Anatomy, Bony Pelvis and Lower Limb: Pelvis Bones
Anatomy, Bony Pelvis and Lower Limb: Pelvis Bones
Introduction
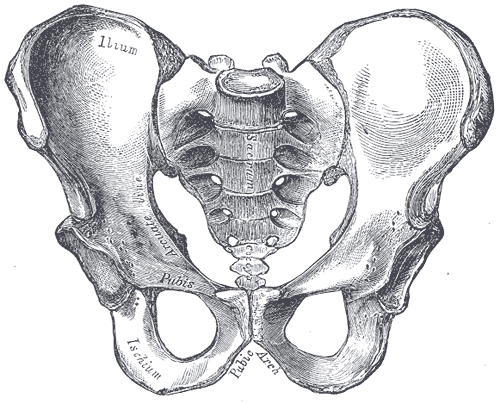
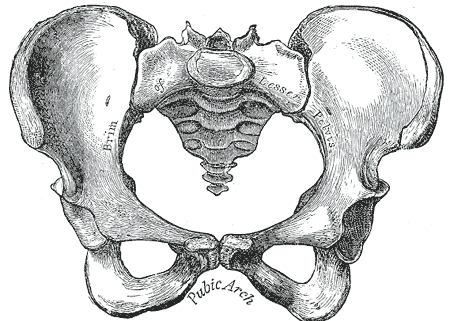
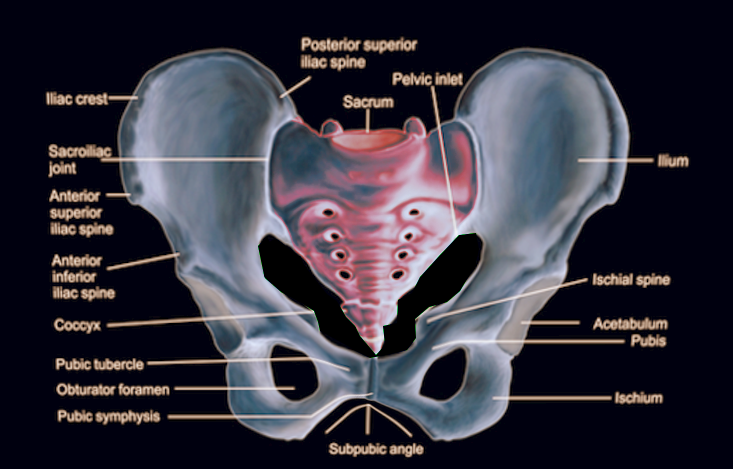
The pelvis consists of the right and left hip bones, each formed by the union of the pubis, ischium, and ilium bones, together with the midline sacrum and coccyx. Anteriorly, the hip bones meet to form the pubic symphysis. Posteriorly, the hip bones unite with the sacrum to form the sacroiliac joints. Together, this structure forms a basin-shaped ring called the bony pelvis or pelvic girdle that connects the axial and the appendicular skeleton.[1]
The bony pelvis is key to many functions of the body, as a transitional zone for neurovascular structures traversing between the abdomen and the lower limbs, a junctional point between the spine and lower limb forces during locomotion, and a structure within which lie crucial visceral structures such as the female reproductive organs, urinary bladder, and rectum.[2]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Each hip bone consists of three bones: the ischium, ilium, and pubis. Together, these bones form the hip or innominate bone; they articulate in the midline with the sacrum posteriorly and anteriorly at the interface between the two pubic bones. The pelvic brim is the line formed by the continuation of the pectineal line on the pubic bones, the arcuate line of the ilium, and the ala of the sacrum. Below this brim is defined as the ‘true pelvis,’ whereas the ‘false pelvis’ above this line is, in fact, part of the abdominal cavity.[3]
The Ilium
The ilium is the physically largest of the three pelvic bones. This structure is located superiorly relative to the pubis and ischium and is composed of a wing-shaped portion called the superior ala along with the inferior body. The rim of the superior ala is called the iliac crest. Anteriorly this crest ends at the anterior superior iliac spine and posteriorly at the posterior superior iliac spine.[4] Inferior to these lie their inferior equivalents. Medially, the iliac fossa is concave and very thin at its deepest part, containing a large bursa for the overlying iliacus muscle. The posterior part of the medial surface contains the auricular surface for articulation with the sacrum. The arcuate line runs obliquely forwards from this, defining part of the pelvic brim.
