Introduction
The thyroid gland is a major endocrine organ that produces triiodothyronine (T3), tetraiodothyronine (T4), and calcitonin. These hormones are essential for bodily function and metabolism. This endocrine gland has a highly vascular blood supply due to its physiologic significance.
The superior thyroid artery (STA) arising from the external carotid artery (ECA), and the inferior thyroid artery (ITA) branching from the thyrocervical trunk create the blood supply to the thyroid gland. The STA and ITA anastomose bilaterally at the thyroid gland giving this organ a dual blood supply.
External Carotid artery branches: Superior thyroid artery, ascending pharyngeal artery, lingual artery, facial artery, occipital artery, posterior auricular artery, maxillary artery, superficial temporal artery.[1]
Thyrocervical Trunk branches: inferior thyroid artery, suprascapular artery, ascending cervical artery, transverse cervical artery.[2]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The thyroid has two lobes, a right and left connected by an isthmus. Besides the production of T3 and T4, the thyroid produces calcitonin. This hormone is made and secreted by the parafollicular cells or C-cells. Calcitonin ultimately opposes the parathyroid hormone produced by the parathyroid gland. Calcitonin decreases serum calcium concentration, while parathyroid hormone increases serum calcium concentration.
Embryology
The thyroid gland is the earliest endocrine organ to appear and derives from the endoderm, which migrates caudally from the floor of the pharynx during embryogenesis.[3]
Blood Supply and Lymphatics
The STA is the first branch off of the ECA arising from its anterior surface just inferior to the level of the greater cornu of the hyoid bone; it then branches into the infrahyoid artery, the superior laryngeal artery, and the cricothyroid artery and sternocleidomastoid artery.
- Infrahyoid artery: supplies the infrahyoid muscles
- Superior laryngeal artery: supplies mucous membranes, and muscles of the larynx
- Cricothyroid artery: supplies the cricothyroid muscle, isthmus, and pyramidal lobe (when present)
- Sternocleidomastoid artery: supplies the sternocleidomastoid muscle.
The ITA is the third branch of the thyrocervical trunk. The inferior thyroid artery is considered the principal blood supplier of the thyroid gland. The ITA gives rise to the ascending cervical artery, the inferior laryngeal artery, and also gives pharyngeal, tracheal, and esophageal branches. Also of importance, the ITA supplies the four parathyroid glands. Anatomical importance regarding the ITA is that it courses medially and posteriorly to the carotid sheath.
Ascending cervical artery: Supplies the neck, and gives off many small spinal arteries.
Inferior laryngeal artery: Supplies the larynx anastomosing with the superior laryngeal artery. This courses with the recurrent laryngeal nerve.[4]
Venous return from the thyroid is not as complicated as the arterial supply. The superior thyroid veins and middle thyroid veins drain into the internal jugular vein. The right and left inferior thyroid veins to drain into their respective brachiocephalic veins (right and left). The left internal jugular vein drains into the left subclavian vein to form the left brachiocephalic vein. The right internal jugular vein drains the right subclavian vein to form the right brachiocephalic vein. The right and left brachiocephalic veins coalesce to create the superior vena cava returning deoxygenated blood to the right atrium.
Nerves
The parasympathetic division of the autonomic nervous system is the primary innervation of the thyroid gland, via the vagus nerve (CNX). Remember, the vagus nerve does not stimulate, inhibit, nor control hormonal production or release.[5] Hematogenous feedback mechanisms are the mainstay of hormonal regulation, mainly through negative feedback inhibition.
Muscles
There are three categories of muscles concerning the thyroid and the larynx; internally for control of the vocal cords (speech production) as well as laryngeal inlet opening and closing, and extrinsic musculature.[6]
Physiologic Variants
The thyroid gland may have a pyramidal, which is a remnant of the thyroglossal duct from embryogenesis. The left lobe of the thyroid is the most common origin of the pyramidal lobe.[7]
Surgical Considerations
During a parathyroidectomy or thyroidectomy (total or partial), careful attention should be given to the arteries of the thyroid as well as coursing nerves. The recurrent laryngeal nerve, a branch of CN X courses with the inferior thyroid artery, while dissecting the ITA insult to the recurrent laryngeal nerve will cause the patient to go hoarse as this nerve innervates the larynx. Often during thyroidectomies, surgeons leave one parathyroid gland as not to cause the patient to become hypocalcemic.[8] As the inferior thyroid arteries mainly supply the parathyroid glands, accidental ligation can result in hypoparathyroidism.
