Anteroinferior Glenoid Labrum Lesion (Bankart Lesion)
Anteroinferior Glenoid Labrum Lesion (Bankart Lesion)
Introduction
The glenoid labrum is a fibrocartilaginous ring attached circumferentially to the glenoid rim contributing to the stability of the shoulder joint.[1] The glenoid labrum increases the glenoid surface vertically by 75% and horizontally by 57%, according to Saha et al.[2] Bankart's lesion represents an anterior and inferior labral detachment from the glenoid with an associated capsuloligamentous injury below the equator of the glenoid.[3] This result in anterior instability of the shoulder joint due to the loss of the following normal mechanisms, such as the choke block effect of the labrum, concavity compression mechanism of the rotator cuff, and function of the inferior glenohumeral ligament.[4] Traumatic subluxations or dislocations of the shoulder joint cause injury to the glenoid labrum.[5] Almost 87 to 100% of the index anterior shoulder dislocations are associated with Bankart lesions.[6]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Lesions of the glenoid labrum are most commonly the result of traumatic shoulder dislocation.[7] The most common cause of traumatic shoulder dislocation is participation in collision or contact sports.[8] Primary or recurrent shoulder dislocations result in varying degrees of injury to the glenoid labrum, such as Bankart lesion, SLAP (Superior Labral lesion Anterior to Posterior) lesion, ALPSA (Anterior Labral Periosteal Sleeve Avulsion) lesion, and HAGL (Humeral Avulsion of Glenohumeral Ligament) lesion. Bankart lesion is specifically caused by anterior shoulder dislocation with the shoulder in external rotation and abduction.[9]
Abnormal translation of the head of the humerus during dislocation results in excessive loading and stretching of the labrum and capsuloligamentous structures. This excessive stretch leads to a tear or avulsion of the labrum with associated capsular injury.[10]
Epidemiology
Shoulder dislocations occur in 1% of the population, most of which are anterior (90%).[11] Traumatic dislocations are the leading cause of shoulder injuries.[12] Most dislocations (95%) are traumatic and occur three times more often in men.[13] In young athletes, the recurrence rate is over 90% if not treated surgically.[12]
An anterior shoulder dislocation is associated with a Bankart lesion in 87 to 100%, a Hill-Sachs lesion in 90%, a bony Bankart lesion in 73%, a rotator cuff injury in 13%, and a SLAP (Superior Labral lesion Anterior to Posterior) in 10%.[14][15][16] Perthes lesion, Anterior Labral Periosteal Sleeve Avulsion (ALPSA), Gleno-Labral Articular Disruption (GLAD), and Humeral avulsion of Glenohumeral Ligament (HAGL) occur in a minority of patients.[16][17]
Pathophysiology
Traumatic anterior shoulder dislocation results in various injuries to the shoulder joint (glenohumeral joint). Soft tissue injuries, such as glenoid labrum tears, capsular tears, glenohumeral ligaments, and rotator cuff injuries, may occur.[18] The bony injuries may involve the glenoid rim or the humeral head.[14] The soft tissue Bankart lesion is an injury to the anteroinferior glenoid labrum and capsule-ligament complex. It is a pure soft-tissue injury. Bankart lesion is caused explicitly by anterior shoulder dislocation with the shoulder in external rotation and abduction.[9]
