Dermatoscopic Characteristics of Melanoma Versus Benign Lesions and Nonmelanoma Cancers
Dermatoscopic Characteristics of Melanoma Versus Benign Lesions and Nonmelanoma Cancers
Introduction
Dermoscopy, also known as dermatoscopy, is a valuable noninvasive handheld tool that enables clinicians to examine skin lesions under microscopic magnification. An additional feature, polarized light, enhances the visualization of deeper skin structures.[1] Studies have demonstrated that this instrument reduces costs by decreasing the number of biopsies compared to evaluations based solely on the naked eye.[2] Dermoscopic characteristics often correlate with histopathologic findings, providing clinicians with deeper insights into the nature of the lesions being examined.[3]
While a naked eye examination can be useful, it has been observed that up to 40% of melanomas may be misclassified when clinicians rely solely on the ABCDE rule.[4] The ABCDE rule includes asymmetry, border irregularity, color variegation, diameter greater than 6 mm, and evolution.[5]
Dermoscopy not only aids in diagnosing melanomas but is also valuable in identifying nonmelanoma skin cancers. Studies have shown that dermoscopy can help differentiate among various subtypes of basal cell carcinomas.[6] This is significant as the various histological subtypes of basal cell carcinomas require distinct treatment approaches.[6]
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
A dermoscope is a handheld device that magnifies skin structures and provides visualization through the skin's surface, allowing clinicians to view the epidermis and superficial dermis.[5][7][8] Biopsy ratios have decreased from 1:18 to 1:4 by using this tool.[5] Studies have demonstrated the economic benefits of dermoscopy, showing that it increases the sensitivity of diagnosing malignant lesions by 91%.