The Ischium
The ischium is the inferior posterior portion of the hip bone; it consists of a superior body and an inferior ramus. At the posteromedial junction, the bone has a projection called the ischial spine—the concavity between this spine and the posterior inferior iliac spine forms the greater sciatic notch. The concavity between this spine and the inferior ramus is called the lesser sciatic notch. The ischial tuberosity lies at the posterior and inferior surface of the ischium and is divided into a medial part which serves as an attachment for the biceps, semitendinosus, and semimembranosus muscles, and a lateral part to which the sacrotuberous ligament is attached.[5]
The Pubis
The pubis is the inferior, anterior portion of the hip bone consisting of a superior ramus, body, and inferior ramus. The superior ramus helps form the acetabulum and is ridged by an upper pectineal line and lower obturator crest. The inferior ramus of the pubis fuses with the inferior ramus of the ischium. The pubis and ischium together form the obturator foramen, through which pass important neurovascular structures. The body of both the left and right pubis join to form the pubic symphysis joint in the midline, each covered with a layer of hyaline cartilage and intervened by a fibrocartilage disc.[6]
The articular facet for the head of the femur, the acetabulum, is a hemispherical concavity lined by hyaline cartilage. This structure is formed by contributions from the pubis, ilium, and ischium.
The Sacrum and Coccyx
The sacrum forms from the fusion of the five sacral vertebral bodies, which become progressively smaller as they transition from superior to inferior. The sacrum is roughly triangular in shape, gently concave, and pierced by four bilateral sacral foramina to allow passage of the regional nerve roots.[7] The superior-most sacral body, S1, is by far the largest, and its body projects anteriorly as the sacral promontory and is flanked on either side by the lateral alae. Each sacral ala is traversed anteriorly by the sympathetic trunk, lumbosacral trunk, and obturator nerve.
Lateral to the foramina, the area is termed the lateral mass and is the origin of various muscles. On the lateral aspect of the sacrum is an articular surface on each side where it forms the joints with the iliac bone, described later. On the dorsal aspect of the sacrum, there are three vertical bony ridges: the midline median sacral crest, the intermediate sacral crests just medial to the sacral foramina, and the lateral sacral crest. The articular facets for the synovial joint with the L5 vertebra are superiorly on the dorsal aspect of the sacrum.[8]
The sacral cornu is the rounded termination of the intermediate sacral crest at the inferior dorsal aspect on each side. An axial cross-section of the sacrum reveals the triangular sacral canal, through which travels the filum terminale and meninges, as well as a vertebral venous plexus and fatty tissue.[9]
The coccyx is a triangular bone formed by the fusion of four small pieces, and it articulates with the inferior-most part of the sacrum at the sacrococcygeal joint. This joint is reinforced anteriorly and posteriorly by corresponding sacrococcygeal ligaments. Furthermore, at each side, a lateral sacrococcygeal ligament forms a foramen through which the S5 nerve root passes.[5]
Joints and Ligaments of the Pelvis
Various important joints and ligaments maintain the structural integrity of the bony pelvis. The pubic symphysis and sacrococcygeal joint have been described earlier.
The sacroiliac joint is formed by the articulation between the auricular surfaces of the median ilium and the pelvic surface of the sacrum.[10] The joint is reinforced anteriorly by the anterior sacroiliac ligament and posteriorly by the strong interosseous sacroiliac ligament and posterior sacroiliac ligaments.[5] These ligaments provide all the stability for the sacroiliac joint.
