Introduction
Anorexia nervosa is an eating disorder defined by restriction of energy intake relative to requirements, leading to a significantly low body weight. Patients will have an intense fear of gaining weight and distorted body image with the inability to recognize the seriousness of their significantly low body weight.[1][2][3]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The success of many professions depends on a person's weight. Models and actors portray a level of thinness that is difficult to attain, and it is enhanced by make-up and photographic alterations. Athletes in sports such as ballet, long-distance running, and martial arts are pressured to maintain lean body weights to outperform the competition. Media outlets promote diet secrets and weight loss tips in excess. Populations such as maturing females identify thin body types with increased self-esteem and link weight loss with self-control.[4][5]
Epidemiology
Anorexia nervosa is more common in females than males. Onset is late adolescence and early adulthood. Lifetime prevalence is 0.3% to 1% (European studies have demonstrated a prevalence of 2% to 4%), irrespective of culture, ethnicity, and race. Risk factors for eating disorders include childhood obesity, female sex, mood disorders, personality traits (impulsivity and perfectionism), sexual abuse, or weight-related concerns from family or peer environments.[6][7][8]
Pathophysiology
Studies demonstrate biological factors play a role in the development of anorexia nervosa in addition to environmental factors. Genetic correlations exist between educational attainment, neuroticism, and schizophrenia. Patients with anorexia nervosa have altered brain function and structure there are deficits in neurotransmitters dopamine (eating behavior and reward) and serotonin (impulse control and neuroticism), differential activation of the corticolimbic system (appetite and fear), and diminished activity among the frontostriatal circuits (habitual behaviors). Patients have co-morbid psychiatric disorders such as major depressive disorder and generalized anxiety disorder.
History and Physical
Patients will report symptoms such as amenorrhea, cold intolerance, constipation, extremity edema, fatigue, and irritability. They may describe restrictive behaviors related to food like calorie counting or portion control, and purging methods, for example, self-induced vomiting or use of diuretics or laxatives. Many exercise compulsively for extended periods of time. Patients with anorexia nervosa develop multiple complications related to prolonged starvation and purging behaviors.
Evaluation
Workup includes a thorough medical history (comprehensive review of systems, family and social history, medications including nonprescribed, past medical and psychiatric history, prior abuse) and physical exam (looking for complications above). Basic labs include coagulation panel, complete blood count, complete metabolic profile, 25-hydroxyvitamin D, testosterone (males), thyroid-stimulating hormone, and urine testing (beta-hCG [females] and drugs, either illicit or prescription). An electrocardiogram is recommended to assess for life-threatening arrhythmias. Additional studies may be necessary if BMI is less than 14 kg/m, for example, echocardiogram in patients with hemodynamic compromise (dyspnea, murmurs, syncope) or computed tomography of the abdomen to rule out superior mesenteric artery syndrome or amenorrhea more than 9 months (dual-energy x-ray absorptiometry).[9][8]
Complications of anorexia nervosa are listed:
- Cardiovascular: bradycardia, dilated cardiomyopathy, electrolyte-induced arrhythmias, hypotension, mitral valve prolapse, pericardial effusion
- Constitutional: arrested growth, hypothermia, low body mass index (BMI), muscle wasting
- Dermatologic: carotenoderma, lanugo, xerosis
- Endocrine: hypothalamic hypogonadism, osteoporosis
- Gastrointestinal: constipation (laxative abuse), gastroparesis
- Hematologic: cytopenias (inc. normocytic anemia), bone marrow hypoplasia/aplasia
- Neurologic: brain atrophy, peripheral neuropathy (mineral and vitamin deficiencies)
- Obstetric: antenatal and postnatal complications
- Psychiatric: depression, impaired concentration, insomnia, irritability
- Renal and electrolytes: hypokalemic metabolic acidosis or alkalosis (laxative or diuretic abuse, resp.), prerenal renal failure, refeeding syndrome.
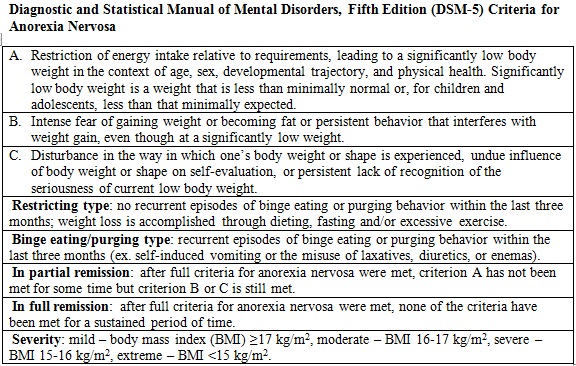
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides the diagnostic criteria for anorexia nervosa (A-C). It classifies the disease by type, status, and severity.