If a patient presents with a nodule that needs a biopsy, it requires placement of an internal jugular central line needs to be placed, an ultrasound will guide these procedures to protect local neuro-vasculature damage and increase accuracy. On either side of the thyroid lies the carotid sheath, which encompasses the common carotid artery, internal carotid artery, vagus nerve, sympathetic plexus of nerves, and the internal jugular vein.[9]
Clinical Significance
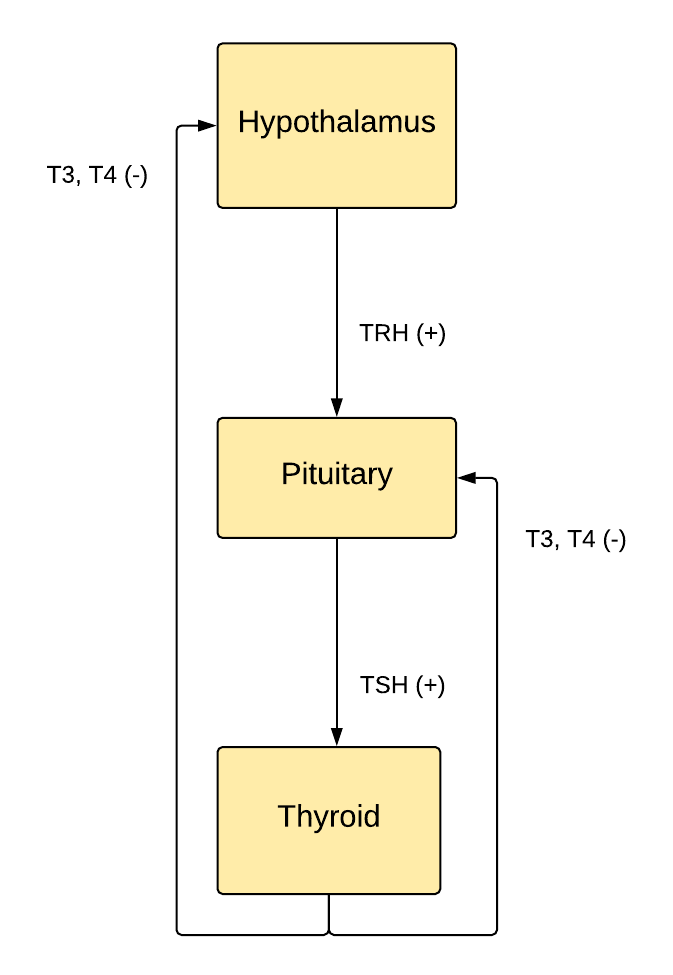
Thyroid releasing hormone (TRH) is released from the hypothalamus in response to low T3/T4, which stimulates the anterior pituitary gland to produce thyroid-stimulating hormone (TSH), where it is also stored. TSH stimulates the thyroid gland to produce T3 and T4, which creates a metabolic effect throughout the body (see below for examples of metabolic effects). T3 and T4 negatively feedback and inhibit the release of additional TRH and TSH from the hypothalamus and anterior pituitary, respectively. Meaning, increased T3/T4 in the blood normally inhibits the release of TRH and subsequently TSH.[10]
Hyperthyroidism: Diagnosed by a decreased TSH and increased T4. Objective findings on the exam would include but are not limited to tachycardia and hyperreflexia. Subjective findings, as described by the patient, would include palpitations, diarrhea, weight loss, anxiety, and heat intolerance.[11]
Hypothyroidism: Diagnosed by the presence of increased TSH and decreased T4. Objective findings on the exam would include but are not limited to bradycardia, decreased deep tendon reflexes, and a lethargic appearing patient. Subjective findings, as described by the patient, would include constipation, weight gain, fatigue, cold intolerance, and hair loss.[12]
The findings listed above are not an all-inclusive list but rather signs and symptoms most often found and reported.
Other Issues
There are various issues with the thyroid: toxic adenoma, goiter, hyperthyroidism, hypothyroidism, and malignancy. This list is not all-inclusive.
Ectopic thyroid tissue may be present in the tumor stroma ovarii, which occurs in the ovary. Another site of ectopic thyroid tissue is at the tongue termed lingual thyroid.
Multiple endocrine neoplasia (MEN) is also of significance with three (3) types. MEN 1 (Wermer syndrome), MEN 2A, MEN 2B.[13][14]
MEN1: Autosomal dominant, associated with the 3 Ps of parathyroid, pituitary gland abnormalities, and pancreatic islet cell tumors (insulinoma, glucagonoma, VIPoma, and gastrinoma)
MEN2A: RET mutation, associated with parathyroid, medullary thyroid carcinoma, and pheochromocytoma.
