Introduction
Major basic protein (MBP) is an eosinophil granule protein. Eosinophil granules contain a crystalloid core comprised of MBP and a matrix consisting of other toxic and pro-inflammatory mediators. MBP is the predominant constituent in eosinophil granules. MBP derives its name from research in guinea pig eosinophils that showed MBP was the majority protein in secondary granules. Increased concentrations of MBP and other cationic proteins have shown correlations with atopic diseases, parasitic infections, and other eosinophil-associated inflammatory processes.
Cellular Level
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Cellular Level
MBP is a 13.8 kDa protein rich in arginine with an isoelectric point (pI) of 11.4.[1][2] The cationic properties of MBP have a link to many of its essential functions. Studies of MBP mRNA have shown that MBP is synthesized from a pre-proform. The pre-portion serves as a signal sequence. The pro-portion is highly acidic and rich in glutamic acid.[3] Some studies have suggested it may play a role in protecting eosinophils from damage during protein processing from the Golgi apparatus to secondary granules.[4]
The MBP proform (proMBP) is absent in mature eosinophils. The exact trigger for cleavage of proMBP to MBP is not known. Interleukin-5 (IL-5) is known to stimulate the maturation of eosinophils within the bone marrow and serve as a chemotaxis agent at sites of inflammation. IL-5 also stimulates the synthesis of proteins in eosinophil granules.
Studies of IL-5 stimulated umbilical cord precursor cells identified a homolog of MBP named MBP2.[4] Both proteins have similar molecular masses, but with a pI of 8.7, MBP2 has a much lower positive charge than MBP.[4] Although MBP is present in eosinophils, basophils, and other cells, MBP2 has, so far, only been identified in eosinophils, making it a potentially useful biomarker for eosinophilic disorders.[4] MBP and MBP2 have similar biological effects, at least in vitro, despite their differences in cell localization and pI.
Organ Systems Involved
Eosinophil-mediated diseases involving the lungs, heart, skin, and gut are the best studied and characterized.[5] However, almost any tissue or organ can be affected:
- Cardiovascular
- Gastrointestinal
- Pulmonary
- Renal
- Neurologic
- Skin
Function
- Host defense against parasitic infections, such as Trichinella spiralis and Schistosoma mansoni.[6]
- Activation of mast cells, basophils, and neutrophils during inflammation.[7]
- Complement activation through alternative and classical pathways.[8]
- Platelet agonist[9]
- Antibacterial activity[10]
- Natural protein inhibitor of heparanase - heparanase has been implicated in inflammation and inflammation-associated cancer due to its ability to degrade the extracellular matrix scaffold and potentially assist with penetration of eosinophils into other tissues.[11][12]
Additional functions more closely associated with pathologic activity, such as fibrosis, bronchospasm, and epithelial remodeling, are detailed in subsequent sections.
Mechanism
MBP is toxic to helminths, bacteria, and mammalian cells. MBP can exert cytotoxic effects through several pathways. It is capable of increasing membrane permeability, disrupting a cell’s lipid bilayer.[13][14] MBP also increases histamine release by stimulating mast cells and basophils. Additionally, it can enhance superoxide formation in alveolar macrophages.[14]
MBPs participate in host defense and inflammation via another distinct method: extracellular DNA traps.[15] Eosinophil extracellular traps (EETs) are an innate immune mechanism, and they form from cell-released DNA, which combines with eosinophil granule proteins, including MBP, to form a web that is capable of binding and destroying bacteria.[14][15] The exact role of MBP and other eosinophil granule proteins in EETs is still under active investigation. Of note, extracellular traps also form by neutrophils (where they were first characterized in 2004), basophils, and lymphocytes.
MBP can influence nerve activity, as well. MBP is an allosteric antagonist of inhibitory M2 receptors.[16] The role of eosinophils and MBP in stimulating bronchial hyperreactivity is a well-characterized phenomenon. MBP and other eosinophil granules are responsible for enhancing vagally induced bronchospasm.[16] M2 muscarinic receptors in vagal nerves in the lung inhibit the release of acetylcholine, which is responsible for bronchoconstriction. The blockade of inhibitory M2 receptors by MBP leads to increased release of acetylcholine and bronchial hyperreactivity. Studies have shown that neutralization of MBP with polyanionic substances or with antibodies to MBP is able to prevent M2 receptor dysfunction and bronchospasm.[16]
Pathophysiology
Organ and tissue-specific damage due to eosinophil dysfunction or hyperactivity occurs through a variety of methods. MBP is heavily involved in these processes. Four general mechanisms can describe the pathology seen in eosinophilic disorders[5]:
- Eosinophilic infiltration: Excessive accumulation of eosinophils in tissue can lead to tissue damage if there is extensive deposition. This condition may occur in eosinophilic types of pneumonia, for example.[5][17]
- Allergic inflammation: As previously mentioned, IL-5 is vital for its role in stimulating the differentiation and growth of eosinophils and for stimulating their recruitment to sites of inflammation. Th2 cells are highly associated with allergic conditions and can stimulate eosinophils directly or indirectly. Direct stimulation can occur with the Th2 release of IL-5. Indirect activation can occur with Th2 production of IgE, which can bind mast cells (type I hypersensitivity response). Release of mast cell contents, such as Il-5 and leukotrienes, can lead to further eosinophil activation and inflammation.