Of note, amenorrhea has been removed from the DSM-5 criteria. Patients who meet the new criteria and continue to menstruate have similar outcomes as those who do not.
Other eating disorders have similar features to anorexia nervosa. Avoidant or restrictive food intake disorder involves food restriction with failure to meet the nutritional need. While patients are often underweight, this disturbance does not meet diagnostic criteria for anorexia nervosa. Individuals with binge eating disorder eat excessive amounts of calories in a short period with a lack of self-control but do not display compensatory behaviors such as purging or restriction. Patients with bulimia nervosa will binge and purge without a corresponding low BMI. Pica refers to chronic ingestion of nonfood substances and may be a manifestation of underlying medical or psychiatric condition. For example, patients with anorexia nervosa may eat toilet paper when they are hungry. Rumination disorder occurs when patients repeatedly regurgitate food for one month when no other medical condition can be identified and does not occur solely during the course of another eating disorder. Other specified feeding or eating disorder refers to conditions with symptoms that impair functioning but do not meet criteria for a specific eating disorder, for example, patients who meet criteria for anorexia nervosa but have BMI more than 18.5 kg/m are classified as “atypical anorexia nervosa.”
Major depressive disorder can cause anorexia and weight loss. However, patients are not obsessed with body habitus. Patients with obsessive-compulsive disorder may have food rituals but maintain a normal weight. Patients who abuse stimulants such as cocaine and methamphetamine experience weight loss through increased metabolism and concentrated efforts to obtain illicit substances rather than consume calories.
Medical conditions can cause weight loss. Examples are celiac disease, hyperthyroidism, inflammatory bowel disease, malignancy, poorly controlled diabetes mellitus, primary adrenal insufficiency, and tuberculosis. The diagnosis will come from the history and physical examination. Order labs as dictated by the clinical picture.
Treatment / Management
Treatment for anorexia nervosa is centered on nutrition rehabilitation and psychotherapy. Patients who need inpatient treatment have the following characteristics:
- Existing psychiatric disorders requiring hospitalization
- High risk for suicide (intent with highly lethal plan or failed attempt)
- Lack of support system (severe family conflict or homelessness)
- Limited access (lives too far away to participate in a daily treatment program)
- Medically unstable (bradycardia, dehydration, hypoglycemia or poorly controlled diabetes, hypokalemia or other electrolyte imbalances indicative of refeeding syndrome, hypothermia, hypotension, organ compromise requiring acute treatment)
- Poorly motivated to recover (uncooperative, preoccupied with intrusive thoughts)
- Purging behaviors that are persistent, severe, and occur multiple times a day
- Severe anorexia nervosa (less than 70% of ideal body weight or acute weight loss with food refusal)
- Supervised feeding and/or specialized feeding (nasogastric tube) required
- Unable to stop compulsively exercising (not a sole indication for hospitalization).
Outpatient treatment includes intensive therapy (2 to 3 hours per weekday) and partial hospitalization (6 hours per day). Pediatric patients benefit from family-based psychotherapy to explore underlying dynamics and restructure the home environment.
Refeeding syndrome can occur following prolonged starvation. As the body utilizes glucose to produce molecules of adenosine triphosphate (ATP), it depletes the remaining stores of phosphorus. Also, glucose entry into cells is mediated by insulin and occurs rapidly following long periods without food. Both cause electrolyte abnormalities such as hypophosphatemia and hypokalemia, triggering cardiac and respiratory compromise. Patients should be followed carefully for signs of refeeding syndrome and electrolytes closely monitored.
Pharmacotherapy is not used initially. For acutely ill patients who do not respond to initial treatment, olanzapine is a first-line medication. Other antipsychotics have not demonstrated similar effects on weight gain. For patients who are not acutely ill but have co-morbid psychiatric conditions such as generalized anxiety disorder or major depressive disorder, combination therapy with selective serotonin reuptake inhibitors (SSRIs) and therapy is best. Patients who do not respond to SSRIs may need a second-generation antipsychotic. Tricyclic antidepressants (TCAs) are less preferred due to concerns about cardiotoxicity, especially in malnourished patients. Bupropion is contraindicated in patients with eating disorders due to the increased risk of seizures.[10][11][12](A1)
Differential Diagnosis
- Cancer
- Chronic mesenteric ischemia
- Achalasia
- Malabsorption
- Hyperthyroidism
- Irritable bowel syndrome
- Celiac disease
Prognosis
Remission in AN varies. Three-fourths of patients treated in out-patient settings remit within 5 years and the same percentage experience intermediate-good outcomes (including weight gain). Relapse is more common in patients who are older with a longer duration of disease or lower body fat/weight at the end of treatment, have co-morbid psychiatric disorders, or receive therapy outside of a specialized clinic. Patients who achieve partial remission often develop another form of eating disorder (ex. bulimia nervosa or unspecified eating disorder).
