Introduction
Skin biopsy is an important diagnostic procedure that is commonly performed in dermatology practice.[1] Various methods of skin biopsy exist, and multiple factors are considered in choosing the most appropriate biopsy technique for a given situation.[2] Among the most important factors are location and depth and breadth of sampling. An effort is made to provide the consulting pathologist with as much tissue as clinically reasonable, from a location with the highest chance of diagnostic yield, while causing as little disfigurement and compromise of function to the patient as possible.
Biopsies can be categorized as incisional, in which only a portion of a lesion is sampled, or excisional in which the physician removes all of the visible lesion. An incisional biopsy can be performed as a shave, scissor, curettage, or punch specimen. Excisional biopsy is usually done with a full-thickness scalpel excision or with a deeper oblique (shave or scoop) excision.
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
A biopsy is indicated for diagnosing conditions of the skin and sometimes in systemic diseases that have skin or soft tissue manifestations.
Contraindications
A skin biopsy usually has no contraindications. If there is an allergy to local anesthetics, infection, or tattoo that may lead to challenges, the clinician should take appropriate precautions.
The pre-biopsy evaluation includes a review of bleeding disorders, anticoagulative medication use, and bleeding history. Such factors do not usually preclude skin biopsy.
Equipment
Required equipment includes:
Skin Disinfectant
- Usually alcohol, but other skin disinfectants may be used
Local Anesthetic
- Most commonly xylocaine, 0.5-2 %
- Buffering 1:9 with sodium bicarbonate significantly decreases the pain of injection [3]
Gauze
Biopsy Instrument (usually one of the following)
- Biopsy punch
- #15 scalpel blade
- Flexible hand-held surgical blade or razor blade
- Small scissors for skin tags or other small, protuberant lesions, especially on thin skin
Specimen Fixative
Most often formalin, but specific tests such as direct immunofluorescence and viral or other cultures require other media.[2]
Hemostatic Agent
- Aluminum chloride solution is most commonly used, but other agents such as Monsel's ferric subsulfate solution may be used.
Sterile Ointment and Bandage Material
- Sterile petrolatum is preferred as there is no significant difference in infection vs topical antibiotic, but much less chance of causing an allergic reaction.
- Non-stick surgical dressing and hypoallergenic tape
Preparation
Once the biopsy site has been selected, the area should be wiped with alcohol to decrease bacterial count and also to remove oils from the skin. For red lesions, it is especially important to mark the site prior to injecting anesthetic, as lesions often blanch when injected.
Technique or Treatment
The simplest incisional biopsy technique is the shave technique. A scalpel or a hand-held blade is used to scoop a skin sample of desired thickness. This method is best for superficial processes or for diagnosing non-melanoma skin cancers (NMSC), although NMSC may show more aggressive histologic changes deeper in the skin and may even be missed by very superficial biopsy. The skin is first cleaned and locally anesthetized, and then the skin is stretched with the non-dominant hand while one uses the scalpel or flexible blade to obtain the tissue specimen. Alternatively, the skin may be squeezed while performing a shave biopsy if the deeper tissue is desired and if a more depressed wound is acceptable.
Scissors may be used to obtain incisional biopsies, particularly for small, pedunculated lesions like skin tags or in areas of thin, redundant skin such as the eyelids or axillae. In this method, the base of the lesion is locally anesthetized and cleaned, and then the lesion is snipped at its base while very gently grasping the lesion with forceps. Hemostasis can often be obtained with topical aluminum chloride or with electrocoagulation. It is often useful to paint the pedunculated lesion with aluminum chloride before snipping. In most instances, no additional hemostasis is necessary.
The punch biopsy is another incisional method in which a cylindrical blade is used to obtain a specimen that contains a fuller thickness of the skin. Since it provides greater depth, a punch biopsy is often the best choice for diagnosing inflammatory skin conditions. This method can also be used for the excision of small skin lesions. Disposable punches are sharper and provide better tissue specimens than reusable punches, which are rarely used today. Punch specimens are particularly useful in diagnosing inflammatory dermatoses or in conditions in which the pathology is likely to involve deeper aspects of the skin and subcutaneous tissue. They are also useful in larger pigmented lesions in which excisional biopsy may not be deemed practical. In such cases, one may perform several punch biopsies throughout the larger lesion to get a better sampling. Punches are available in varying diameters, with the most commonly used sizes ranging from 2 mm to 6 mm. The size is chosen to obtain adequate tissue for histologic evaluation while sparing the patient as much disfigurement as possible. Particularly on the face, one may choose a smaller punch. When performing this procedure, it is best to stretch the skin perpendicular to the relaxed skin tension lines with one hand, while the biopsy punch is rotated back and forth with the other hand. When the punch specimen is obtained, and then the skin is released, this results in an elliptical defect. When performing this type of biopsy, the punch is rotated while applying pressure down into the skin. One should be aware of the underlying anatomy and avoid cutting into vital underlying structures with the punch. The punch specimen is gently lifted with forceps or a skin hook, being very careful not to crush the tissue, and the base is severed with fine scissors. The small defect may be closed with simple suturing or allowed to heal secondarily. Some physicians place a bit of cellulose or collagen foam in the biopsy defect to provide an extra measure of hemostasis postoperatively.