[9] While some may argue that aggressive biopsying, despite its low sensitivity, can be justified to detect melanoma, patient concerns must be considered. Patients often have concerns about scarring, fear of undergoing a biopsy, and the risk of infection.[4] Developing proficiency in dermoscopy can increase confidence in making informed decisions about when a biopsy is necessary
Issues of Concern
While dermoscopy is highly beneficial during a patient’s skin examination, becoming proficient with the tool requires overcoming a learning curve.[4] Dermoscopy should be considered an invaluable adjunct to the naked eye examination and relevant clinical information, such as recent changes in lesion morphology.[10] Comprehensive and consistent training is essential to develop proficiency, as initial use may actually increase benign lesion biopsy rates.[4] Clinicians risk false confidence without adequate training, potentially leading to missed necessary biopsies.[11]
Clinical Significance
Dermoscopy holds significant clinical value in differentiating benign from malignant lesions, improving diagnostic accuracy and patient care. This noninvasive tool provides a detailed examination of skin lesions, leading to more informed and precise clinical decisions.
Benign Versus Malignant Lesions
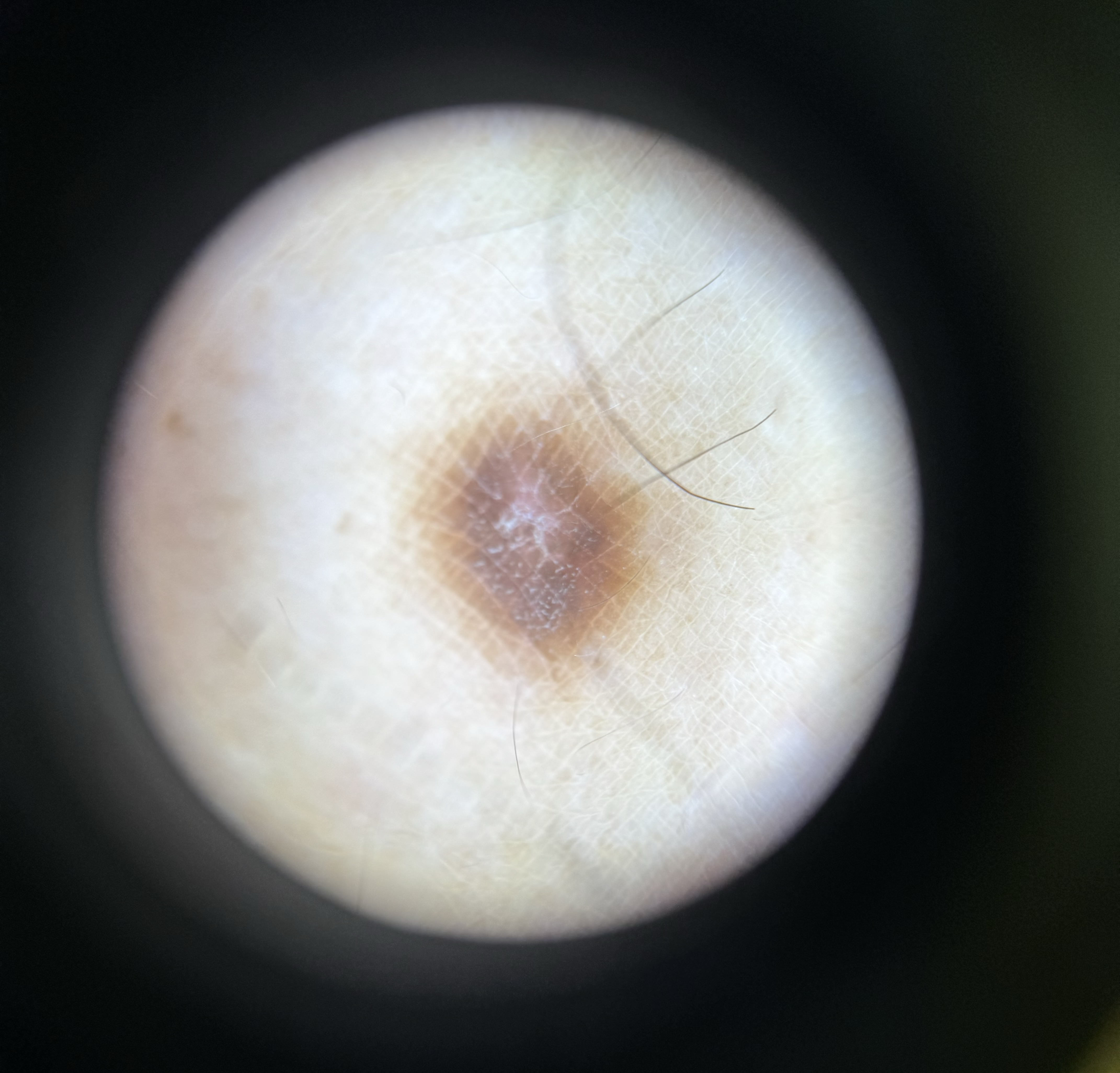
To accurately differentiate between benign and malignant lesions, it is essential to understand the characteristics of benign lesions. Certain nevi exhibit distinct dermoscopic findings. For instance, Spitz nevus typically displays a "starburst" pattern, which can help distinguish it from melanoma.[12] Benign nevi generally feature a regular pigment network and uniformly shaped globules throughout the lesion (see Image. Dermoscopic Image of a Benign Nevus).[13] Blue nevi, on the other hand, often have a homogeneous blue steel color throughout the lesion.[5]