Other important ligaments in the region include the sacrotuberous, sacrospinous, and iliolumbar ligaments.[11] The sacrotuberous ligament is blended with the posterior sacroiliac ligament and attaches to the posterior superior and posterior inferior spines of the ilium, the transverse tubercles of the sacrum below the sacroiliac joint, and the upper part of the coccyx.[12] The sacrospinous ligament crosses the pelvic aspect of the sacrotuberous ligament obliquely, originating from the lower sacrum and upper coccyx and inserting at the spine of the ischium. The iliolumbar ligament has its base at the transverse process of the L5 vertebra, and from here, an upper band inserts at the iliac crest, and a lower band blends with the anterior sacroiliac ligament.[5]
The functions of the pelvic bones are locomotion, childbirth, and support to the abdominal viscera. The pelvis transmits the weight from the axial to the lower appendicular skeleton. Likewise, the pelvis bears the weight of the upper body when sitting. The bony structure also provides attachment sites for many abdominal, pelvic, and lower extremity muscles and provides attachment sites for external reproductive organs. Additionally, the pelvic girdle serves to protect the pelvic and abdominopelvic viscera.[2]
Embryology
The formation of the pelvic bones involves a fusion of multiple elements which allow articulation of the axial skeleton with the lower extremities. The hip bones (ilium, ischium, and pubis) remain separate but attach via the triradiate cartilage in early life. Upon puberty, these bones fuse to form the acetabulum, a socket on the lateral aspect of the hip where the femoral head articulates.
The lateral plate mesoderm forms the ilium, ischium, and pubis. These bones then undergo endochondral ossification, similar to long bones, but an initial blastemal structure forms, which undergoes chondrification—afterward, the sites of the primary ossification centers form. The sacrum undergoes this type of ossification as well.
Blood Supply and Lymphatics
Vascular supply to the hip bones comes from branches of both the external and internal iliac arteries. Both of these come from the bifurcation of the common iliac artery, which bifurcates at the level of the L5-S1 vertebral level. The external iliac artery travels along the pelvic brim, giving off the inferior epigastric and deep circumflex iliac arteries. The artery then transitions into the femoral artery after passing the inguinal ligament. The internal iliac artery travels posteromedial into the pelvis, bifurcating into the anterior and posterior divisions of the internal iliac artery.[13] The anterior division includes the umbilical, obturator, inferior vesical, uterine, vaginal, middle rectal, internal pudendal, and inferior gluteal. The posterior division consists of the iliolumbar, lateral sacral, and superior gluteal arteries.
The sacrum receives its blood supply from the lateral sacral and the median sacral arteries. The lateral sacral arteries are a branch of the internal iliac artery—the median artery branches off the aorta after it bifurcates into the internal and external iliac arteries.
The lymphatic system of the pelvis has many contributions and groups of lymph nodes. The main groups of lymph nodes are the external iliac lymph nodes, internal iliac lymph nodes, sacral lymph nodes, and the common iliac lymph nodes.
Nerves
Innervation of the pelvis includes mainly the sacral and coccygeal plexuses.
The sacral plexus derives from the L4-S4 nerve roots, and it sits on the internal surface of the piriformis muscle—most of the sacral nerves stemming from the sacral plexus exit through the greater sciatic notch. The sciatic nerve forms out of the sacral plexus and can be compressed by the muscle, causing radicular pain down the leg. This form of entrapment neuropathy caused by compression from the piriformis muscle is called piriformis muscle syndrome.[14]
The coccygeal plexus forms from the S4-S5 nerve roots and lies along the pelvic surface of the coccygeus muscle.
The autonomic system also provides innervation to the pelvis, which mainly courses via the inferior hypogastric plexus. This plexus is made of nerve fibers from the sympathetic splanchnic nerves, parasympathetic splanchnic nerves, and hypogastric nerves. The autonomic nerves travel to the organs via their corresponding splanchnic nerve group.[15]
Muscles
The pelvic bones are an attachment for many different muscle groups involving the abdomen, pelvis, perineum, and lower extremities. The muscles limited to the pelvis include the muscles of the pelvic wall and the pelvic diaphragm.
