral branches and do not have anterior intercostal arteries.
The intercostal veins run most superiorly in the costal grooves. There are 11 posterior intercostal veins and 1 pair of subcostal veins. Like the posterior arteries, the posterior veins also anastomose with the anterior intercostal veins. Several of the superior posterior intercostal veins typically merge to form the left and right superior intercostal veins at the level of T3 or T4, which can then empty into the brachiocephalic vein or the superior vena cava.[9] The remaining posterior intercostal veins end at the azygos vein before emptying into the superior vena cava. The internal thoracic veins accompany the internal thoracic arteries before emptying into the brachiocephalic vein.
Nerves
The medulla oblongata's respiratory center controls the ventilation rate and depth. While the dorsal respiratory group controls the motor neurons for all inspiration, the ventral respiratory group controls forced exhalation since normal exhalation is passive. The phrenic nerve is a branch of the cervical plexus. It originates mostly from C4, with some involvement of C3 and C5. The right and left sides travel through the neck and thorax before innervating the diaphragm.[10]. The anterior rami of spinal nerves T1 through T11 forms the intercostal nerves, while the anterior rami of spinal nerve T12 forms the subcostal nerve.[11] A portion of the anterior ramus of T1 forms part of the brachial plexus. However, the remaining intercostal nerves do not form plexuses. While the afferent fibers of these nerves conduct sensory information, including that of the overlying skin, the efferent fibers relay motor information to the muscles of respiration.
Muscles
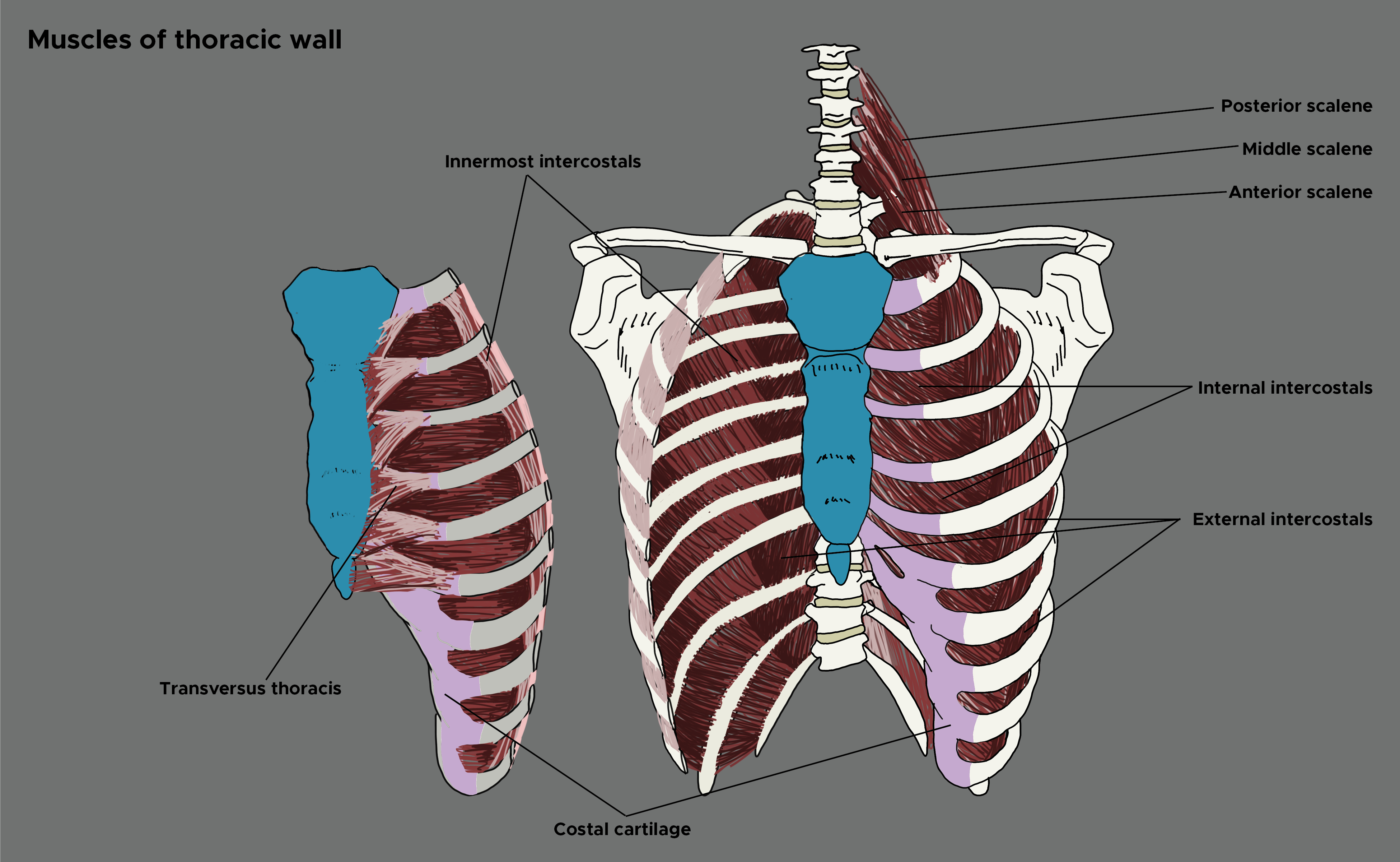
The musculature of the thoracic wall can be divided into 2 groups: those involved in inhalation and those responsible for forced exhalation (see Image. Muscles of the Thoracic Wall). During inhalation, the thorax's anterior-posterior, vertical, and transverse dimensions are increased. Contraction of the dome-shaped diaphragm causes the central tendon to be pulled inferiorly, flattening the diaphragm and increasing the vertical dimensions of the thorax.[12] Contraction of the external intercostals raises the lateral part of the ribs, causing a bucket handle motion that increases the transverse diameter of the thorax. The vertebrosternal ribs also follow a pump handle motion, which raises the sternum and increases the anterior-posterior dimensions of the thorax. The muscles of the neck can assist in this action.