Another incisional biopsy technique is the wedge biopsy. This usually involves taking a narrow ellipse of tissue from a larger skin neoplasm. The long axis of the biopsy is generally oriented in a radial fashion and includes a cross-section from the center of the lesion and extends into a portion of normal-appearing skin. If performed with sufficient depth this method can be especially useful in the diagnosis of keratoacanthoma, in which the cross-sectional architecture of the lesion is characteristic. This method can also provide a great deal of information in suspected melanoma when an excisional biopsy is not practical.
Excisional biopsy is preferred in small lesions or in suspected malignant melanoma, when practical.[4][5][6] If melanoma is suspected, it is important to perform a biopsy of adequate depth, as staging and treatment are determined by the thickness of the tumor. If the base is transected, accurate staging can be difficult or impossible. Excisional biopsy is most often performed with the scalpel, taking the full thickness of the skin of the entire visible lesion and may contain some subcutaneous tissue. Excisional biopsy may also be performed with a razor blade or flexible blade made specifically for skin surgery. To be considered an excision, the deep shave must extend into the underlying adipose (fatty) tissue.
Hemostasis may be obtained with chemical styptic agents such as aluminum chloride or Monsel's ferric subsulfate solution in small or superficial biopsy wounds. Alternately, one may use collagen or cellulose sponges to control bleeding, in addition to a pressure bandage. Hemostasis in punch sites can often be obtained with one or a few simple sutures. The absorbable suture material may be used to save the patient a trip back for suture removal. Excisional biopsy sites often require electrocoagulation before the placement of a pressure dressing. If an excisional biopsy site is to be sutured, chemical anticoagulant agents should be avoided. After suturing, the site should be cleaned and sterile petrolatum is applied. A non-stick dressing is applied along with cotton or fluffed gauze to apply pressure, and this pressure dressing is secured with paper or hypoallergenic stretch fabric tape. Tape strips should run perpendicular to the incision line to tension is decreased on sutures.
Finally, it is important to know what to biopsy. In some cases in which a skin eruption has different appearances, it may be necessary to sample a few representative areas. Blistering conditions may call for biopsy of both lesional and perilesional skin and may require different transport media, particularly if direct immunofluorescence, tissue culture, or fungal culture are planned. If in doubt, it is always a good idea to check with the dermatopathologist before the biopsy to be sure that proper equipment and media are present at the time of the biopsy. Also, providing the pathologist with pertinent clinical information increases the likelihood of obtaining information that will be helpful to the patient.
Complications
Complications may include:
- Bleeding at the biopsy site
- Hematoma
- Infection
Pressure dressings and ice may minimize the development of bleeding or hematomas. A suture is often needed for hemostasis, particularly after a punch biopsy greater than 3mm to 4 mm. Uncontaminated procedures have a less than 5% infection rate. Prophylactic antibiotics can be considered if the patient is at high risk.
Rarely do patients experience a hypersensitivity reaction or a vasovagal response. If a vasovagal reaction occurs, place the patient in a Trendelenburg position or place the patient flat and elevate the legs.
Clinical Significance
The patient should be informed the biopsy site will heal with some degree of scarring. A shave biopsy heals over weeks with crusting, eschar, and mild pain and leaves a hypopigmented or hyperpigmented scar.
Skin biopsies are usually used to assist in making or confirming a diagnosis. The intent is to characterize the nature of a skin growth or eruption and assist in the histopathologic evaluation of a tissue sample.
Because of the low risk, a skin biopsy can be safely and routinely performed in an inpatient or outpatient setting.
Enhancing Healthcare Team Outcomes
While the biopsy is technically simple, the choice of biopsy type and site is essential to obtaining a useful sample. Especially if performing a biopsy without an assistant, it is important to have all needed supplies available and open prior to beginning. Also prior to biopsy, it is very helpful to take photographs of good quality. It is also of utmost importance to provide information to the pathologist, including clinical description, location of biopsy, and clinical differential diagnosis.
