Introduction
Ocular ultrasound has many potential benefits in the evaluation of patients presenting to the emergency department with acute vision loss, ocular trauma, headache or concern for increased intracranial pressure.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
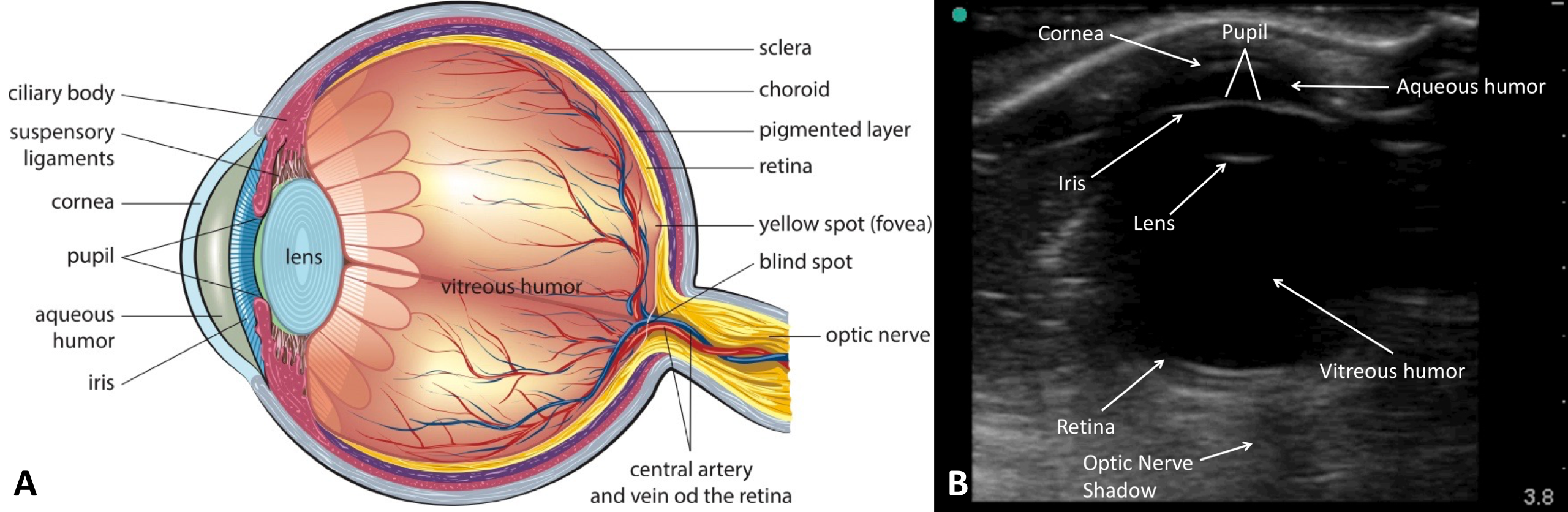
Comprehensive understanding of the anatomy of the globe and surrounding structures is critical for a provider performing point of care ocular ultrasound.
Fat and muscle within the orbital cavity surround the globe which is comprised of the sclera, uvea, and retina which all surround the aqueous and vitreous humor.
-
The sclera is the outermost layer of the eye. It acts as a protective barrier which surrounds the entire globe and is contiguous with the dural sheath of the optic nerve posteriorly. [1]
-
The uvea lies below the sclera and consists of the iris, ciliary body, and choroid plexus. The iris is a pigmented ring with a central opening, the pupil, and connects to the ciliary body peripherally. This creates a separation between the anterior and posterior chambers of the globe. The lens is positioned just posterior to the iris. The ciliary body connects the iris to the ciliary muscle, and the choroid forms a center vascular layer between the sclera and the retinal pigment epithelium. The choroid is also attached to the lens via the zonular fibers. [1]
-
The retina is the innermost layer of the eye. It is comprised of a sensory layer that contains photoreceptors, ganglion cells and the retinal pigment epithelium layer attached to the choroid. Of note, the retinal layers are attached only to the optic disc and the ora serrata. Intraocular pressure holds the retina otherwise in place. Two important parts of the retina are the optic disc, where the central retinal artery and vein enter, and the macula which is the thinnest portion of the retina. [1]
Important vasculature of the eye includes the central retinal artery, which originates from the ophthalmic artery, and the central retinal vein. The optic nerve provides sensory innervation to the eye. These three structures travel together in the optic nerve sheath which contains cerebrospinal fluid and communicates directly with the subarachnoid space. [1]
Indications
Vision Loss
Retinal and Vitreous Detachment
-
Often presents with complaints of “flashes” or “floaters” in vision, partial or complete vision loss. Retinal detachment is visualized on ultrasound as a mobile hyperechoic membrane or flap, often described as having serpentine motion with eye movement. Retinal detachments are tethered to the optic nerve and ora serrata. Posterior vitreous detachments have lower echogenicity and are not tethered to the optic disc. [2][3][4][5]
Vitreous Hemorrhage
-
Vitreous hemorrhage appears as a heterogeneous matter within the globe that will swirl when the eye is moved. This has been described as “snow globe” effect. It may also occur in the setting of trauma. [6][3]
Central Retinal Artery Occlusion
-
Presents with painless acute vision loss. Case reports have described central retinal artery occlusion on ultrasound as a hyperechoic spot posterior to the globe, confirmed with lack of arterial flow with color Doppler. [7]
Headache
Increased Intracranial Pressure and Papilledema
-
The optic nerve is contained within a dural sheath that communicates directly with the subarachnoid space. When intracranial pressure rises the nerve sheath expands and eventually the optic disc bulges into the vitreous chamber. This is referred to as papilledema and can be visualized on ultrasound. Studies have shown a correlation between increased intracranial pressure and optic nerve sheath diameter greater than 5 mm, measured 3 mm posterior to the retina. Papilledema may also be directly visualized with ultrasound as a bulging optic disc elevated more than 0.6 mm from the retina. [8][9][10][11]
Trauma