Beyond the diaphragm compressing the abdominal cavity and the external intercostals lifting the ribs, the serratus posterior superior attaches to ribs 2 through 5 and elevates them during inhalation. When the neck is fixed, the scalene helps to elevate the first and second ribs. Likewise, the sternocleidomastoid can assist in raising the sternum.[13]. When needed, the pectoralis minor assists in lifting third, fourth, and fifth ribs. Numerous muscles aid in forced exhalation. The internal intercostals are located deep to the external intercostals. While the external intercostals run inferomedially from the superior rib to the adjacent inferior rib, the internal intercostals lie perpendicularly to the externals. This allows them to depress the ribs. The transversus thoracis spreads across the inner surface of the thoracic cage from the lower posterior sternum to ribs 2 through 6.[14] The transversus thoracis aids in depressing the ribs. Similarly, the serratus posterior inferior attaches the vertebrae to ribs 8 through 12 and depresses them during contraction.
Physiologic Variants
The body of the sternum is usually longer and thicker in males and shorter and thinner in females. This can be used to assist in the determination of biological sex in skeletal remains.[15] Additionally, many variations in sternum and rib formation exist. A bifid xiphoid or even a bifid sternum can be seen.[3] Similarly, a sternal foramen is caused by incomplete ossification of the left and right centers. The sternal foramen can be misidentified as a penetrating injury on X-rays or could lead to significant injury since the sternum is a common site for acupuncture. Like a sternal foramen, ectopia cordis is a congenital condition due to a more significant malformation of the sternum.[16] The thoracic wall may expose the heart due to the maldevelopment of the sternum and the pericardium.
Bifid ribs occur when the anterior portion of a rib splits into 2 before reaching the sternum. The corresponding musculature, blood vessels, and nerves also bifurcate. Bifid ribs are usually unilateral and asymptomatic.[17] Cervical and lumbar ribs are also potential anatomic abnormalities. If the costal element of the seventh cervical vertebrae elongates, it can form a cervical rib, although it usually does not reach the sternum. This same anomaly can occur at the level of L1, forming a lumbar rib. Furthermore, a lack of elongation of the costal element of the 12th rib can cause it to fail to develop. This leaves some people with only 11 ribs.