- Fibrosis: Eosinophils can cause fibrosis by releasing transforming growth factor β, interleukin 4, and interleukin 13, leading to fibroblast activation and proliferation.[18] Eosinophils can also release granular contents, such as MBP and eosinophil peroxidase (EPO), to stimulate epithelial cells to express fibrosis-inducing factors, a mechanism employed in bronchial epithelial cells that contributes to airway remodeling.[19] Researchers have also identified MBP for its role in promoting muscle fibrosis in muscular dystrophy, endomyocardial fibrosis, eosinophilic esophagitis, and other conditions.[20][21][20]
- Thrombosis: Eosinophil granular contents can induce a hypercoagulable state in certain diseases by activating platelets. MBP and EPO are potent platelet agonists.[9] This action is evident in conditions such as thrombotic microangiopathy of the kidney in association with hypereosinophilic syndrome.[5]
Clinical Significance
Linking clinical symptoms or diseases to eosinophils can, at times, be especially challenging, because eosinophils may not always be present on histopathological or microscopic examination of specimens. This situation can occur due to the degranulation of eosinophil contents at target sites without direct infiltration of eosinophils. As a result, testing for MBP and granular proteins has increased.
Skin: Atopic dermatitis is associated with elevations of serum IgE and eosinophilia in blood. However, biopsies of patients with atopic dermatitis are absent of eosinophils. An analysis of skin tissue via immunofluorescence from affected patients revealed the presence of MBP, suggesting degranulation of MBP from eosinophils in the dermis of patients with atopic dermatitis.[22] These findings further emphasize that eosinophil involvement cannot be excluded simply because of their absence on biopsy, since the release of granule contents, such as MBP, can still occur.
MBP has also been found in skin biopsies of patients with chronic urticaria.[23] Other skin conditions associated with general eosinophilia include eosinophilic cellulitis and bullous pemphigoid.[5]
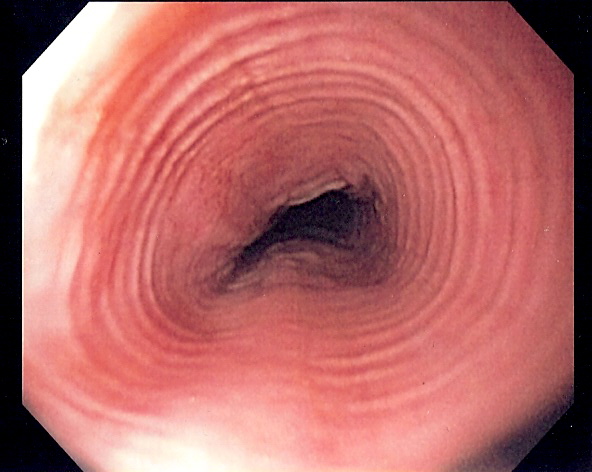
Gastrointestinal: Eosinophilia and MBP have correlated with various gastrointestinal conditions, such as eosinophilic esophagitis, celiac disease, inflammatory bowel disease, and eosinophilic gastroenteritis.[24] In a study of patients with eosinophilic esophagitis, biopsies were taken for histological examination and evaluation for the presence of MBP by staining with indirect immunofluorescence.[25] MBP deposition in eosinophilic esophagitis was found in all studied symptomatic patients and showed a correlation with symptom severity independent of eosinophil counts. Similar to atopic dermatitis, eosinophils likely release their granule contents and lose their morphological identity when specimens are examined.[25]
Upper and lower airways: MBP has implications in bronchial hyperreactivity (reviewed in “mechanisms”). The measurement of this granule in the sputum of patients with asthma has been shown in some studies to be better at identifying asthma than measurement of eosinophilia alone.[26] Upper airway eosinophilic involvement includes conditions such as chronic rhinosinusitis, especially with associated nasal polyposis.[27]
Cardiovascular: MBP is deposited in the cardiac tissue of patients with the eosinophilic endomyocardial disease.[21] Evaluation of cardiac tissue biopsies stained for MBP found eosinophils and MBP in necrotic and thrombotic lesions within the endocardium and blood vessels, demonstrating the involvement of MBP and other granule proteins in triggering cardiac injury in endomyocardial fibrosis.[21] Endomyocardial fibrosis is considered the most common restrictive cardiomyopathy in the world. It is clinically comparable to Loeffler endocarditis, another restrictive cardiomyopathy caused by eosinophil infiltration. Vascular dysfunction has also been associated with eosinophilia and includes disorders such as eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome).