All-cause mortality is greater in AN compared to the rest of the population. It has one of the highest mortality rates of all eating disorders due to medical complications, substance abuse, and suicide. Patients with AN have increased rates of suicide and this accounts for 25% of deaths associated.
Complications
- Amenorrhea
- Delayed puberty
- Hypercarotenemia
- Hypothermia
- Hypoglycemia
- Osteoporosis
- Failure to thrive
- Cardiomyopathy
- Bradycardia
- Arrhythmias
- Renal failure
- Constipation
- Peripheral neuropathy
- Pancytopenia
- Infertility
Deterrence and Patient Education
Anorexia nervosa is a psychiatric disease in which patients restrict their food intake relative to their energy requirements through eating less, exercising more, and/or purging food through laxatives and vomiting. Despite being severely underweight, they do not recognize it and have distorted body images. They can develop complications from being underweight and purging food. Diagnose by history, physical, and lab work that rules out other conditions that can make people lose weight. Treatment includes gain weight (sometimes in a hospital if severe), therapy to address body image, and management of complications from malnourishment.
Enhancing Healthcare Team Outcomes
Anorexia nervosa is a serious eating disorder that has very high morbidity. The disorder is usually managed with an interprofessional team that consists of a psychiatrist, dietitian, social worker, internist, endocrinologist, gastroenterologist, and nurses. The disorder cannot be prevented and there is no cure. Hence patient and family education is key to preventing high morbidity. The dietitian should educate the family on the importance of nutrition and limiting exercise. The mental health nurse should educate the patient on changes in behavior, easing stress, and overcoming any emotional issues. The pharmacist should educate the patient and family on the use of drugs like laxatives and weight loss pills. Only through close follow-up and monitoring can patient outcomes be improved. [13][14] [Level 5]
Evidence-based Outcomes
Remission in anorexia nervosa varies. Three-fourths of patients treated in out-patient settings remit within five years and the same percentage experience intermediate-good outcomes, including weight gain. Relapse is more common in patients who are older with a longer duration of disease or lower body fat/weight at the end of treatment, have co-morbid psychiatric disorders, or receive therapy outside of a specialized clinic. Often, patients who achieve partial remission develop another form of eating disorders like bulimia nervosa or unspecified eating disorder.
All-cause mortality is greater in anorexia nervosa compared to the rest of the population. It has one of the highest mortality rates of all eating disorders due to medical complications, substance abuse, and suicide. Patients with anorexia nervosa have increased rates of suicide, and this accounts for 25% of deaths associated with the disorder. [15][16][9] [Level 5]
Media
(Click Image to Enlarge)
References
Strand M, von Hausswolff-Juhlin Y, Welch E. [ARFID: food restriction without fear of weight gain]. Lakartidningen. 2018 Sep 11:115():. pii: E97R. Epub 2018 Sep 11 [PubMed PMID: 30226628]
Phillipou A, Rossell SL, Castle DJ. Anorexia nervosa or starvation? The European journal of neuroscience. 2018 Dec:48(11):3317-3318. doi: 10.1111/ejn.14158. Epub 2018 Sep 30 [PubMed PMID: 30218629]
Burton AL, Mitchison D, Hay P, Donnelly B, Thornton C, Russell J, Swinbourne J, Basten C, Goldstein M, Touyz S, Abbott MJ. Beliefs about Binge Eating: Psychometric Properties of the Eating Beliefs Questionnaire (EBQ-18) in Eating Disorder, Obese, and Community Samples. Nutrients. 2018 Sep 14:10(9):. doi: 10.3390/nu10091306. Epub 2018 Sep 14 [PubMed PMID: 30223500]
Gander M, Sevecke K, Buchheim A. Disorder-specific attachment characteristics and experiences of childhood abuse and neglect in adolescents with anorexia nervosa and a major depressive episode. Clinical psychology & psychotherapy. 2018 Nov:25(6):894-906. doi: 10.1002/cpp.2324. Epub 2018 Sep 14 [PubMed PMID: 30216616]
