Introduction
A bronchoscopy is an essential tool for clinicians and health care providers treating patients with lung diseases. [1][2]Since its introduction to clinical practice by Shigeto Ikeda in 1966, flexible bronchoscopy has become an essential tool in diagnosis and management of patients with lung diseases. Rigid bronchoscopy can be particularly helpful in therapeutic cases.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
A flexible bronchoscope, equipped with fiber optics, camera, and light source, allows for real-time, direct visualization of the airways. [3][4]It can be used to examine the respiratory tract starting from the oral or nasal cavity to the sub-segmental bronchi. Advanced bronchoscopic techniques such as endobronchial ultrasound enable ultrasonographic evaluation of mediastinal structures such as lymph nodes, as well as the periphery of the lung.
Indications
Diagnostic Indications
Hemoptysis, chronic unexplained cough, stridor, mediastinal or hilar lymphadenopathy, nodal staging of lung cancer, pulmonary infiltrates, pneumonia, atelectasis, suspected tracheomalacia, tracheoesophageal fistula, and post lung transplant surveillance.[3][5]
Therapeutic Indications
Foreign body retrieval, tracheal and bronchial stent placement balloon dilatation of airway stenosis, ablation or debulking of endobronchial tumors, management of persistent air leak or bronchopleural fistula, difficult intubations, bronchoscopic lung volume reduction surgery, bronchial thermoplasty for asthma, whole lung lavage, and as an adjunct during percutaneous tracheotomy.[6] Bronchoscopy is a good temporizing modality for hemoptysis by isolating the bleeding lung using bronchial blocker, however, the therapeutic yield is poor.
Diseases for Which Bronchoscopy Is Not the Optimal Diagnostic or Therapeutic Tool
There are diseases in which bronchoscopy is commonly done, however, the diagnostic and therapeutic yield is poor. Deshwal et al have grouped these into the following categories[7]
1. Infectious causes:
- Cystic fibrosis
- Smear negative pulmonary tuberculosis
2. Hemoptysis
3. Radiological findings
- Atelectasis in a patient on mechanical ventilation
- fibrosing mediastinitis
- Pleural effusion
4. Mediastinal lymphadenopathy from the following causes
- Idiopathic pulmonary fibrosis
- Stage 1 Sarcoidosis
- Congestive lymphadenopathy
- Calcified lymphadenopathy
- Lymphoma
- COPD exacerbation and lymphadenopathy
Contraindications
Bronchoscopy should not be performed when risks of the procedure outweigh the benefits. Risk-benefit assessment is undertaken on a case-by-case basis by the treating pulmonologist. Contraindications may include, but not limited to, severe baseline hypoxia, hemodynamic instability, recent myocardial infarction, severe hypoxia, uncooperative patient, severe bleeding disorder or an inexperienced operator.
Equipment
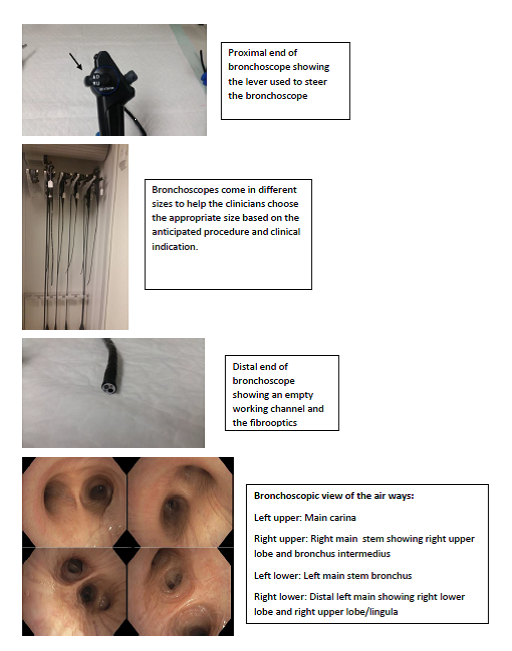
The flexible bronchoscope consisting of fiber optic bundles, camera, and working channel, is connected to a light source and image processor, which displays the transmitted images on a monitor. The bronchoscope can be steered to view the airways by the use of a lever at the proximal end of the bronchoscope. Flexible bronchoscopes come in different sizes and varying working channel diameters. This variety allows for appropriate selection of bronchoscope for a given clinical scenario. Standard diagnostic tools such as biopsy forceps, an aspiration needle, and bronchial brush are used to obtain tissue samples. Therapeutic tools such as balloons, laser fiber argon plasma coagulation catheter and ,electrocautery and cryotherapy probes can also be used through a flexible bronchoscope. Advances in bronchoscopy include endobronchial ultrasound, radial probe ultrasound, confocal endomicroscopy, narrow band imaging, autofluorescence, and electromagnetic navigational bronchoscopy.