MEN2B: RET mutation, associated with parathyroid, medullary thyroid carcinoma, pheochromocytoma, and mucosal neuromas.
Graves disease is a primary cause of hyperthyroidism and is diagnosed by an elevated T4 and decreased TSH but, more specifically, antibodies against thyroid-stimulating immunoglobulin, also known as TRAb.[15]
Hashimoto thyroiditis is a primary cause of hypothyroidism and is diagnosed by a decreased T4 and elevated TSH with antibodies against thyroperoxidase (TPO).[16]
Media
(Click Image to Enlarge)
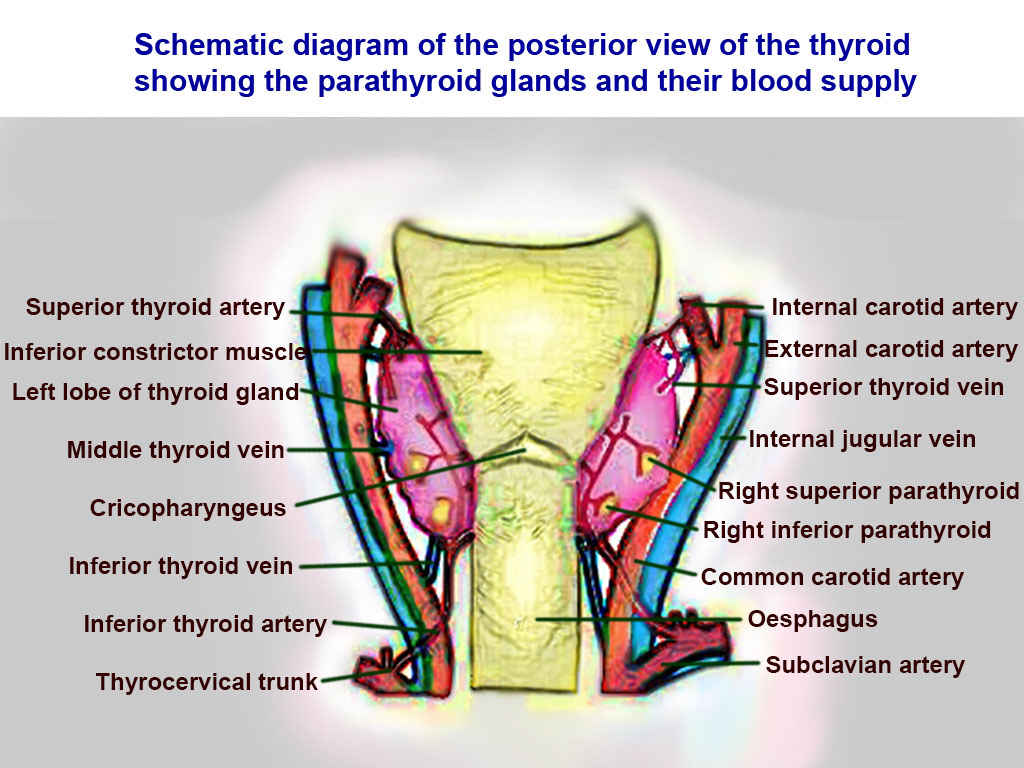
Thyroid Arteries, Veins, and Muscles. Posterior view of thyroid includes superior thyroid, inferior constrictor, left lobe of thyroid, middle thyroid vein, cricopharyngeaus, inferior thyroid vein, inferior thyroid vein, inferior thyroid artery, thyrocervical trunk, internal carotid, external carotid, superior thyroid, internal jugular, right superior parathyroid, right inferior parathyroid, common carotid, oesphagus, and subclavian.