Along the anterolateral wall of the true pelvis lies the obturator internus muscle. This muscle extends from the bony surfaces of the pelvis into the lesser sciatic foramen and inserts on the greater trochanter. The muscle receives innervation from the nerve to the obturator internus (L5-S2). The obturator internus serves as an external rotator of the hip and strengthens the hip joint.[16]
Along the posterolateral surface of the true pelvis lies the piriformis muscle. This muscle extends from the bony surfaces of the sacrum and pelvis into the greater sciatic foramen, with its insertion on the greater trochanter of the femur. The muscle receives innervation from the anterior rami of S1 and S2. The piriformis also serves as an external rotator of the hip and strengthens the hip joint.[17]
The pelvic diaphragm consists of the coccygeus muscles and the levator ani muscles.
The coccygeus muscle is the most posterior and superior of the pelvic diaphragm muscles. This muscle extends from the ischial spines to attach to the lateral surface of the coccyx and inferior sacral segment. The innervation of the coccygeus comes from branches of the S4 and S5 spinal nerves. The coccygeus serves as the support for the pelvic viscera and flexes the coccyx.
The levator ani is subdivided into different muscle groups (pubococcygeus, puborectalis, and iliococcygeus), but the margins are ill-defined. These muscle groups extend from the anterior bony surfaces of the pelvis to attach to the perineal body, anococcygeal ligament, and walls of the viscera near the pelvic floor.[18] The muscles are innervated by the nerve to the levator ani, inferior anal nerve, and coccygeal plexus. They serve as support for the pelvic viscera.[19]
Physiologic Variants
Physiologic variants of the bony pelvis exist between males and females. The male pelvis is typically thicker and heavier than the lighter and thinner pelvis of the female. Males also tend to have a narrower pelvic opening than females.
Most physiological differences lie in variations of the pelvic girdle. There are four types classically described:
- The gynaecoid pelvis displays an oval shape with a wide transverse diameter. This variant is the most common type and provides adequate cavity space for a female to give birth.
- The android displays a heart-shaped inlet and is most common in males.
- The platypelloid type displays a wide inlet transversely but is short in the anterior-posterior axis. This type provides challenges for a female to give birth and is found among approximately 20% of women.[20]
- The anthropoid type is characterized by a wide anterior-posterior axis but is short in the transverse axis and is found in around 15% of women.[20]
Surgical Considerations
The diameter of the pelvic ring is a surgical consideration that must be considered when planning childbirth.[21] The capability of vaginally delivering a baby is limited to the anatomical structure of the woman’s pelvis, and the anteroposterior diameter of the pelvic inlet must, therefore, be assessed radiographically or with pelvic examination.[22] A diagonal conjugate is measured instead during the pelvic examination due to the inability to measure a true anteroposterior diameter. The distance between the ischial spines is also considered because this space is the narrowest part of the pelvic canal. A cesarean section will be an option if the anatomical structure makes vaginal birth difficult or dangerous for the health of the woman or baby.