Surgical Considerations
Some essential surgical considerations regarding the thorax pertain to needle decompression and chest tube placement. As discussed, the blood vessels and nerves of the anterior thorax follow the costal groove on the inferior aspect of each rib.[11] Therefore, needle thoracostomy should be completed by piercing over the superior aspect of the rib on the affected side. Several sites have been studied, including the second intercostal space at the midclavicular line and the fourth and fifth intercostal spaces at the anterior axillary line.[18] Similarly, chest tube placement (tube thoracostomy) should be performed in the fourth or fifth intercostal space and track above the rib. Chest tubes should be placed between the mid to anterior axillary line.[19] Lastly, while performing a left-sided thoracotomy, providers must remember that the left phrenic nerve runs along the pericardium and should be avoided to reduce the risk of phrenic nerve palsy.[20]
Clinical Significance
Accessory muscle use generally involves activating inactive muscles to aid in ventilation. While this can be a normal finding during activities such as exercise or singing, it is important in patients who are at rest. The list of accessory muscles includes but is not limited to, the scalenes, sternocleidomastoids, internal intercostals, transversus thoracis, pectoralis major and minor, serratus anterior, serratus posterior superior and inferior, latissimus dorsi, trapezius, and the muscles of the abdominal wall. [13],[21] Injury to the brain, spinal cord, or phrenic nerve can paralyze the diaphragm and prevent patients from being able to breathe, thus requiring artificial ventilation.[10] Injury most commonly occurs at or above the level of C4. Infection with poliomyelitis (polio) has caused similar symptoms in the past. Hemi-diaphragm is another nerve-related finding. It occurs when there has been an injury or lesion to 1 side of the phrenic nerve, causing paradoxical, or the opposite of normal, motion of 1 side of the diaphragm during inhalation.
A pneumothorax occurs when free air enters the pleural cavity between the parietal and visceral pleurae. This may cause atelectasis or deflation of the affected lung. A pneumothorax can be caused by an internal insult such as a ruptured bleb or an external injury such as a broken rib or penetrating wound. Treatment may require the removal of the free air by thoracentesis/needle thoracotomy or the placement of a chest tube.[19] A flail chest occurs when 2 or more ribs have been fractured in 2 or more locations, causing a free-moving segment.[22] Early on, this segment may be internally splinted by the intercostal muscles. With fatigue, the segment eventually shows a paradoxical motion to the rest of the chest wall. This may significantly impair ventilation.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
West JB. The original presentation of Boyle's law. Journal of applied physiology (Bethesda, Md. : 1985). 1999 Oct:87(4):1543-5 [PubMed PMID: 10517789]
Waxenbaum JA, Reddy V, Futterman B. Anatomy, Back, Thoracic Vertebrae. StatPearls. 2024 Jan:(): [PubMed PMID: 29083651]
Kirum GG, Munabi IG, Kukiriza J, Tumusiime G, Kange M, Ibingira C, Buwembo W. Anatomical variations of the sternal angle and anomalies of adult human sterna from the Galloway osteological collection at Makerere University Anatomy Department. Folia morphologica. 2017:76(4):689-694. doi: 10.5603/FM.a2017.0026. Epub 2017 Mar 29 [PubMed PMID: 28353306]
Monsoro-Burq AH. Sclerotome development and morphogenesis: when experimental embryology meets genetics. The International journal of developmental biology. 2005:49(2-3):301-8 [PubMed PMID: 15906245]