Preparation
Informed consent should be obtained from the patient or the patient’s health care power of attorney. A focused history and physical examination should be obtained to ensure the procedure is clinically indicated and to evaluate for potential contraindications. The patient should fast (nothing by mouth) for six to eight hours before the procedure. Hemodynamic monitoring, pulse oximetry, and intravenous access should be assured before the start of the procedure. Patient’s medication list and allergies, and laboratory results should always be checked. An ECG may be performed if clinically indicated. A ‘time out’ is performed at the start of the procedure. Although bronchoscopy can be done without sedation, most procedures are done under moderate conscious sedation with the use of various sedatives based on the clinician’s preference (e.g., benzodiazepines, opioids, dexmedetomidine). Certain procedures may require more deep sedation or general anesthesia. Regardless of the sedation or anesthesia used the physicians should be aware of the potential side effects and how to manage patients receiving these medications.
Technique or Treatment
The bronchoscope may be introduced into the nasal cavity or the mouth (or through an endotracheal tube or laryngeal mask airway) and advanced to the level of the vocal cords. Assessment of the appearance and movement of the cords is done. As the bronchoscope is advanced beyond the vocal cords, a careful inspection of the entire airway is performed. In particular, abnormal endobronchial lesions or mucosal abnormalities, as well as any evidence of narrowing or dynamic collapse, is assessed. Pictures or videos can be recorded for future reference. Effort should be made to avoid unnecessary contact with the mucosa to avoid trauma. Based on the indication of the procedure, appropriate tools are selected to accomplish specific tasks such as tissue sampling or tumor debulking. At the conclusion of the procedure, a final assessment of the airway should be performed ensure adequate hemostasis. A post-procedural chest x-ray may be needed to evaluate for the presence of a pneumothorax. All patients should be monitored before, during and after the procedure. After uneventful recovery and in the absence of complications the patient may be discharged on the same day. Appropriate follow up is scheduled, and the patient is advised not to drive, operate heavy machinery for the rest of the day, or participate in any activity that requires full consciousness as the effect of the medications may last many hours.
Complications
Medication-related complications:[8][9]
- An overdose of local anesthetics can result in central nervous system (CNS)-toxicity like neuropathy, seizures, and coma.
- Methemoglobinemia
- Most sedative medications can result in hemodynamic effects including low blood pressure or low heart rate.
- General anesthetics may result in malignant hyperthermia and prolonged neuromuscular paralysis.
Procedure-related complications:
- Bleeding: In most cases, bleeding is usually self-limited. The pulmonologists should carefully ascertain for hemostasis, and in the event of severe bleeding prompt management should be immediately instituted.
- Pneumothorax: In 1% to 3% of patients, pneumothorax may occur after transbronchial biopsies. Small pneumothoraces may be managed conservatively, while symptomatic and large pneumothorax will require chest tube insertion and hospitalization. A tension pneumothorax results in hemodynamic instability and should be recognized even without imaging studies. Appropriate life-saving measures such as chest tube insertion should be undertaken immediately. Most pneumothoraces after bronchoscopy develop within the first hour of the procedure but can be delayed up to 24 hours. Appropriate instructions to the patient and appropriate follow up should be arranged.
- Cardiac arrhythmias may also occur especially in patients with pre-existing cardiac disease.
- Other potential complications of the procedure include trauma to the vocal cords, pneumomediastinum, hypoxia, and rarely death.
Clinical Significance
Bronchoscopy is helpful in the diagnosis and management of various airway and lung diseases. With further advances in technology, a bronchoscopy will not only continue its current role in clinical practice but will expand its scope as a minimally invasive advanced diagnostic and therapeutic tool.