Foreign Body
-
Foreign bodies that are echogenic such as metal, glass or wood can be visualized within the globe. The presence of a foreign body should raise suspicion of globe rupture, and ocular ultrasound should be discontinued. [2][12]
Lens Dislocation (ectopia lentis)
-
The lens can be visualized in the vitreous chamber outside its normal position behind the iris. [2][6]
Globe Rupture
-
If there is a high clinical suspicion of globe perforation or rupture ultrasound examination is not recommended. The typical appearance of a globe rupture on ultrasound is that of a heterogeneous collection of hematoma, blood and vitreous humor in the posterior chamber. [2]
Retrobulbar Hematoma
-
An accumulation of blood in the retrobulbar space that can lead to pain increased intraocular pressure and stretching of the optic nerve. It usually occurs in the setting of trauma and can be rapidly progressive and is an ocular emergency. Retrobulbar collections of blood and hematoma may be seen on ocular ultrasound. [2]
Increased Intracranial Pressure
-
Can be evaluated using optic nerve sheath diameter as described above. In clinical situations where concern for increased intracranial pressure is high, ocular ultrasound has the added benefit of being easily repeatable for frequent monitoring of optic nerve sheath diameter. This can be especially helpful if the patient is sedated or otherwise unable to participate in a neurologic exam. [8][9][10][11]
Consensual Pupillary Response
-
Significant periorbital soft tissue swelling may prevent examination of the direct pupillary reflex of the affected eye. Ocular ultrasound can be used in this setting to visualize the affected eye consensual pupillary response.
Vitreous Hemorrhage
-
Vitreous hemorrhage appears as a heterogeneous matter within the globe that will swirl when the eye is moved. This has been described as “snow globe” effect. [2][6]
Retinal Detachment
Contraindications
Practitioners should not perform ocular ultrasound if there is a concern for globe rupture. If signs of globe rupture are noted during the exam, the ultrasound examination should be discontinued.
Equipment
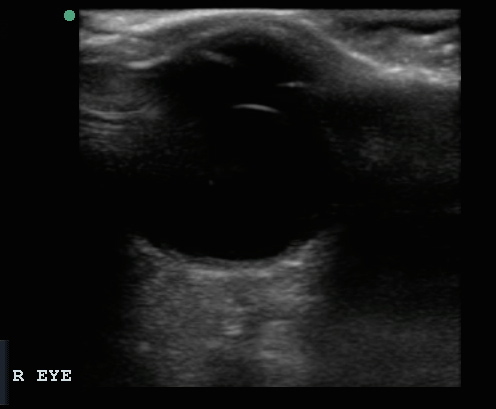
Ocular ultrasound should be performed with the high-frequency linear probe, and many ultrasound machines have an ocular setting.
Preparation
Materials needed for the exam are an ultrasound with a linear probe, ultrasound gel, and a clear plastic film such as a Tegaderm. Sterile petroleum jelly, antibiotic ointment, or ophthalmic ointment may be useful but are not necessary.
Technique or Treatment
If desired, a small amount of ointment may be applied directly to the lid and lashes of a closed eye to minimizing air trapping. [13] The clear plastic film is then applied directly to the closed eye taking care to avoid air trapping under the plastic film. The air between the skin and the plastic film will create an artifact and interfere with the exam. A copious amount of ultrasound gel should be applied on top of the plastic film with the goal of having enough gel so that the probe can rest lightly on top of the gel minimizing pressure on the eye. The provider’s hand should rest lightly on the bridge of the patient’s nose to stabilize the transducer, and the orbit should be assessed in both sagittal and transverse planes. With the probe horizontal the provider should scan the globe from top to bottom, and then with the probe stationary in the horizontal position the patient should look up and down continuously for several seconds. In the sagittal plane the globe should be scanned from right to left, and then the probe held stationary while the patient looks back and forth from right to left.
Complications
With the exclusion of possible damage in the setting of globe rupture, ocular ultrasound offers few risks to the patient and when done correctly, should not cause the patient significant discomfort.