Zayas LV, Wang SB, Coniglio K, Becker K, Murray HB, Klosterman E, Kay B, Bean P, Weltzin T, Franko DL, Eddy KT, Thomas JJ. Gender differences in eating disorder psychopathology across DSM-5 severity categories of anorexia nervosa and bulimia nervosa. The International journal of eating disorders. 2018 Sep:51(9):1098-1102. doi: 10.1002/eat.22941. Epub 2018 Sep 7 [PubMed PMID: 30193008]
Levinson CA, Zerwas SC, Brosof LC, Thornton LM, Strober M, Pivarunas B, Crowley JJ, Yilmaz Z, Berrettini WH, Brandt H, Crawford S, Fichter MM, Halmi KA, Johnson C, Kaplan AS, La Via M, Mitchell J, Rotondo A, Woodside DB, Kaye WH, Bulik CM. Associations between dimensions of anorexia nervosa and obsessive-compulsive disorder: An examination of personality and psychological factors in patients with anorexia nervosa. European eating disorders review : the journal of the Eating Disorders Association. 2019 Mar:27(2):161-172. doi: 10.1002/erv.2635. Epub 2018 Aug 22 [PubMed PMID: 30136346]
Nagata JM, Garber AK, Tabler JL, Murray SB, Bibbins-Domingo K. Prevalence and Correlates of Disordered Eating Behaviors Among Young Adults with Overweight or Obesity. Journal of general internal medicine. 2018 Aug:33(8):1337-1343. doi: 10.1007/s11606-018-4465-z. Epub 2018 Jun 11 [PubMed PMID: 29948810]
Sacco B, Kelley U. Diagnosis and Evaluation of Eating Disorders in the Pediatric Patient. Pediatric annals. 2018 Jun 1:47(6):e244-e249. doi: 10.3928/19382359-20180523-02. Epub [PubMed PMID: 29898236]
Dittmer N, Voderholzer U, von der Mühlen M, Marwitz M, Fumi M, Mönch C, Alexandridis K, Cuntz U, Jacobi C, Schlegl S. Specialized group intervention for compulsive exercise in inpatients with eating disorders: feasibility and preliminary outcomes. Journal of eating disorders. 2018:6():27. doi: 10.1186/s40337-018-0200-8. Epub 2018 Sep 11 [PubMed PMID: 30214803]
Level 2 (mid-level) evidenceHale MD, Logomarsino JV. The use of enteral nutrition in the treatment of eating disorders: a systematic review. Eating and weight disorders : EWD. 2019 Apr:24(2):179-198. doi: 10.1007/s40519-018-0572-4. Epub 2018 Sep 8 [PubMed PMID: 30196528]
Level 1 (high-level) evidenceLock J. Family therapy for eating disorders in youth: current confusions, advances, and new directions. Current opinion in psychiatry. 2018 Nov:31(6):431-435. doi: 10.1097/YCO.0000000000000451. Epub [PubMed PMID: 30063479]
Level 3 (low-level) evidenceGrenon R, Carlucci S, Brugnera A, Schwartze D, Hammond N, Ivanova I, Mcquaid N, Proulx G, Tasca GA. Psychotherapy for eating disorders: A meta-analysis of direct comparisons. Psychotherapy research : journal of the Society for Psychotherapy Research. 2019 Oct:29(7):833-845. doi: 10.1080/10503307.2018.1489162. Epub 2018 Jun 29 [PubMed PMID: 29958509]
Level 1 (high-level) evidenceVust S, Cook-Darzens S, Lier F, Ambresin AE. [Adolescents suffering from anorexia nervosa: an evidence-based approach of the parent's role in 2018]. Revue medicale suisse. 2018 Apr 18:14(603):835-838 [PubMed PMID: 29668146]
Gómez-Candela C, Palma Milla S, Miján-de-la-Torre A, Rodríguez Ortega P, Matía Martín P, Loria Kohen V, Campos Del Portillo R, Martín-Palmero Á, Virgili Casas MªN, Martínez Olmos MÁ, Mories Álvarez MªT, Castro Alija MªJ, Martín-Palmero Á. [Consensus document about the nutritional evaluation and management of eating disorders: anorexia nervosa]. Nutricion hospitalaria. 2018 Mar 7:35(Spec No1):11-48. doi: 10.20960/nh.1561. Epub 2018 Mar 7 [PubMed PMID: 29565628]
Level 3 (low-level) evidenceVásquez N, Urrejola P, Vogel M. [An update on inpatient treatment of anorexia nervosa: practical recommendations]. Revista medica de Chile. 2017 May:145(5):650-656. doi: 10.4067/S0034-98872017000500013. Epub [PubMed PMID: 28898342]
Ziser K, Mölbert SC, Stuber F, Giel KE, Zipfel S, Junne F. Effectiveness of body image directed interventions in patients with anorexia nervosa: A systematic review. The International journal of eating disorders. 2018 Oct:51(10):1121-1127. doi: 10.1002/eat.22946. Epub 2018 Sep 6 [PubMed PMID: 30189104]
Level 1 (high-level) evidence