A pigment network is a reticular pattern of brown lines commonly seen in nevi and dermatofibromas.[13] Dermatofibromas Dermatofibromas typically also feature a central white patch (see Image. Dermoscopic Image of a Dermatofibroma).[13] Atypical nevi often exhibit monomorphic vessels and multiple colors, typically black, light brown, and dark brown.[10] In contrast, melanoma will show more prominent skin markings and irregular hyperpigmentation, distinguishing it from atypical nevi.[14]
Melanoma
Dermoscopy is crucial for the early diagnosis of melanoma, as it can reveal malignant features that might otherwise appear benign during a naked eye examination.[14] Key dermoscopic characteristics of melanoma include a homogeneous blue pattern, irregular globules, pseudopods at the periphery, a negative and irregular pigment network, and angulated lines.[13] These characteristics are noted to have a high odds ratio for diagnosing melanoma.[4] A homogeneous blue pattern may correlate histologically with pagetoid spread and an increased number of melanocytes.[5] Irregular globules represent nests of melanocytes observed in histology, while pseudopods can indicate melanocyte nests at the dermal-epidermal junction.[5]
A negative pigment network is described as winding hypopigmented lines encircling elongated globules, a finding particularly associated with melanomas arising from nevi.[13][5] Histologically, this may correlate with the bridging of rete ridges.[5] An irregular pigment network is histologically observed as disorganized rete ridges.[5] Angulated lines on histology correspond to flattened dermoepidermal junctions, pagetoid spread, and the confluence of atypical melanocytes.[5]