Abnormal translation of the head of the humerus during dislocation results in excessive loading and stretching of the labrum and capsuloligamentous structures.[10] This excessive stretch leads to a tear or avulsion of the labrum with associated capsular injury. In contrast, the bony Bankart lesion is an avulsion fracture of the glenoid rim with anteroinferior glenoid labrum and capsuloligamentous complex injury.[19] Bone loss alters the shape of the glenoid cavity as an inverted pear, and this will reduce the glenoid articular arc.[20]
Burkhart studied the effect of a change in shape and reduced surface area of the glenoid on recurrence. The recurrence rate was higher in the groups with significant bone loss at the glenoid.[20] Hill-Sachs lesion is a posterosuperior osteochondral impaction fracture of the humeral head.[21] There are two types of Hill-Sachs lesions: one interlocked with the glenoid rim and one not interlocked when the shoulder is in a functional position (abduction and external rotation). They are referred to as "engaging" and "non-engaging," respectively.[4]
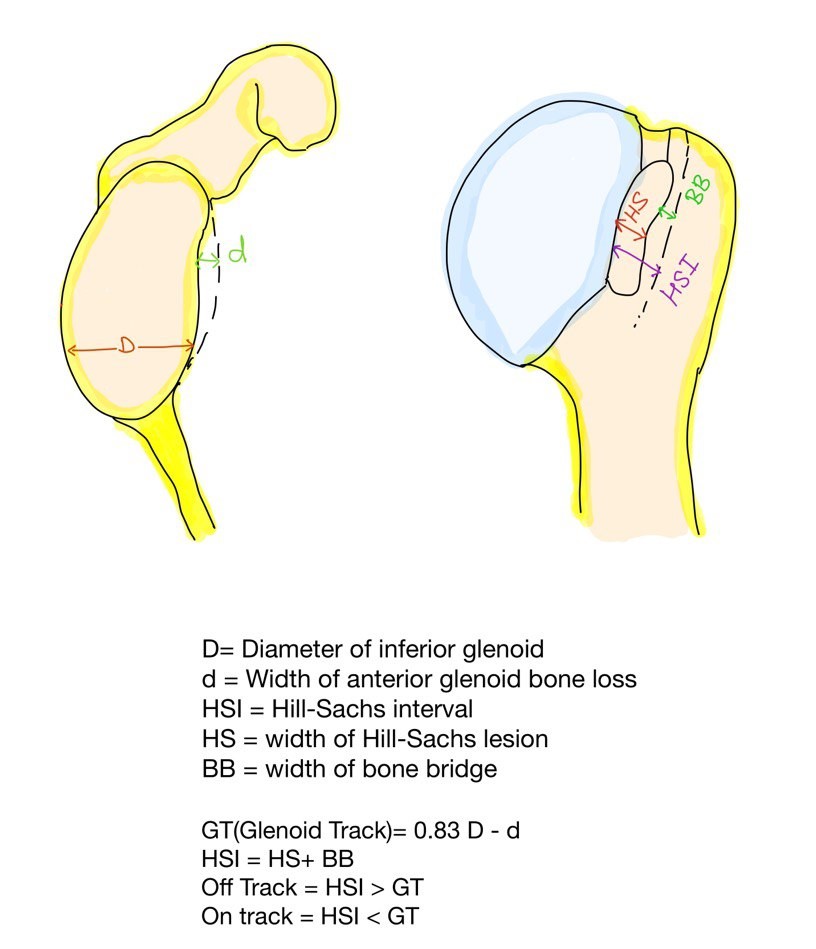
In engaging Hill Sachs, the long axis of the bone defect is parallel to the anterior glenoid rim; hence it will engage with the glenoid rim.[14] The bone defect of the non-engaging- Hill Sachs is diagonal or not parallel to the anterior glenoid margin, so there is no engagement of the humeral head with the glenoid margin in functional positions, but engagement may occur in non-functional positions such as an extension or low abduction (<70 degrees).[14] The non-engaging variant is the most common, but an engaging Hill-Sachs causes the most recurrences.[14][22] Recently, Giovanni et al. proposed the concept of a glenoid track (on-track and off-track lesions).[14] According to this concept, "off-track" lesions usually engage even after soft tissue repair.[23]
History and Physical
Glenoid labral lesions present with signs and symptoms of recurrent shoulder instability with generalized shoulder pain.[5] A few patients may present with catching, locking, or popping sensations in the shoulder.[24] Most patients with a Bankart lesion report primary or recurrent anterior shoulder dislocation.
History
Evaluation of the Bankart’s lesion requires a thorough history, including the index dislocation, number of dislocations or subluxations, and their reduction method (self or medical personnel). Clinicians must enquire about the patient’s occupation, involvement in the contact sport, mechanism of trauma, and history of the epileptic disorder.[25] The history of a dislocation includes the following key points –
- Demographic details
- Occupation
- Level of activity- contact sport, recreational, none
- Index dislocation
- Age at first dislocation
- Number of dislocations/subluxations
- Mechanism of dislocation
- Presence of associated injury
- Reduction of dislocation- self or medical person
- Dislocation in sleep
- History of epileptic disorder
Examination
Clinical examination is dedicated to diagnosing the presence of shoulder instability and associated injuries.