Enhancing Healthcare Team Outcomes
an interprofessional team skilled in the care of patients with airways and lung disease and adept in the use of bronchoscopy equipment is essential to performing bronchoscopy safely and manage complications. In addition to a skilled bronchoscopist, personnel includes an endoscopy nurse and respiratory therapist or technician trained in the use of bronchoscopy equipment. If general anesthesia is used for the procedure, additional personnel include anesthesiologist and/or nurse anesthetist. Many bronchoscopy suites also use rapid on-site cytologic evaluation of specimens by a pathologist or cytology technician.[10][11][12]
Media
(Click Image to Enlarge)
References
Ninan N, Wahidi MM. Basic Bronchoscopy: Technology, Techniques, and Professional Fees. Chest. 2019 May:155(5):1067-1074. doi: 10.1016/j.chest.2019.02.009. Epub 2019 Feb 16 [PubMed PMID: 30779915]
Sakpal SV, Donahue S, Crespo HS, Auvenshine C, Agarwal SK, Nazir J, Santella RN, Steers J. Utility of fiber-optic bronchoscopy in pulmonary infections among abdominal solid-organ transplant patients: A comprehensive review. Respiratory medicine. 2019 Jan:146():81-86. doi: 10.1016/j.rmed.2018.12.002. Epub 2018 Dec 12 [PubMed PMID: 30665523]
Biswas A, Mehta HJ, Sriram PS. Diagnostic Yield of the Virtual Bronchoscopic Navigation System Guided Sampling of Peripheral Lung Lesions using Ultrathin Bronchoscope and Protected Bronchial Brush. Turkish thoracic journal. 2019 Jan 1:20(1):6-11. doi: 10.5152/TurkThoracJ.2018.18030. Epub 2019 Jan 1 [PubMed PMID: 30664420]
O'Shea C, Khan KA, Tugwell J, Cantillon-Murphy P, Kennedy MP. Loss of flexion during bronchoscopy: a physical experiment and case study of commercially available systems. Lung cancer management. 2017 Dec:6(3):109-118. doi: 10.2217/lmt-2017-0012. Epub 2017 Dec 1 [PubMed PMID: 30643576]
Level 3 (low-level) evidenceMohan A, Harris K, Bowling MR, Brown C, Hohenforst-Schmidt W. Therapeutic bronchoscopy in the era of genotype directed lung cancer management. Journal of thoracic disease. 2018 Nov:10(11):6298-6309. doi: 10.21037/jtd.2018.08.14. Epub [PubMed PMID: 30622805]
Gendeh BS, Gendeh HS, Purnima S, Comoretto RI, Gregori D, Gulati A. Inhaled Foreign Body Impaction: A Review of Literature in Malaysian Children. Indian journal of pediatrics. 2019 Jan:86(Suppl 1):20-24. doi: 10.1007/s12098-018-2824-8. Epub 2019 Jan 9 [PubMed PMID: 30623311]
Deshwal H, Avasarala SK, Ghosh S, Mehta AC. Forbearance With Bronchoscopy: A Review of Gratuitous Indications. Chest. 2019 Apr:155(4):834-847. doi: 10.1016/j.chest.2018.08.1035. Epub 2018 Aug 29 [PubMed PMID: 30171862]
Choo R, Naser NSH, Nadkarni NV, Anantham D. Utility of bronchoalveolar lavage in the management of immunocompromised patients presenting with lung infiltrates. BMC pulmonary medicine. 2019 Feb 26:19(1):51. doi: 10.1186/s12890-019-0801-2. Epub 2019 Feb 26 [PubMed PMID: 30808314]
Agarwal S, Hoda W, Mittal S, Madan K, Hadda V, Mohan A, Bharti SJ. Anesthesia and anesthesiologist concerns for bronchial thermoplasty. Saudi journal of anaesthesia. 2019 Jan-Mar:13(1):78-80. doi: 10.4103/sja.SJA_640_18. Epub [PubMed PMID: 30692896]
Jakubczyc A, Neurohr C. [Diagnosis and Treatment of Interstitial Lung Diseases]. Deutsche medizinische Wochenschrift (1946). 2018 Dec:143(24):1774-1777. doi: 10.1055/a-0622-9299. Epub 2018 Dec 3 [PubMed PMID: 30508858]
Krishnan S, Kniese CM, Mankins M, Heitkamp DE, Sheski FD, Kesler KA. Management of broncholithiasis. Journal of thoracic disease. 2018 Oct:10(Suppl 28):S3419-S3427. doi: 10.21037/jtd.2018.07.15. Epub [PubMed PMID: 30505529]
Thakkar HS, Hewitt R, Cross K, Hannon E, De Bie F, Blackburn S, Eaton S, McLaren CA, Roebuck DJ, Elliott MJ, Curry JI, Muthialu N, De Coppi P. The multi-disciplinary management of complex congenital and acquired tracheo-oesophageal fistulae. Pediatric surgery international. 2019 Jan:35(1):97-105. doi: 10.1007/s00383-018-4380-8. Epub 2018 Nov 3 [PubMed PMID: 30392126]