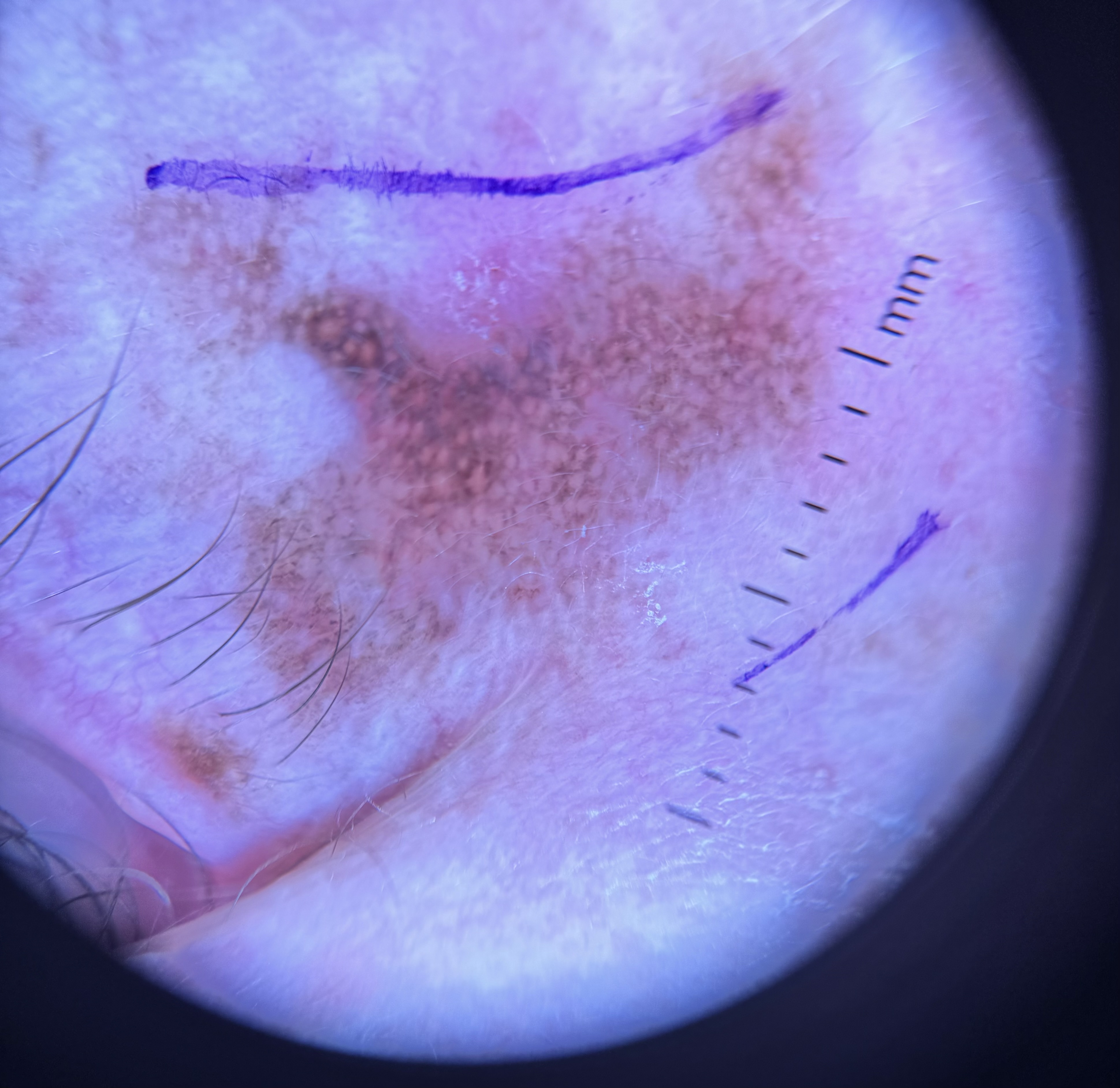
Subtypes of melanoma: Melanoma has several subtypes, each with specific dermoscopic characteristics that aid in diagnosis. Melanoma in situ typically presents with significant pigment regression, an atypical network, angulated lines, irregular hyperpigmentation, and prominent skin markings (see Image. Dermoscopic Image of Malignant Melanoma In Situ).[14] Lentigo maligna is one of the most challenging subtypes of melanoma to diagnose, even with dermoscopy, due to its characteristics that often resemble benign lesions.[3] Characteristics of lentigo maligna include rhomboid structure, gray globules and dots, and asymmetric pigmented follicular openings.[3] The presence of gray globules, dots, and angulated lines is highly sensitive for diagnosing lentigo maligna.[14]
In superficial spreading melanoma, the presence of an irregular network typically indicates melanoma in situ within the lesion.[5] Not only can specific subtypes of melanoma be assessed with dermoscopy, but an increasing number of studies suggest that it may also be possible to evaluate Breslow thickness using this technique.[15] A study demonstrates that increased Breslow thickness correlates with the presence of white shiny structures, a blue-gray veil, and milky red areas.[16]
Special Site Lesions
Special site lesions exhibit specific dermoscopic characteristics that help differentiate between benign and malignant lesions, especially melanoma. In acral lesions, increased pigmentation in the ridges is a strong indicator of melanoma, with a reported specificity as high as 99%. Additionally, a checklist can be used to thoroughly evaluate acral lesions. The BRAAFF checklist stands for