Contributed by T Silappathikaram
(Click Image to Enlarge)
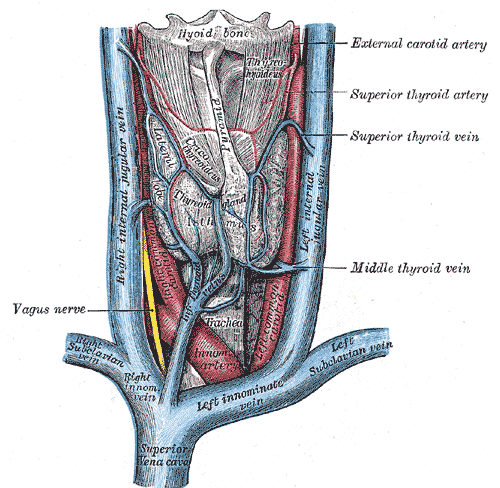
Veins and Arteries of the Neck. Superior vena cava, left and right innominate vein, left and right subclavian vein, left and right internal jugular vein, innominate arteries, hyoid bone, thyroid gland, and trachea.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
References
Charlick M, M Das J. Anatomy, Head and Neck: Internal Carotid Arteries. StatPearls. 2023 Jan:(): [PubMed PMID: 32310521]
Jardaly AH, Bordoni B. Anatomy, Thorax, Thyrocervical Arteries. StatPearls. 2025 Jan:(): [PubMed PMID: 32310456]
Miles B, Srinivasan VN. Embryology, Pharyngeal Pouch. StatPearls. 2023 Jan:(): [PubMed PMID: 32491656]
Noordzij JP, Ossoff RH. Anatomy and physiology of the larynx. Otolaryngologic clinics of North America. 2006 Feb:39(1):1-10 [PubMed PMID: 16469651]
Roman BR, Randolph GW, Kamani D. Conventional Thyroidectomy in the Treatment of Primary Thyroid Cancer. Endocrinology and metabolism clinics of North America. 2019 Mar:48(1):125-141. doi: 10.1016/j.ecl.2018.11.003. Epub [PubMed PMID: 30717897]
Jacobsen B, VanKampen N, Ashurst JV. Anatomy, Head and Neck, Thyrohyoid Membrane. StatPearls. 2023 Jan:(): [PubMed PMID: 30422588]
Gurleyik E, Gurleyik G, Dogan S, Cobek U, Cetin F, Onsal U. Pyramidal Lobe of the Thyroid Gland: Surgical Anatomy in Patients Undergoing Total Thyroidectomy. Anatomy research international. 2015:2015():384148. doi: 10.1155/2015/384148. Epub 2015 Jul 7 [PubMed PMID: 26236507]
Lončar I, Dulfer RR, Massolt ET, Timman R, de Rijke YB, Franssen GJH, Burger PJWA, Smit C, van der Horst FAL, Peeters RP, van Eijck CHJ, van Ginhoven TM. Postoperative parathyroid hormone levels as a predictor for persistent hypoparathyroidism. European journal of endocrinology. 2020 Aug:183(2):149-159. doi: 10.1530/EJE-20-0116. Epub [PubMed PMID: 32580147]
Miyake N, Hayashi S, Kawase T, Cho BH, Murakami G, Fujimiya M, Kitano H. Fetal anatomy of the human carotid sheath and structures in and around it. Anatomical record (Hoboken, N.J. : 2007). 2010 Mar:293(3):438-45. doi: 10.1002/ar.21089. Epub [PubMed PMID: 20169562]
Brent GA. Mechanisms of thyroid hormone action. The Journal of clinical investigation. 2012 Sep:122(9):3035-43. doi: 10.1172/JCI60047. Epub 2012 Sep 4 [PubMed PMID: 22945636]
Level 3 (low-level) evidenceDavis JR, Dackiw AP, Holt SA, Nwariaku FE, Oltmann SC. Rapid Relief: Thyroidectomy is a Quicker Cure than Radioactive Iodine Ablation (RAI) in Patients with Hyperthyroidism. World journal of surgery. 2019 Mar:43(3):812-817. doi: 10.1007/s00268-018-4864-7. Epub [PubMed PMID: 30483883]
Merson J. Hypothyroidism. JAAPA : official journal of the American Academy of Physician Assistants. 2018 Dec:31(12):43-44. doi: 10.1097/01.JAA.0000547758.46299.d9. Epub [PubMed PMID: 30489390]
Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, Pieterman CRC, van Leeuwaarde RS, van den Broek MFM, van Nesselrooij BPM, Valk GD. Multiple Endocrine Neoplasia Type 1. Endotext. 2000:(): [PubMed PMID: 29465925]
Raue F, Frank-Raue K, Grauer A. Multiple endocrine neoplasia type 2. Clinical features and screening. Endocrinology and metabolism clinics of North America. 1994 Mar:23(1):137-56 [PubMed PMID: 7913021]
Kotwal A, Stan M. Thyrotropin Receptor Antibodies-An Overview. Ophthalmic plastic and reconstructive surgery. 2018 Jul/Aug:34(4S Suppl 1):S20-S27. doi: 10.1097/IOP.0000000000001052. Epub [PubMed PMID: 29771756]
Level 3 (low-level) evidenceWilliams DE, Le SN, Godlewska M, Hoke DE, Buckle AM. Thyroid Peroxidase as an Autoantigen in Hashimoto's Disease: Structure, Function, and Antigenicity. Hormone and metabolic research = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 2018 Dec:50(12):908-921. doi: 10.1055/a-0717-5514. Epub 2018 Oct 25 [PubMed PMID: 30360003]