Media
(Click Image to Enlarge)
(Click Image to Enlarge)

Transmission electron microscope image of a thin section cut through an Eosinophil. Eosinophils contain eosinophil granules that are large (0.1-1.0 micron) spherical, membrane-bound structures, containing a dense and lamellated crystalloid core. Contributed from Louisa Howard; http://remf.dartmouth.edu/images/humanBloodCellsTEM/source/1.html (Public Domain)
References
Thomas LL, Kubo H, Loegering DJ, Spillard K, Weaver AJ, McCormick DJ, Weiler C, Gleich GJ. Peptide-based analysis of amino acid sequences important to the biological activity of eosinophil granule major basic protein. Immunology letters. 2001 Oct 1:78(3):175-81 [PubMed PMID: 11578692]
Level 3 (low-level) evidenceOxvig C, Gleich GJ, Sottrup-Jensen L. Localization of disulfide bridges and free sulfhydryl groups in human eosinophil granule major basic protein. FEBS letters. 1994 Mar 21:341(2-3):213-7 [PubMed PMID: 8137941]
Level 3 (low-level) evidenceBarker RL, Gleich GJ, Pease LR. Acidic precursor revealed in human eosinophil granule major basic protein cDNA. The Journal of experimental medicine. 1988 Oct 1:168(4):1493-8 [PubMed PMID: 3171483]
Popken-Harris P, McGrogan M, Loegering DA, Checkel JL, Kubo H, Thomas LL, Moy JN, Sottrup-Jensen L, Snable JL, Kikuchi MT. Expression, purification, and characterization of the recombinant proform of eosinophil granule major basic protein. Journal of immunology (Baltimore, Md. : 1950). 1995 Aug 1:155(3):1472-80 [PubMed PMID: 7543523]
Level 3 (low-level) evidenceAkuthota P, Weller PF. Spectrum of Eosinophilic End-Organ Manifestations. Immunology and allergy clinics of North America. 2015 Aug:35(3):403-11. doi: 10.1016/j.iac.2015.04.002. Epub 2015 Jun 17 [PubMed PMID: 26209892]
Wassom DL, Gleich GJ. Damage to Trichinella spiralis newborn larvae by eosinophil major basic protein. The American journal of tropical medicine and hygiene. 1979 Sep:28(5):860-3 [PubMed PMID: 484767]
Level 3 (low-level) evidenceOgasawara H, Furuno M, Edamura K, Noguchi M. Peptides of major basic protein and eosinophil cationic protein activate human mast cells. Biochemistry and biophysics reports. 2020 Mar:21():100719. doi: 10.1016/j.bbrep.2019.100719. Epub 2019 Dec 25 [PubMed PMID: 32072023]
Weiler JM, Edens RE, Bell CS, Gleich GJ. Eosinophil granule cationic proteins regulate the classical pathway of complement. Immunology. 1995 Feb:84(2):213-9 [PubMed PMID: 7750997]
Rohrbach MS, Wheatley CL, Slifman NR, Gleich GJ. Activation of platelets by eosinophil granule proteins. The Journal of experimental medicine. 1990 Oct 1:172(4):1271-4 [PubMed PMID: 2212954]
Lehrer RI, Szklarek D, Barton A, Ganz T, Hamann KJ, Gleich GJ. Antibacterial properties of eosinophil major basic protein and eosinophil cationic protein. Journal of immunology (Baltimore, Md. : 1950). 1989 Jun 15:142(12):4428-34 [PubMed PMID: 2656865]
Temkin V, Aingorn H, Puxeddu I, Goldshmidt O, Zcharia E, Gleich GJ, Vlodavsky I, Levi-Schaffer F. Eosinophil major basic protein: first identified natural heparanase-inhibiting protein. The Journal of allergy and clinical immunology. 2004 Apr:113(4):703-9 [PubMed PMID: 15100677]
Level 3 (low-level) evidenceMeirovitz A, Goldberg R, Binder A, Rubinstein AM, Hermano E, Elkin M. Heparanase in inflammation and inflammation-associated cancer. The FEBS journal. 2013 May:280(10):2307-19. doi: 10.1111/febs.12184. Epub 2013 Mar 4 [PubMed PMID: 23398975]
Level 3 (low-level) evidenceKleine TJ, Gleich GJ, Lewis SA. Eosinophil major basic protein increases membrane permeability in mammalian urinary bladder epithelium. The American journal of physiology. 1998 Jul:275(1):C93-C103. doi: 10.1152/ajpcell.1998.275.1.C93. Epub [PubMed PMID: 9688839]