the characteristics of irregular blotch, parallel ridges, asymmetry of structures, asymmetry of colors, parallel furrow pattern, and fibrillar pattern. Each feature is scored as irregular blotch and asymmetry of structures and colors; each adds 1 point if present, and parallel ridges add 3 points if present. Conversely, the presence of parallel furrow and fibrillar patterns each deducts 1 point if present in the lesion. A total score of 1 or more points on the BRAAFF checklist indicates a higher likelihood of melanoma.[14]
Nonpigmented Cancerous Lesions
Dermoscopy is also valuable for assessing nonpigmented cancerous lesions. Basal and squamous cell carcinomas are the 2 most common types of skin cancers. However, the dermoscopic characteristics of nonmelanoma skin cancers are generally less specific compared to properly diagnosed melanomas. A study comparing dermoscopy to naked eye examinations found that the proportion of correct diagnoses increased from 41.3% to 52.7% when using dermoscopy.[14]
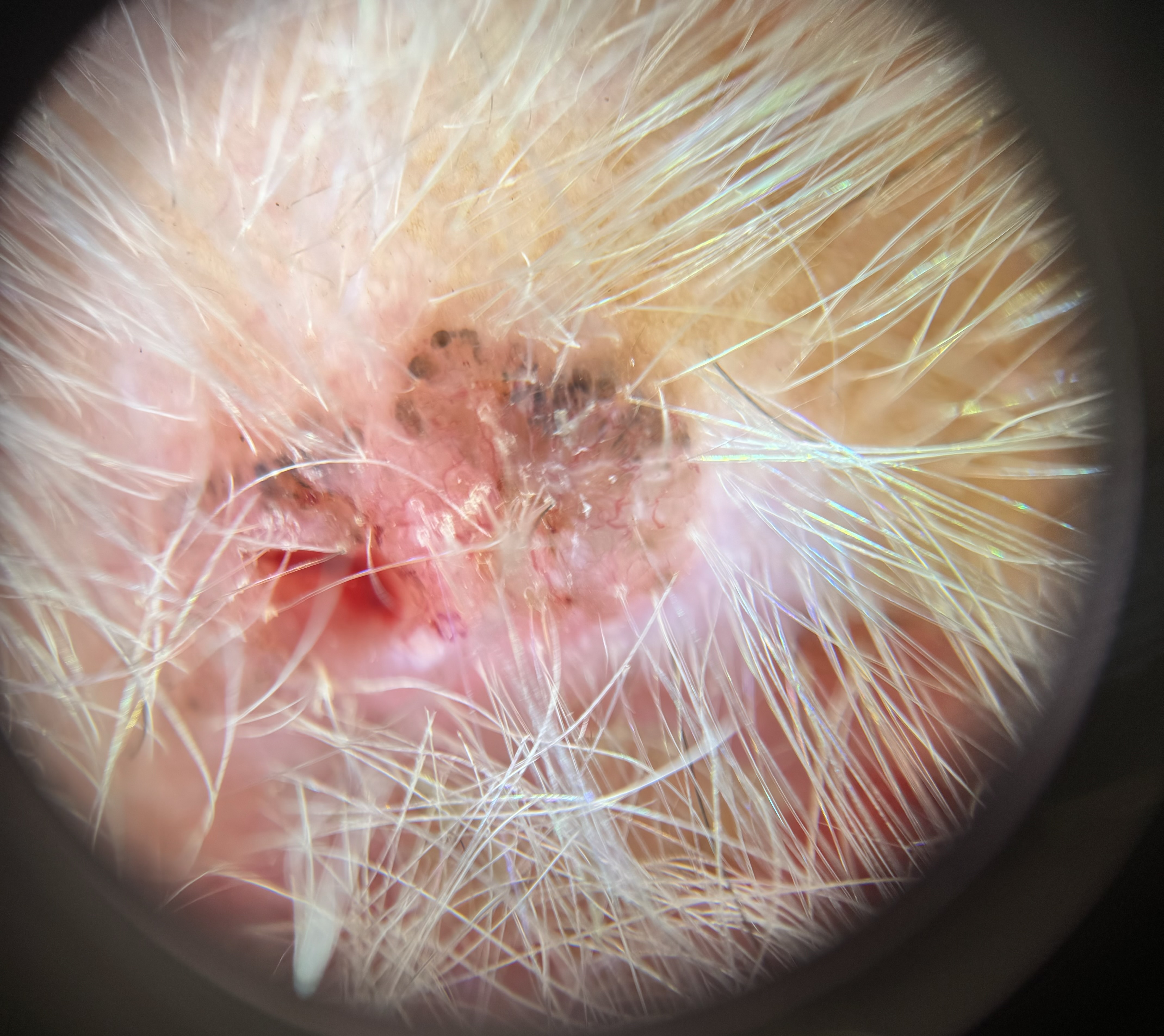
Basal cell carcinoma: Dermoscopy reveals several key characteristics of basal cell carcinoma, including arborizing vessels, a maple leaf-like structure, ulceration, blue-gray globules, blue ovoid nests, and spoke wheel areas.[14] Although some features may overlap with other neoplastic lesions, the appearance of shiny white blotches and strands, particularly visible under polarized light, are more distinctive of basal cell carcinoma than other neoplasms (see Image. Dermoscopic Image of a Basal Cell Carcinoma).
Notably, superficial basal cell carcinoma typically lacks arborizing vessels and blue ovoid nests and is more likely to exhibit multiple small erosions, especially in lighter Fitzpatrick skin types. In contrast, nodular basal cell carcinoma usually exhibits arborizing vessels, blue ovoid nests, and ulceration.[4] Pigmented basal cell carcinomas are more likely to show blue ovoid nests, blue globules, and arborizing vessels.[14]