Signs of Anterior Instability
- Apprehension test – [Specificity-96%, Sensitivity-72%]
- Jobe’s relocation test - [Specificity-92%, Sensitivity-81%]
- Anterior drawer test - [Specificity-85%, Sensitivity-53%]
- Bony apprehension test - [Specificity-86%, Sensitivity-100%][26][27]
Signs of Posterior Instability
- Posterior apprehension- [Specificity-99%, Sensitivity-20%][28]
- Jerk test- [Specificity-98%, Sensitivity-73%]
- Porcellini test- [Specificity-99.3%, Sensitivity-100%][29]
- Kim test- [Specificity- 94%, Sensitivity- 80%][30]
Signs of Mid-range Instability
- Sulcus sign rules out multidirectional instability. [Specificity-97%, Sensitivity-28%][31]
Generalized Ligamentous Laxity
- Beighton score[32]
Evaluation
Investigations
Radiographs - It is important to obtain plain radiographs as part of the initial workup to rule out associated fractures and frank osseous defects such as bony Bankart, Hill-Sachs, glenoid fractures, coracoid fractures, and greater tuberosity fractures.[33]
- Anteroposterior view (AP view)
- True AP view
- Axillary view
- Scapular Y view
- Acromial outlet view
Special views[33]
- West point axillary view- Bony Bankart's lesion
- Stryker's notch view – Hill-Sachs lesion
Magnetic Resonance Imaging (MRI)
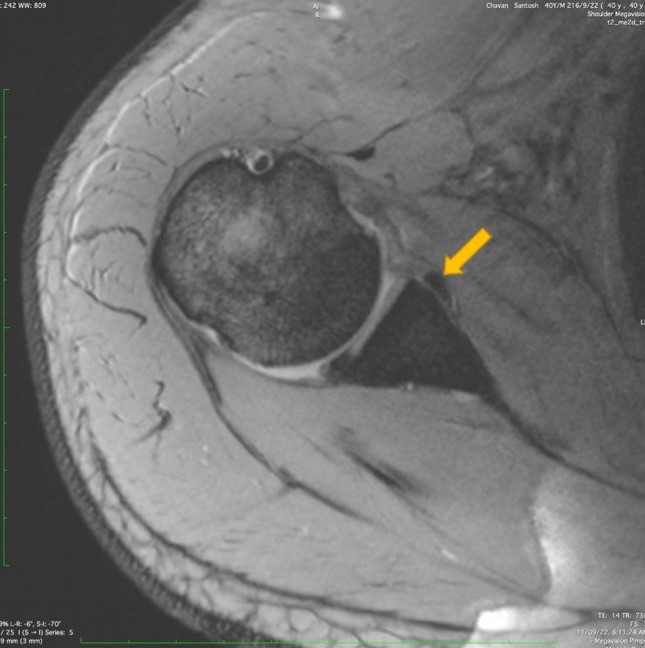
MRI with or without contrast is the gold standard investigation for soft tissue injuries such as glenoid labrum and capsuloligamentous injury. It also helps in planning the management of shoulder instability. MRI findings will be hemorrhagic effusion and capsulolabral elevation from the anterior and inferior glenoid rim in an acute Bankart injury. MRI in the abduction and External rotation has improved sensitivity (94%) and specificity (82%) for detecting Bankart lesions than the traditional neutral position. Presence of associated lesions such as Perthe's lesion, Anterior Labral Periosteal Sleeve Avulsion (ALPSA), Gleno-Labral Articular Disruption (GLAD), and Superior Labral tear from Anterior to Posterior (SLAP), and Humeral avulsion of Glenohumeral Ligament (HAGL) can be diagnosed on MRI.[34]
MR-arthrogram is more specific and sensitive than MRI for detecting labral tears. The specificity and sensitivity are 96% and 93 %, respectively.[24]
Non- Contrast Computed Tomography (NCCT) with 3D reconstruction - This investigation is very useful in quantifying the glenoid bone loss, the orientation of the articular surface, humeral bone loss, and the glenoid version.
Following are the indications for NCCT with 3D reconstruction[35]
- Mid-range instability on clinical examination.
- Glenoid bone loss suspicion on the radiograph.
- Large Hill-Sachs.
- A very large number of shoulder dislocations.
- Identification of "On Track" and "Off Track" Hill-Sachs lesion.
Measurements of glenoid and humeral bone loss on 3D reconstruction[14][19]
- GT = 83% (D – d)
- HSI = HS + BB
On Track = HSI < GT
Off Track = HSI > GT
Abbreviations
- GT - glenoid track.
- D – Diameter of inferior glenoid.
- d- Width of anterior glenoid bone loss.
- HSI- Hill-Sachs Interval.
- HS- width of Hill-Sachs lesion.
- BB- Width of Bone Bridge (distance of the lateral edge of Hill-Sachs from the medial edge of rotator cuff insertion).