Media
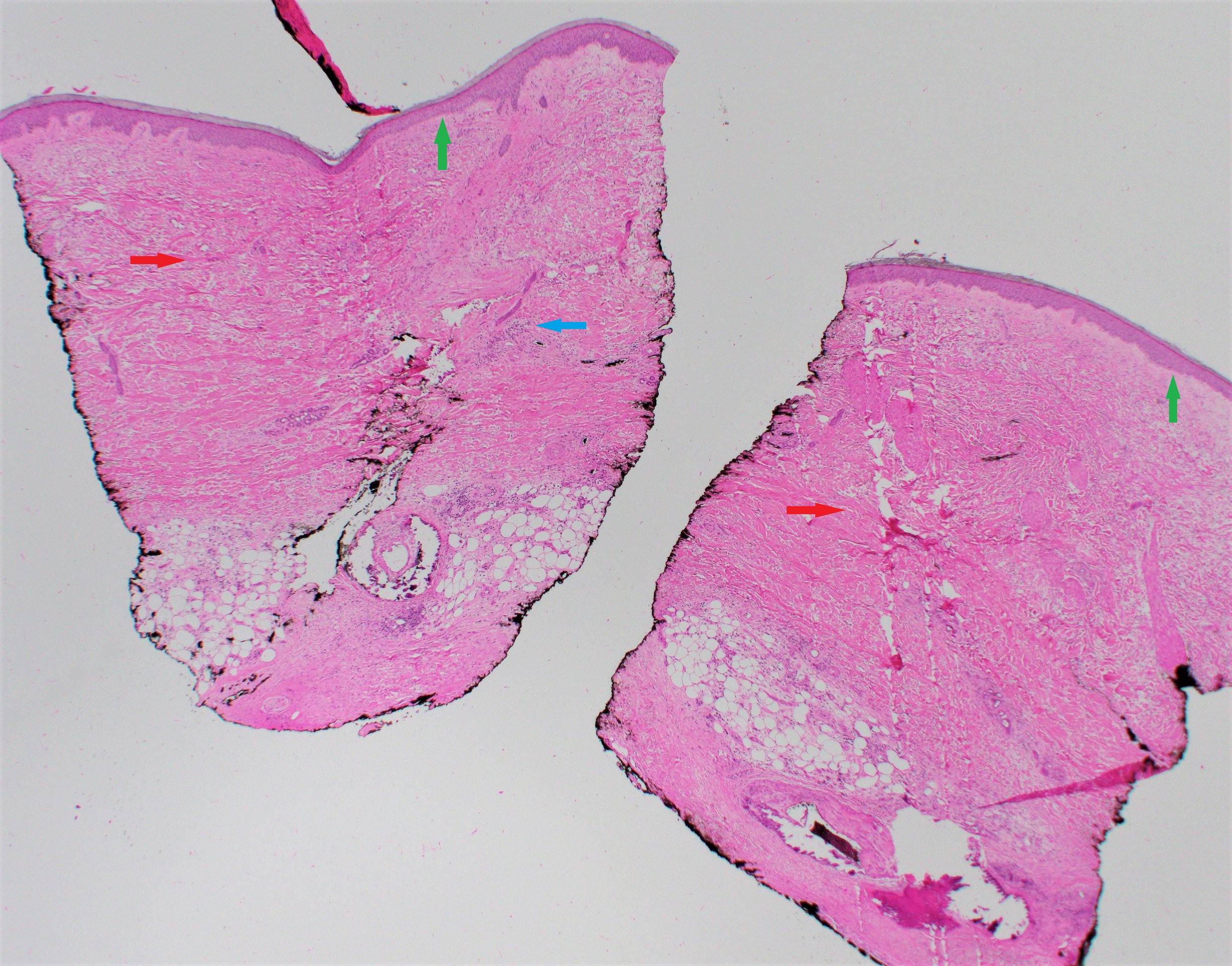
(Click Image to Enlarge)
References
Yang S, Kampp J. Common Dermatologic Procedures. The Medical clinics of North America. 2015 Nov:99(6):1305-21. doi: 10.1016/j.mcna.2015.07.004. Epub 2015 Sep 11 [PubMed PMID: 26476254]
Elston DM, Stratman EJ, Miller SJ. Skin biopsy: Biopsy issues in specific diseases. Journal of the American Academy of Dermatology. 2016 Jan:74(1):1-16; quiz 17-8. doi: 10.1016/j.jaad.2015.06.033. Epub [PubMed PMID: 26702794]
McKay W, Morris R, Mushlin P. Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anesthesia and analgesia. 1987 Jun:66(6):572-4 [PubMed PMID: 3034106]
Miedema J, Zedek DC, Rayala BZ, Bain EE 3rd. 9 tips to help prevent derm biopsy mistakes. The Journal of family practice. 2014 Oct:63(10):559-64 [PubMed PMID: 25343153]
Cheng R, Bialas RW, Chiu ST, Lawrence TJ, Lesesky EB. Punch biopsy vs. shave biopsy: a comparison of margin status of clinically atypical pigmented lesions. The British journal of dermatology. 2015 Sep:173(3):849-51. doi: 10.1111/bjd.13830. Epub 2015 Aug 19 [PubMed PMID: 25864555]
Sharma KS, Lim P, Brotherston MT. Excision versus incision biopsy in the management of malignant melanoma. The Journal of dermatological treatment. 2016:27(1):88-90. doi: 10.3109/09546634.2015.1034083. Epub 2015 Apr 17 [PubMed PMID: 25886086]