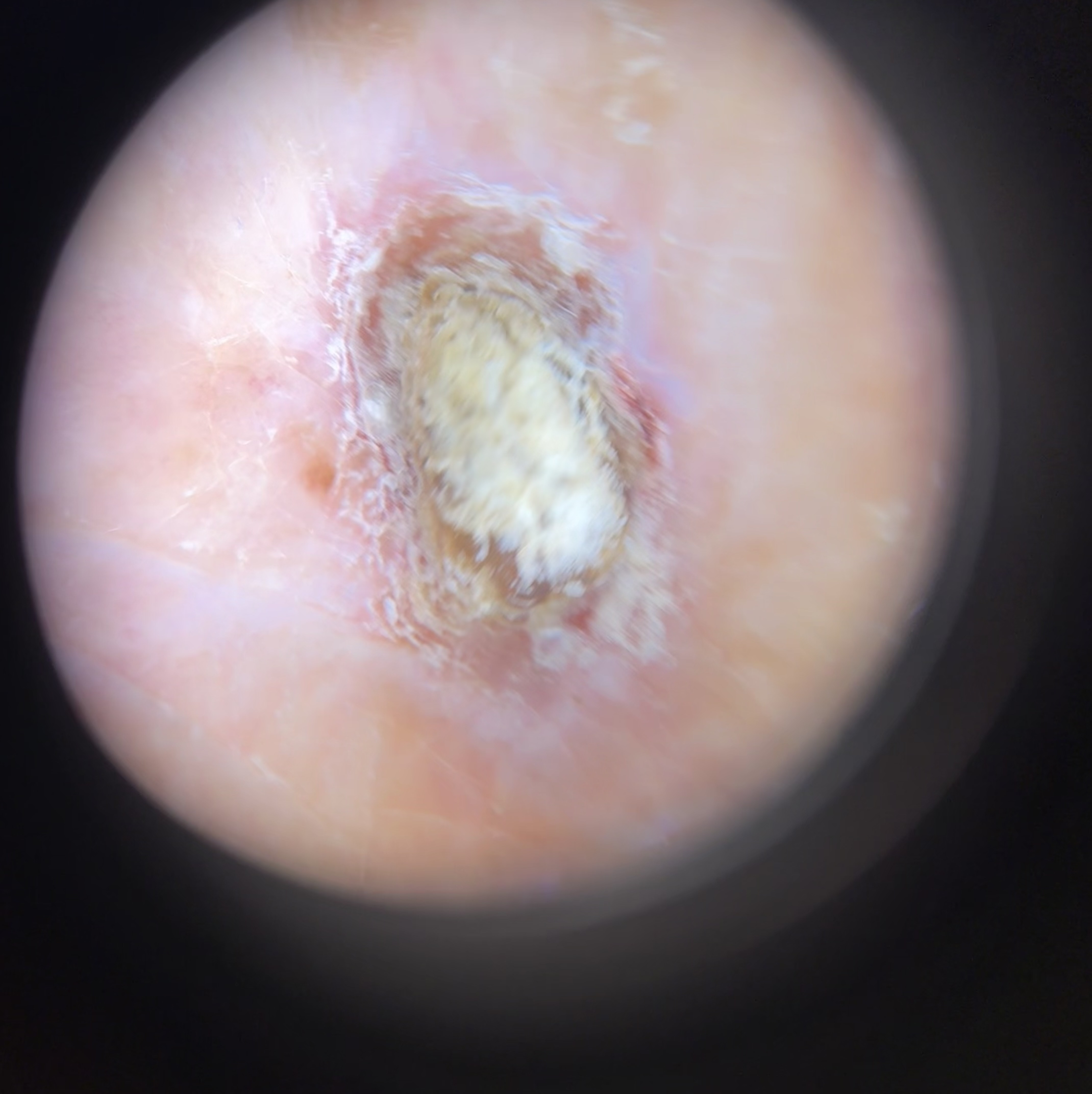
Squamous cell carcinoma: Dermoscopy reveals distinct characteristics of squamous cell carcinoma, including coiled vessels, blood spots, structureless areas, and white circles (see Image. Dermoscopic Image of a Squamous Cell Carcinoma). Well-differentiated squamous cell carcinoma typically shows blood spots, white circles, and structureless areas, which help differentiate it from actinic keratosis. In contrast, poorly differentiated squamous cell carcinoma may present with ulceration, bleeding, and a lack of scaling. Keratoacanthoma is usually characterized by a keratin plug in the center of the lesion.[14]
Other Issues
As dermoscopy is not a standalone or perfect tool, healthcare professionals must utilize the patient's clinical history in addition to the dermoscopic findings to make an accurate diagnosis. With proper training, dermoscopy can help reduce healthcare costs and increase the rate of skin cancer detection. Dermoscopy is a valuable tool for clinicians performing skin examinations, but its benefits are fully realized only when the clinician is adequately trained. Mastering dermoscopy requires practice, but the rewards are invaluable once proficiency is achieved.
Enhancing Healthcare Team Outcomes
Dermoscopy is an invaluable tool for clinicians performing thorough skin examinations. Enhancing patient-centered care, outcomes, safety, and team performance related to dermoscopy requires an interprofessional approach involving physicians, advanced practitioners, nurses, pharmacists, and other healthcare professionals.