Following pelvic trauma, reduction and fixation of pelvic fractures may be necessary. Depending on the type and severity of the trauma, plus the co-existence of any visceral injuries, a range of approaches and techniques can be used. In general, anterior and posterior approaches can be taken. However, in extremis, it may be most appropriate to undertake a complete trauma laparotomy to fully assess and treat the viscera and bony structures following trauma.[23]
The anterior approach to the bony pelvis can be open or percutaneous. An open approach can be performed via a Pfannenstiel incision and allows access to the urinary bladder in case of urological injury in trauma requiring operative management.[24] Anterior percutaneous fixation of pelvic fractures is achievable using an internal pelvic fixator (INFIX).[25]
Sacroiliac fixation can be performed via a posterior percutaneous approach under radiological guidance.[26][27] However, this approach is challenging owing to nearby neurovascular structures, so careful planning of the screw’s trajectory is required to avoid injury.[28] Patient factors such as obesity or dysmorphism can further complicate this approach, and in cases where it is not possible, an open posterior approach can be taken.[23]
Clinical Significance
Fractures of the pelvis most often result following direct trauma, for example, in pedestrian versus car accidents or a fall from significant heights, and may involve multiple bones of the pelvis or the hip joint. Pelvic fractures are potentially life-threatening, as more than 2 liters of blood can exsanguinate into the pelvic cavity without any evidence of external bleeding; for this reason, the management of pelvic fractures involves rapid fluid resuscitation and temporary external fixation to try and tamponade any internal bleeding while definitive treatment is planned.[29]
The contemporary classification of pelvic fractures used is that outlined by Young and Burgess. This classification system has a description of injuries resulting in force directed through the midline (anterior-posterior compression) from lateral to medial (lateral compression) or upwards off the midline (vertical shear).[30] The first two categories are further divided into three subtypes, as follows:
- Anterior-posterior compression (APC) injuries result from a force through the midline pubic symphysis. APC I injuries are defined as having less than 2.5 cm of widening at the symphysial joint and are considered clinically stable. APC II injuries demonstrate more than 2.5 cm diastasis at the symphysial joint, and there is disruption of the anterior part of the sacroiliac joint but not the posterior aspect. They are considered rotationally unstable but vertically stable. APC III injuries include all the features of the APC II injuries but with disruption of the posterior part of the sacroiliac joint, and therefore equate to a complete hemipelvis separation. They are unstable rotationally and vertically.[31]
- Lateral compression (LC) injuries are more common than APC injuries and result from a force from lateral to medial. LC I injuries are stable and comprise an oblique fracture of the pubic rami with an ipsilateral fracture of the sacral ala. LC II injuries also have an ipsilateral iliac wing fracture and are rotationally unstable but vertically stable. LC III injuries result from a greater force and cause contralateral anterior and posterior sacroiliac joint disruption.[32]