Treatment / Management
Factors that determine the treatment of Bankart repair are:
- Age of the patient
- Level of physical activity
- Desired future activity level
- History of shoulder pain
- Recurrent shoulder instability
- Associated glenoid or humerus bone loss[23]
Conservative Management
The best candidates for nonoperative management are patients older than 30 with no obvious shoulder instability, preserved normal osseous restrain to instability, and no desire to participate in recreational activities. Patients with multidirectional instability (MDI), voluntary dislocators, and minimal demand are further prospects for nonoperative therapy.[36](A1)
Operative Management
Indications for operative management- Young athletes (less than 30 years of age) with acute, primary, and traumatic anterior shoulder dislocations who wish to continue playing sports are the best candidates for surgical intervention.[37][38] Other indications are as follows-
- Post-traumatic recurrent shoulder instability limiting daily activities
- Post-traumatic anterior shoulder dislocation with an associated large rotator cuff tear, bony defect in the glenoid or the humerus head (Hill Sachs lesion)
- Persistent subluxation and pain even after adequate nonoperative management.
- Patients with a propensity for recurrent instability include athletes with overhead activities, construction workers, and climbers.
Relative Contraindications for Operative Management
- Uncooperative/ medically unstable patients
- Seizure disorder
- Primary collagen disorders, such as (Ehlers- Danlos or Marfan syndrome)
- Atraumatic shoulder instability
- A neurologic injury such as paralysis of the axillary nerve or suprascapular nerve
- Recurrent instability with post-traumatic arthritis[38]
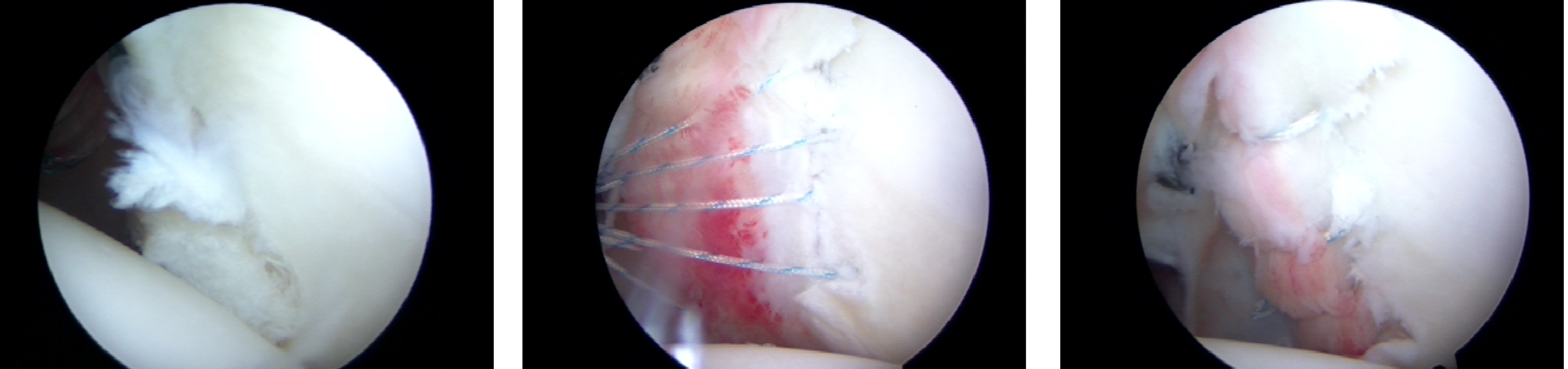
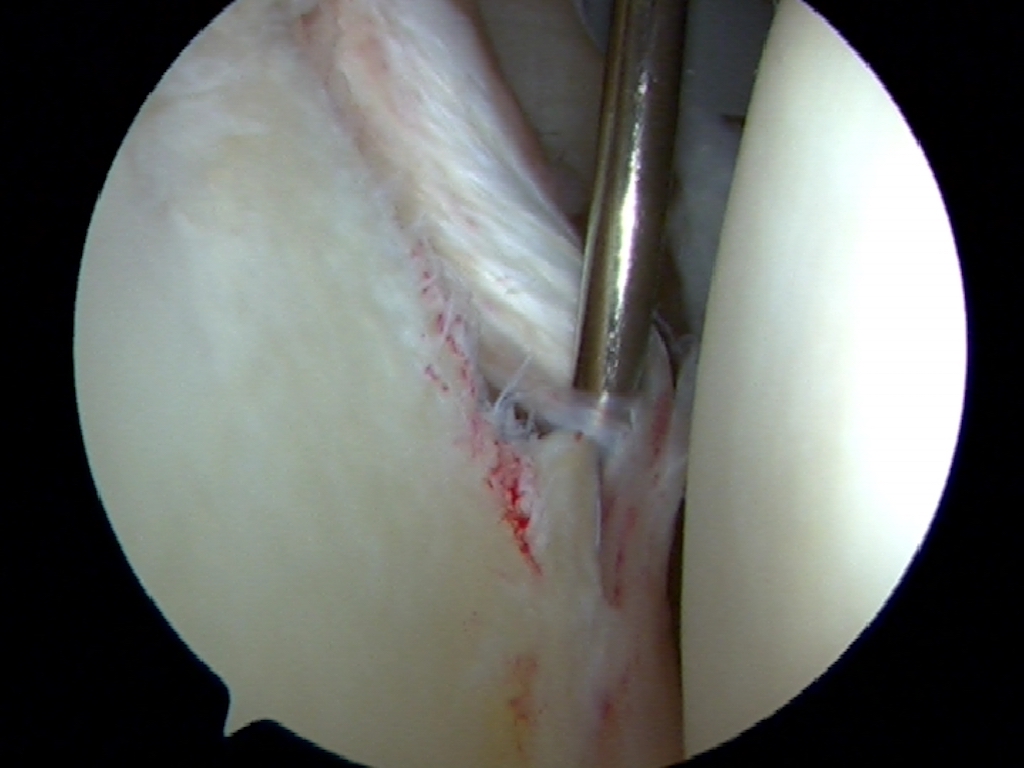
Deciding the Surgery - The patient's expectations, age, and level of the sport (contact vs. non-contact) are the most crucial factors to consider when treating a labral injury.[39] If the patient is young and involved in contact sports (high demand), they will be considered for surgery.[40] The glenoid bone loss and engaging (off track)/non-engaging (on track) Hill Sachs lesions are assessed in all of these patients.[23] If the glenoid bone loss is less than 13.5%, isolated arthroscopic or open Bankart's repair with suture anchors will be sufficient.[41][42] This non-significant bone loss will not engage in almost all cases [23]. The glenoid bone loss of 13.5% to 17.3% is subcritical; in such cases risk of recurrence is taken into consideration, and high-risk patients (young athletes from contact sports, and the presence of engaging Hill-Sachs lesion) will be treated with arthroscopic or open Bankart's repair with remplissage.[42][43] (A1)