Level 3 (low-level) evidenceAcharya KR, Ackerman SJ. Eosinophil granule proteins: form and function. The Journal of biological chemistry. 2014 Jun 20:289(25):17406-15. doi: 10.1074/jbc.R113.546218. Epub 2014 May 6 [PubMed PMID: 24802755]
Level 3 (low-level) evidenceSimon D, Simon HU, Yousefi S. Extracellular DNA traps in allergic, infectious, and autoimmune diseases. Allergy. 2013 Apr:68(4):409-16. doi: 10.1111/all.12111. Epub 2013 Feb 15 [PubMed PMID: 23409745]
Level 3 (low-level) evidenceJacoby DB, Gleich GJ, Fryer AD. Human eosinophil major basic protein is an endogenous allosteric antagonist at the inhibitory muscarinic M2 receptor. The Journal of clinical investigation. 1993 Apr:91(4):1314-8 [PubMed PMID: 8473484]
Level 3 (low-level) evidenceCarrington CB, Addington WW, Goff AM, Madoff IM, Marks A, Schwaber JR, Gaensler EA. Chronic eosinophilic pneumonia. The New England journal of medicine. 1969 Apr 10:280(15):787-98 [PubMed PMID: 5773637]
Ramirez GA, Yacoub MR, Ripa M, Mannina D, Cariddi A, Saporiti N, Ciceri F, Castagna A, Colombo G, Dagna L. Eosinophils from Physiology to Disease: A Comprehensive Review. BioMed research international. 2018:2018():9095275. doi: 10.1155/2018/9095275. Epub 2018 Jan 28 [PubMed PMID: 29619379]
Pégorier S, Wagner LA, Gleich GJ, Pretolani M. Eosinophil-derived cationic proteins activate the synthesis of remodeling factors by airway epithelial cells. Journal of immunology (Baltimore, Md. : 1950). 2006 Oct 1:177(7):4861-9 [PubMed PMID: 16982928]
Wehling-Henricks M, Sokolow S, Lee JJ, Myung KH, Villalta SA, Tidball JG. Major basic protein-1 promotes fibrosis of dystrophic muscle and attenuates the cellular immune response in muscular dystrophy. Human molecular genetics. 2008 Aug 1:17(15):2280-92. doi: 10.1093/hmg/ddn129. Epub 2008 Apr 21 [PubMed PMID: 18430716]
Level 3 (low-level) evidenceTai PC, Ackerman SJ, Spry CJ, Dunnette S, Olsen EG, Gleich GJ. Deposits of eosinophil granule proteins in cardiac tissues of patients with eosinophilic endomyocardial disease. Lancet (London, England). 1987 Mar 21:1(8534):643-7 [PubMed PMID: 2882081]
Leiferman KM, Ackerman SJ, Sampson HA, Haugen HS, Venencie PY, Gleich GJ. Dermal deposition of eosinophil-granule major basic protein in atopic dermatitis. Comparison with onchocerciasis. The New England journal of medicine. 1985 Aug 1:313(5):282-5 [PubMed PMID: 3892296]
Peters MS, Schroeter AL, Kephart GM, Gleich GJ. Localization of eosinophil granule major basic protein in chronic urticaria. The Journal of investigative dermatology. 1983 Jul:81(1):39-43 [PubMed PMID: 6345685]
Talley NJ, Kephart GM, McGovern TW, Carpenter HA, Gleich GJ. Deposition of eosinophil granule major basic protein in eosinophilic gastroenteritis and celiac disease. Gastroenterology. 1992 Jul:103(1):137-45 [PubMed PMID: 1612323]
Peterson KA, Gleich GJ, Limaye NS, Crispin H, Robson J, Fang J, Saffari H, Clayton F, Leiferman KM. Eosinophil granule major basic protein 1 deposition in eosinophilic esophagitis correlates with symptoms independent of eosinophil counts. Diseases of the esophagus : official journal of the International Society for Diseases of the Esophagus. 2019 Dec 30:32(11):. pii: doz055. doi: 10.1093/dote/doz055. Epub [PubMed PMID: 31310661]
Kim CK, Callaway Z, Kim DW, Kita H. Eosinophil degranulation is more important than eosinophilia in identifying asthma in chronic cough. The Journal of asthma : official journal of the Association for the Care of Asthma. 2011 Dec:48(10):994-1000. doi: 10.3109/02770903.2011.623335. Epub 2011 Oct 24 [PubMed PMID: 22022864]
Van Zele T, Claeys S, Gevaert P, Van Maele G, Holtappels G, Van Cauwenberge P, Bachert C. Differentiation of chronic sinus diseases by measurement of inflammatory mediators. Allergy. 2006 Nov:61(11):1280-9 [PubMed PMID: 17002703]