Level 3 (low-level) evidenceJ AR, G M, K M, P R. Closing the cleft over a throbbing heart: neonatal sternal cleft. BMJ case reports. 2014 Jul 4:2014():. doi: 10.1136/bcr-2014-204529. Epub 2014 Jul 4 [PubMed PMID: 25100810]
Level 3 (low-level) evidenceGailloud P. The supreme intercostal artery includes the last cervical intersegmental artery (C7) - angiographic validation of the intersegmental nomenclature proposed by Dorcas Padget in 1954. Anatomical record (Hoboken, N.J. : 2007). 2014 May:297(5):810-8. doi: 10.1002/ar.22893. Epub 2014 Mar 7 [PubMed PMID: 24610867]
Level 1 (high-level) evidenceShimizu S, Tanaka R, Kan S, Suzuki S, Kurata A, Fujii K. Origins of the segmental arteries in the aorta: an anatomic study for selective catheterization with spinal arteriography. AJNR. American journal of neuroradiology. 2005 Apr:26(4):922-8 [PubMed PMID: 15814947]
Berdajs D, Zünd G, Turina MI, Genoni M. Blood supply of the sternum and its importance in internal thoracic artery harvesting. The Annals of thoracic surgery. 2006 Jun:81(6):2155-9 [PubMed PMID: 16731146]
Kutoglu T, Turut M, Kocabiyik N, Ozan H, Yildirim M. Anatomical analysis of azygos vein system in human cadavers. Romanian journal of morphology and embryology = Revue roumaine de morphologie et embryologie. 2012:53(4):1051-6 [PubMed PMID: 23303031]
Oliver KA, Ashurst JV. Anatomy, Thorax, Phrenic Nerves. StatPearls. 2024 Jan:(): [PubMed PMID: 30020697]
Baxter CS, Singh A, Ajib FA, Fitzgerald BM. Intercostal Nerve Block. StatPearls. 2024 Jan:(): [PubMed PMID: 29489198]
Shahid Z, Burns B. Anatomy, Abdomen and Pelvis: Diaphragm. StatPearls. 2024 Jan:(): [PubMed PMID: 29262082]
Watson AH, Williams C, James BV. Activity patterns in latissimus dorsi and sternocleidomastoid in classical singers. Journal of voice : official journal of the Voice Foundation. 2012 May:26(3):e95-e105. doi: 10.1016/j.jvoice.2011.04.008. Epub 2011 Jul 2 [PubMed PMID: 21724365]
Jelev L, Hristov S, Ovtscharoff W. Variety of transversus thoracis muscle in relation to the internal thoracic artery: an autopsy study of 120 subjects. Journal of cardiothoracic surgery. 2011 Jan 27:6():11. doi: 10.1186/1749-8090-6-11. Epub 2011 Jan 27 [PubMed PMID: 21272314]
Level 2 (mid-level) evidenceRamadan SU, Türkmen N, Dolgun NA, Gökharman D, Menezes RG, Kacar M, Koşar U. Sex determination from measurements of the sternum and fourth rib using multislice computed tomography of the chest. Forensic science international. 2010 Apr 15:197(1-3):120.e1-5. doi: 10.1016/j.forsciint.2009.12.049. Epub 2010 Jan 18 [PubMed PMID: 20083365]
Tadele H, Chanie A. Thoracic Ectopia Cordis in an Ethiopian Neonate. Ethiopian journal of health sciences. 2017 Mar:27(2):203-205 [PubMed PMID: 28579717]
Davran R, Bayarogullari H, Atci N, Kayali A, Ozturk F, Burakgazi G. Congenital abnormalities of the ribs: evaluation with multidetector computed tomography. JPMA. The Journal of the Pakistan Medical Association. 2017 Feb:67(2):178-186 [PubMed PMID: 28138167]
Paydar S, Farhadi P, Ghaffarpasand F. Advanced Trauma Life Support (ATLS) Tips to Be Kept In Mind. Bulletin of emergency and trauma. 2013 Jan:1(1):49-51 [PubMed PMID: 27162823]
Ravi C, McKnight CL. Chest Tube. StatPearls. 2024 Jan:(): [PubMed PMID: 29083704]
Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma-a review. Injury. 2006 Jan:37(1):1-19 [PubMed PMID: 16410079]
Katagiri M, Abe T, Yokoba M, Dobashi Y, Tomita T, Easton PA. Neck and abdominal muscle activity during a sniff. Respiratory medicine. 2003 Sep:97(9):1027-35 [PubMed PMID: 14509557]
Davignon K, Kwo J, Bigatello LM. Pathophysiology and management of the flail chest. Minerva anestesiologica. 2004 Apr:70(4):193-9 [PubMed PMID: 15173695]