- Vertical shear (VS) injury results from an axial force delivered lateral to the midline and are the rarest, most severe, and most unstable injury. This results in complete ligamentous disruption in the hemipelvis and pubic fractures.[33]
Timely operative fixation is key to managing unstable and severe pelvic fractures and should be undertaken as soon as possible following appropriate trauma resuscitation and stabilization.[23] The Young-Burgess classification is also useful for predicting transfusion requirements, which have been found to be increased in APC III, LC II, and LC III fractures compared to the other groups.[34]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
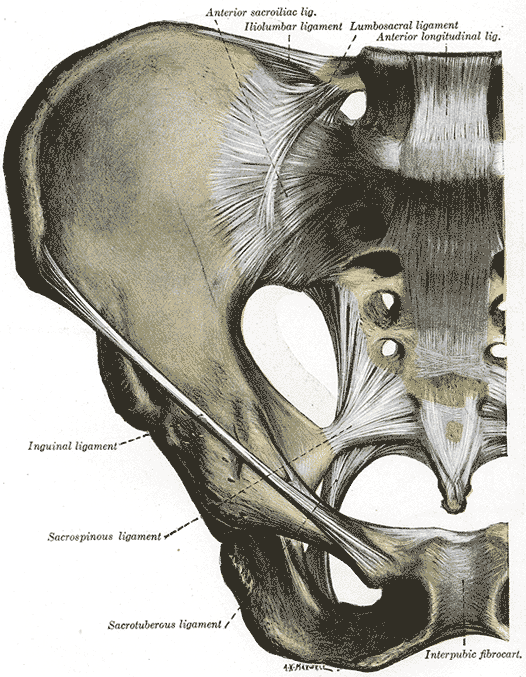
Anterior Articulations, Pelvis. The illustration depicts the sacroiliac, iliolumbar, lumbosacral, longitudinal, inguinal, sacrospinous, sacrotuberous ligaments, intrapubic fibrocartilage, and hip.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
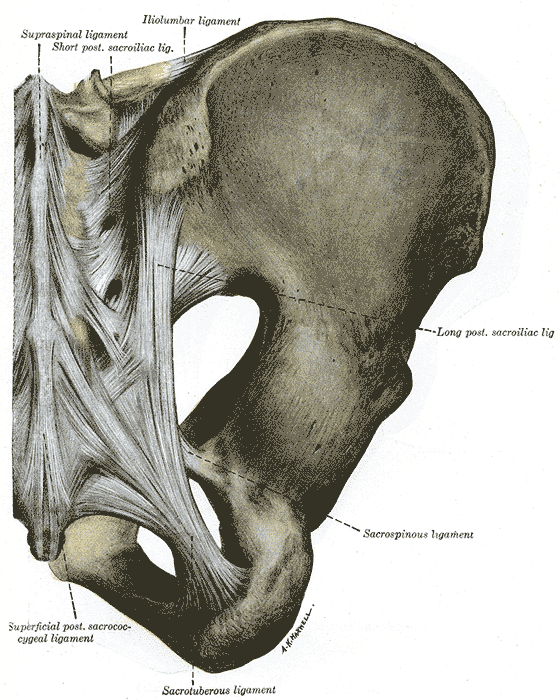
Posterior Articulations, Pelvis. The illustrated image portrays the supraspinal, short posterior, sacroiliac, iliolumbar, sacrospinous, sacrotuberous, superficial posterior sacrococcygeal ligaments, and hip.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
DeSilva JM, Rosenberg KR. Anatomy, Development, and Function of the Human Pelvis. Anatomical record (Hoboken, N.J. : 2007). 2017 Apr:300(4):628-632. doi: 10.1002/ar.23561. Epub [PubMed PMID: 28297176]
Fritsch H, Lienemann A, Brenner E, Ludwikowski B. Clinical anatomy of the pelvic floor. Advances in anatomy, embryology, and cell biology. 2004:175():III-IX, 1-64 [PubMed PMID: 15152384]
Level 3 (low-level) evidenceFritsch H, Hötzinger H. Tomographical anatomy of the pelvis, visceral pelvic connective tissue, and its compartments. Clinical anatomy (New York, N.Y.). 1995:8(1):17-24 [PubMed PMID: 7697508]
McGaugh JM, Brismée JM, Dedrick GS, Jones EA, Sizer PS. Comparing the anatomical consistency of the posterior superior iliac spine to the iliac crest as reference landmarks for the lumbopelvic spine: a retrospective radiological study. Clinical anatomy (New York, N.Y.). 2007 Oct:20(7):819-25 [PubMed PMID: 17729332]
Level 2 (mid-level) evidenceAshby K, Yilmaz E, Mathkour M, Olewnik Ł, Hage D, Iwanaga J, Loukas M, Tubbs RS. Ligaments stabilizing the sacrum and sacroiliac joint: a comprehensive review. Neurosurgical review. 2022 Feb:45(1):357-364. doi: 10.1007/s10143-021-01625-y. Epub 2021 Aug 25 [PubMed PMID: 34432162]
Becker I, Woodley SJ, Stringer MD. The adult human pubic symphysis: a systematic review. Journal of anatomy. 2010 Nov:217(5):475-87. doi: 10.1111/j.1469-7580.2010.01300.x. Epub 2010 Sep 14 [PubMed PMID: 20840351]
Level 1 (high-level) evidenceWu LP, Li YK, Li YM, Zhang YQ, Zhong SZ. Variable morphology of the sacrum in a Chinese population. Clinical anatomy (New York, N.Y.). 2009 Jul:22(5):619-26. doi: 10.1002/ca.20809. Epub [PubMed PMID: 19484801]
Level 2 (mid-level) evidenceMahato NK. Relationship of sacral articular surfaces and gender with occurrence of lumbosacral transitional vertebrae. The spine journal : official journal of the North American Spine Society. 2011 Oct:11(10):961-5. doi: 10.1016/j.spinee.2011.08.007. Epub 2011 Sep 15 [PubMed PMID: 21924685]
Level 2 (mid-level) evidenceAggarwal A, Kaur H, Batra YK, Aggarwal AK, Rajeev S, Sahni D. Anatomic consideration of caudal epidural space: a cadaver study. Clinical anatomy (New York, N.Y.). 2009 Sep:22(6):730-7. doi: 10.1002/ca.20832. Epub [PubMed PMID: 19637298]
Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Journal of anatomy. 2012 Dec:221(6):537-67. doi: 10.1111/j.1469-7580.2012.01564.x. Epub 2012 Sep 19 [PubMed PMID: 22994881]
Level 3 (low-level) evidenceHammer N, Steinke H, Lingslebe U, Bechmann I, Josten C, Slowik V, Böhme J. Ligamentous influence in pelvic load distribution. The spine journal : official journal of the North American Spine Society. 2013 Oct:13(10):1321-30. doi: 10.1016/j.spinee.2013.03.050. Epub 2013 Jun 5 [PubMed PMID: 23755919]
Aldabe D, Hammer N, Flack NAMS, Woodley SJ. A systematic review of the morphology and function of the sacrotuberous ligament. Clinical anatomy (New York, N.Y.). 2019 Apr:32(3):396-407. doi: 10.1002/ca.23328. Epub 2019 Feb 5 [PubMed PMID: 30592090]
Level 1 (high-level) evidenceKachlik D, Vobornik T, Dzupa V, Marvanova Z, Toupal O, Navara E, Stevulova N, Baca V. Where and what arteries are most likely injured with pelvic fractures?: The Influence of Localization, Shape, and Fracture Dislocation on the Arterial Injury During Pelvic Fractures. Clinical anatomy (New York, N.Y.). 2019 Jul:32(5):682-688. doi: 10.1002/ca.23372. Epub 2019 Apr 2 [PubMed PMID: 30873674]
Michel F, Decavel P, Toussirot E, Tatu L, Aleton E, Monnier G, Garbuio P, Parratte B. The piriformis muscle syndrome: an exploration of anatomical context, pathophysiological hypotheses and diagnostic criteria. Annals of physical and rehabilitation medicine. 2013 May:56(4):300-11. doi: 10.1016/j.rehab.2013.03.006. Epub 2013 Apr 30 [PubMed PMID: 23684469]
Shoja MM, Sharma A, Mirzayan N, Groat C, Watanabe K, Loukas M, Tubbs RS. Neuroanatomy of the female abdominopelvic region: A review with application to pelvic pain syndromes. Clinical anatomy (New York, N.Y.). 2013 Jan:26(1):66-76. doi: 10.1002/ca.22200. Epub 2012 Nov 23 [PubMed PMID: 23175283]
Fröhlich B, Hötzinger H, Fritsch H. Tomographical anatomy of the pelvis, pelvic floor, and related structures. Clinical anatomy (New York, N.Y.). 1997:10(4):223-30 [PubMed PMID: 9213037]
Lawson JO. Pelvic anatomy. I. Pelvic floor muscles. Annals of the Royal College of Surgeons of England. 1974 May:54(5):244-52 [PubMed PMID: 4829749]
Guo M, Li D. Pelvic floor images: anatomy of the levator ani muscle. Diseases of the colon and rectum. 2007 Oct:50(10):1647-55 [PubMed PMID: 17762969]
Rocca Rossetti S. Functional anatomy of pelvic floor. Archivio italiano di urologia, andrologia : organo ufficiale [di] Societa italiana di ecografia urologica e nefrologica. 2016 Mar 31:88(1):28-37. doi: 10.4081/aiua.2016.1.28. Epub 2016 Mar 31 [PubMed PMID: 27072173]
Vučinić N, Paulsen F, Milinkov M, Nikolić MB, Todorović ST, Knezi N, Nikolić U. A survey of pelvic types on computed tomography images. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2022 Aug:243():151942. doi: 10.1016/j.aanat.2022.151942. Epub 2022 Apr 2 [PubMed PMID: 35378253]
Level 3 (low-level) evidenceWall-Scheffler CM, Myers MJ. The Biomechanical and Energetic Advantages of a Mediolaterally Wide Pelvis in Women. Anatomical record (Hoboken, N.J. : 2007). 2017 Apr:300(4):764-775. doi: 10.1002/ar.23553. Epub [PubMed PMID: 28297181]
Pavličev M, Romero R, Mitteroecker P. Evolution of the human pelvis and obstructed labor: new explanations of an old obstetrical dilemma. American journal of obstetrics and gynecology. 2020 Jan:222(1):3-16. doi: 10.1016/j.ajog.2019.06.043. Epub 2019 Jun 25 [PubMed PMID: 31251927]