Physicians must master dermoscopic techniques to accurately distinguish between benign and malignant lesions, guiding diagnostic decisions and treatment planning. Proper training is essential for correctly identifying the characteristics of various skin lesions under dermoscopy. Dermoscopy significantly increases specificity in differentiating benign pigmented lesions from melanoma. Although the benefits of diagnosing nonmelanoma skin cancers are slightly lower, these lesions still exhibit distinguishing dermoscopic features that aid their diagnosis.
Advanced practitioners and nurses must develop proficiency in recognizing dermoscopic patterns and assisting with the examination process. They are also crucial in patient education and support during follow-up care. Pharmacists are essential in understanding dermoscopic procedures and offering relevant medication advice, particularly for post-biopsy care and treatment.
An interprofessional approach is crucial for implementing evidence-based protocols for dermoscopic examinations, ensuring standardized care, and developing clear follow-up strategies for patients with identified lesions to guarantee timely management and intervention. Using checklists such as the BRAAFF algorithm for acral melanoma can significantly improve diagnostic accuracy when distinguishing malignant from benign lesions.[17][18]
Interprofessional healthcare teams can enhance the efficacy of dermoscopy in clinical practice through coordinated care efforts. This includes efficiently referring patients to oncologists when advanced care is necessary and educating patients about their skin health, the importance of follow-ups, and preventive measures.
Studies demonstrate that dermoscopy can be cost-effective by reducing unnecessary biopsies, lowering healthcare costs, and decreasing patient anxiety associated with unnecessary procedures. Fewer biopsies also result in fewer scars, thereby improving patient satisfaction. Encouraging physicians to use dermoscopy benefits both patients and the healthcare system. Strategizing dermoscopy use ensures diagnostic accuracy and optimizes patient outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Vestergaard ME, Macaskill P, Holt PE, Menzies SW. Dermoscopy compared with naked eye examination for the diagnosis of primary melanoma: a meta-analysis of studies performed in a clinical setting. The British journal of dermatology. 2008 Sep:159(3):669-76. doi: 10.1111/j.1365-2133.2008.08713.x. Epub 2008 Jul 4 [PubMed PMID: 18616769]
Level 1 (high-level) evidenceMassone C, Di Stefani A, Soyer HP. Dermoscopy for skin cancer detection. Current opinion in oncology. 2005 Mar:17(2):147-53 [PubMed PMID: 15725920]
Level 3 (low-level) evidenceRusso T, Piccolo V, Lallas A, Argenziano G. Recent advances in dermoscopy. F1000Research. 2016:5():. pii: F1000 Faculty Rev-184. doi: 10.12688/f1000research.7597.1. Epub 2016 Feb 17 [PubMed PMID: 26949523]
Level 3 (low-level) evidenceYélamos O, Braun RP, Liopyris K, Wolner ZJ, Kerl K, Gerami P, Marghoob AA. Usefulness of dermoscopy to improve the clinical and histopathologic diagnosis of skin cancers. Journal of the American Academy of Dermatology. 2019 Feb:80(2):365-377. doi: 10.1016/j.jaad.2018.07.072. Epub 2018 Oct 13 [PubMed PMID: 30321580]
Marghoob NG, Liopyris K, Jaimes N. Dermoscopy: A Review of the Structures That Facilitate Melanoma Detection. The Journal of the American Osteopathic Association. 2019 Jun 1:119(6):380-390. doi: 10.7556/jaoa.2019.067. Epub [PubMed PMID: 31135866]