Clinical Significance
Traditional methods of examining the deeper structures in the eye such as dilated fundoscopic and slit lamp examination can be difficult and require significant experience before providers feel proficient with these modalities. CT and MRI are noninvasive options which can be used to evaluate both the globe and orbit, but may be associated with radiation exposure, delays in care, and increased cost. [14] Conventional evaluation of intracranial pressure by emergency medicine physicians requires lumbar puncture which is time-consuming and presents risks to the patient. In many cases, ultrasound can provide an alternative to these tests and benefits include ease of use, low cost, lack of ionizing radiation, and ability to perform imaging at the bedside.
Enhancing Healthcare Team Outcomes
Ocular ultrasound is a valuable technique to determine many pathologies of the eye. However, if the patient has globe rupture, it is advisable to use another imaging technique to determine the problem. Overall, ocular ultrasound is safe, does not use contrast and can be performed at the bedside.
Media
References
Roque PJ, Hatch N, Barr L, Wu TS. Bedside ocular ultrasound. Critical care clinics. 2014 Apr:30(2):227-41, v. doi: 10.1016/j.ccc.2013.10.007. Epub 2013 Dec 12 [PubMed PMID: 24606775]
Kilker BA, Holst JM, Hoffmann B. Bedside ocular ultrasound in the emergency department. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 2014 Aug:21(4):246-53. doi: 10.1097/MEJ.0000000000000070. Epub [PubMed PMID: 24002686]
Woo MY, Hecht N, Hurley B, Stitt D, Thiruganasambandamoorthy V. Test characteristics of point-of-care ultrasonography for the diagnosis of acute posterior ocular pathology. Canadian journal of ophthalmology. Journal canadien d'ophtalmologie. 2016 Oct:51(5):336-341. doi: 10.1016/j.jcjo.2016.03.020. Epub 2016 Sep 3 [PubMed PMID: 27769323]
Chenkin J, Heslop CL, Atlin CR, Romano M, Jelic T. Bilateral Retinal Detachments Caused by Severe Preeclampsia Diagnosed with Point-of-Care Ultrasound. CJEM. 2016 Sep:18(5):395-8. doi: 10.1017/cem.2015.76. Epub 2015 Aug 19 [PubMed PMID: 26285683]
Shinar Z, Chan L, Orlinsky M. Use of ocular ultrasound for the evaluation of retinal detachment. The Journal of emergency medicine. 2011 Jan:40(1):53-7. doi: 10.1016/j.jemermed.2009.06.001. Epub 2009 Jul 21 [PubMed PMID: 19625159]
Frasure SE, Saul T, Lewiss RE. Bedside ultrasound diagnosis of vitreous hemorrhage and traumatic lens dislocation. The American journal of emergency medicine. 2013 Jun:31(6):1002.e1-2. doi: 10.1016/j.ajem.2013.02.013. Epub 2013 Apr 18 [PubMed PMID: 23602749]
Level 3 (low-level) evidenceRiccardi A, Siniscalchi C, Lerza R. Embolic Central Retinal Artery Occlusion Detected with Point-of-care Ultrasonography in the Emergency Department. The Journal of emergency medicine. 2016 Apr:50(4):e183-5. doi: 10.1016/j.jemermed.2015.12.022. Epub 2016 Feb 12 [PubMed PMID: 26879704]
Marchese RF, Mistry RD, Binenbaum G, Liu GT, Scarfone RJ, Woodford AL, Chen AE. Identification of Optic Nerve Swelling Using Point-of-Care Ocular Ultrasound in Children. Pediatric emergency care. 2018 Aug:34(8):531-536. doi: 10.1097/PEC.0000000000001046. Epub [PubMed PMID: 28146012]
Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2008 Feb:15(2):201-4. doi: 10.1111/j.1553-2712.2007.00031.x. Epub [PubMed PMID: 18275454]
Amini A, Kariman H, Arhami Dolatabadi A, Hatamabadi HR, Derakhshanfar H, Mansouri B, Safari S, Eqtesadi R. Use of the sonographic diameter of optic nerve sheath to estimate intracranial pressure. The American journal of emergency medicine. 2013 Jan:31(1):236-9. doi: 10.1016/j.ajem.2012.06.025. Epub 2012 Aug 31 [PubMed PMID: 22944553]
Xu W, Gerety P, Aleman T, Swanson J, Taylor J. Noninvasive methods of detecting increased intracranial pressure. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2016 Aug:32(8):1371-86. doi: 10.1007/s00381-016-3143-x. Epub 2016 Jun 28 [PubMed PMID: 27351182]
Abu-Zidan FM, Balac K, Bhatia CA. Surgeon-performed point-of-care ultrasound in severe eye trauma: Report of two cases. World journal of clinical cases. 2016 Oct 16:4(10):344-350 [PubMed PMID: 27803918]
Level 3 (low-level) evidenceEngelbert PR, Palma JK. Petroleum Jelly: A Novel Medium for Ocular Ultrasound. The Journal of emergency medicine. 2015 Aug:49(2):172-4. doi: 10.1016/j.jemermed.2015.03.003. Epub 2015 May 23 [PubMed PMID: 26014760]
Blaivas M, Theodoro D, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2002 Aug:9(8):791-9 [PubMed PMID: 12153883]