Mostafa AMHAM, Kyriacou H, Chimutengwende-Gordon M, Khan WS. An overview of the key principles and guidelines in the management of pelvic fractures. Journal of perioperative practice. 2021 Sep:31(9):341-348. doi: 10.1177/1750458920947358. Epub 2020 Sep 8 [PubMed PMID: 32894996]
Level 3 (low-level) evidenceStern N, Pignanelli M, Welk B. The management of an extraperitoneal bladder injury associated with a pelvic fracture. Canadian Urological Association journal = Journal de l'Association des urologues du Canada. 2019 Jun:13(6 Suppl4):S56-S60. doi: 10.5489/cuaj.5930. Epub [PubMed PMID: 31194928]
Steer R, Balendra G, Matthews J, Wullschleger M, Reidy J. The use of anterior subcutaneous internal fixation (INFIX) for treatment of pelvic ring injuries in major trauma patients, complications and outcomes. SICOT-J. 2019:5():22. doi: 10.1051/sicotj/2019019. Epub 2019 Jun 28 [PubMed PMID: 31250805]
Chen HW, Liu GD, Fei J, Yi XH, Pan J, Ou S, Zhou JH. Treatment of unstable posterior pelvic ring fracture with percutaneous reconstruction plate and percutaneous sacroiliac screws: a comparative study. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association. 2012 Sep:17(5):580-7. doi: 10.1007/s00776-012-0257-1. Epub 2012 Jul 19 [PubMed PMID: 22810807]
Level 2 (mid-level) evidenceQi H, Geng X, Yu X, Chen W, Jia J, Tian W. Posterior INFIX for Treating Unilateral Unstable Sacral Fractures. Orthopaedic surgery. 2022 Apr:14(4):750-757. doi: 10.1111/os.13251. Epub 2022 Mar 27 [PubMed PMID: 35343061]
Level 2 (mid-level) evidenceDo MT, Levine AD, Liu RW. An anatomical study defining the safe range of angles in percutaneous iliosacral and transsacral screw fixation. Clinical anatomy (New York, N.Y.). 2022 Apr:35(3):280-287. doi: 10.1002/ca.23807. Epub 2021 Nov 19 [PubMed PMID: 34766656]
Fierro NM, Dhillon NK, Siletz AE, Muníz T, Barmparas G, Ley EJ, Hashim YM. Which Pelvic Fractures Are Associated With Extravasation on Angiography? The American surgeon. 2022 Oct:88(10):2493-2498. doi: 10.1177/00031348221101514. Epub 2022 May 12 [PubMed PMID: 35546075]
Young JW, Burgess AR, Brumback RJ, Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986 Aug:160(2):445-51 [PubMed PMID: 3726125]
Alton TB, Gee AO. Classifications in brief: young and burgess classification of pelvic ring injuries. Clinical orthopaedics and related research. 2014 Aug:472(8):2338-42. doi: 10.1007/s11999-014-3693-8. Epub 2014 May 28 [PubMed PMID: 24867452]
Putnis SE, Pearce R, Wali UJ, Bircher MD, Rickman MS. Open reduction and internal fixation of a traumatic diastasis of the pubic symphysis: one-year radiological and functional outcomes. The Journal of bone and joint surgery. British volume. 2011 Jan:93(1):78-84. doi: 10.1302/0301-620X.93B1.23941. Epub [PubMed PMID: 21196548]
Steelman K, Russell R, Vaidya R. Bilateral vertical shear sacroiliac joint dislocations treated with bilateral triangular osteosynthesis in a young female: A case report. Trauma case reports. 2021 Jun:33():100485. doi: 10.1016/j.tcr.2021.100485. Epub 2021 Apr 21 [PubMed PMID: 33997229]
Level 3 (low-level) evidenceManson T, O'Toole RV, Whitney A, Duggan B, Sciadini M, Nascone J. Young-Burgess classification of pelvic ring fractures: does it predict mortality, transfusion requirements, and non-orthopaedic injuries? Journal of orthopaedic trauma. 2010 Oct:24(10):603-9. doi: 10.1097/BOT.0b013e3181d3cb6b. Epub [PubMed PMID: 20871246]
Level 2 (mid-level) evidence