Álvarez-Salafranca M, Ara M, Zaballos P. Dermoscopy in Basal Cell Carcinoma: An Updated Review. Actas dermo-sifiliograficas. 2021 Apr:112(4):330-338. doi: 10.1016/j.ad.2020.11.011. Epub 2020 Nov 28 [PubMed PMID: 33259816]
Ayhan E, Ucmak D, Akkurt Z. Vascular structures in dermoscopy. Anais brasileiros de dermatologia. 2015 Jul-Aug:90(4):545-53. doi: 10.1590/abd1806-4841.20153452. Epub [PubMed PMID: 26375224]
Gerard A, Derom F, Vossaert R, Huyghe JP, Lantin F, Vereecken LF, De Graef J. [Treatment of resectable cancer of the stomach]. Acta chirurgica Belgica. 1984 Mar-Apr:84(2):76-8 [PubMed PMID: 6375224]
Shir-Az O, Yaacobi DS, Berl A, Yosefof E, Grush AE, Shalom A. Diagnostic Accuracy and Cost Savings Associated with Dermoscopy: An Economic Study. Seminars in plastic surgery. 2022 May:36(2):101-106. doi: 10.1055/s-0042-1749152. Epub 2022 Jun 13 [PubMed PMID: 35937434]
Jitian Mihulecea CR, Frățilă S, Rotaru M. Clinical-dermoscopic similarities between atypical nevi and early stage melanoma. Experimental and therapeutic medicine. 2021 Aug:22(2):854. doi: 10.3892/etm.2021.10286. Epub 2021 Jun 9 [PubMed PMID: 34178127]
Jones OT, Jurascheck LC, van Melle MA, Hickman S, Burrows NP, Hall PN, Emery J, Walter FM. Dermoscopy for melanoma detection and triage in primary care: a systematic review. BMJ open. 2019 Aug 20:9(8):e027529. doi: 10.1136/bmjopen-2018-027529. Epub 2019 Aug 20 [PubMed PMID: 31434767]
Level 1 (high-level) evidencePogorzelska-Antkowiak A, Slowinska M, Farinazzo E, Conforti C, Agozzino M. Spitz nevus and melanoma: evaluation with dermoscopy and reflectance confocal microscopy. Postepy dermatologii i alergologii. 2023 Jun:40(3):427-431. doi: 10.5114/ada.2023.125968. Epub 2023 Mar 21 [PubMed PMID: 37545824]
Yélamos O, Braun RP, Liopyris K, Wolner ZJ, Kerl K, Gerami P, Marghoob AA. Dermoscopy and dermatopathology correlates of cutaneous neoplasms. Journal of the American Academy of Dermatology. 2019 Feb:80(2):341-363. doi: 10.1016/j.jaad.2018.07.073. Epub 2018 Oct 13 [PubMed PMID: 30321581]
Weber P, Tschandl P, Sinz C, Kittler H. Dermatoscopy of Neoplastic Skin Lesions: Recent Advances, Updates, and Revisions. Current treatment options in oncology. 2018 Sep 20:19(11):56. doi: 10.1007/s11864-018-0573-6. Epub 2018 Sep 20 [PubMed PMID: 30238167]
Level 3 (low-level) evidenceJitian Mihulecea CR, Iancu GM, Leventer M, Rotaru M. The Many Roles of Dermoscopy in Melanoma Detection. Life (Basel, Switzerland). 2023 Feb 9:13(2):. doi: 10.3390/life13020477. Epub 2023 Feb 9 [PubMed PMID: 36836834]
Martínez-Piva MM, Vacas AS, Rodríguez Kowalczuk MV, Gallo F, Rodrígues Vasconcelos M, Mazzuoccolo LD. Dermoscopy as a Tool for Estimating Breslow Thickness in Melanoma. Actas dermo-sifiliograficas. 2021 May:112(5):434-440. doi: 10.1016/j.ad.2020.11.015. Epub 2020 Nov 28 [PubMed PMID: 33259813]
Lallas A, Kyrgidis A, Koga H, Moscarella E, Tschandl P, Apalla Z, Di Stefani A, Ioannides D, Kittler H, Kobayashi K, Lazaridou E, Longo C, Phan A, Saida T, Tanaka M, Thomas L, Zalaudek I, Argenziano G. The BRAAFF checklist: a new dermoscopic algorithm for diagnosing acral melanoma. The British journal of dermatology. 2015 Oct:173(4):1041-9. doi: 10.1111/bjd.14045. Epub 2015 Oct 1 [PubMed PMID: 26211689]
Ingrassia JP, Stein JA, Levine A, Liebman TN. Diagnosis and Management of Acral Pigmented Lesions. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2023 Oct 1:49(10):926-931. doi: 10.1097/DSS.0000000000003891. Epub 2023 Aug 8 [PubMed PMID: 37556446]