When glenoid bone loss is 13.5% to 17.3% with a low risk of recurrence and is non-engaging, Hill Sachs patients are treated by isolated arthroscopic or open Bankart's repair.[44][45] Patients with 17.4% to 30% glenoid bone loss will need an open Latarjet procedure.[46] About 30% or more, glenoid bone loss mandates glenoid bone grafting (autograft- iliac crest or allograft-distal tibia allograft).[47]
Differential Diagnosis
Anterior Labrum Periosteal Sleeve Avulsion Lesion (ALPSA)
It is an anteroinferior glenoid labrum and capsuloligamentous avulsion with intact scapular periosteum. This lesion will heal at the nonanatomic position and presents as anterior shoulder instability.[48]
Perthes Lesion
The avulsion of the anteroinferior glenoid labrum from the glenoid rim but partially attached with the intact scapular periosteum. As a result, the avulsed labrum is present in an anatomical position but is nonfunctional. Hence, the patient will present with anterior shoulder instability.[49]
Prognosis
Surgical stabilization of anteroinferior glenoid labral lesions with arthroscopic or open procedures yields impressive results.[49] Arthroscopic procedures propose theoretical advantages of anatomical restoration of the glenoid labrum, selective soft tissue tensioning, improved range of motion, less post-operative pain, and preservation of subscapularis muscle over an open approach. Functional outcomes of the shoulder and return to the same level of sport are better with arthroscopically treated Bankart lesions.[38]
The rate of return to the same level of sport after arthroscopically treated Bankart is 71% and 66% after the open procedure.[50]
Complications
Perioperative Complications
- Anchor failure
- Glenoid fracture
- Nerve injury (0.3%) - musculocutaneous or axillary nerve injury
- Hematoma formation
- Infection (0.2%)[50]
Postoperative Complications
Arthroscopic Bankart Repair
Recurrence - Arthroscopic Bankart repair shows a recurrence rate of 10.7% to 13.1%.[51][52] The rate of recurrence is higher in the following patients:
- Young age
- Excessive preoperative dislocations
- Significant bone loss
- Inferior capsule hyperlaxity
Decreased range of motion- reduction in external rotation is a common finding after arthroscopic Bankart repair.[53]
Open Bankarts Repair
- Recurrence: Open Bankart repair is associated with a low recurrence rate of 8%[54]
- Reduced range of motion- external and internal rotations are reduced - open Bankart repair shows more loss of rotations than arthroscopic Bankart repair
- Subscapularis rupture
- Prolonged operative time
- High incidence of sepsis[51]
Postoperative and Rehabilitation Care
Table 1. Rehabilitation protocol after arthroscopic Bankart repair[55]
| Postoperative week | Exercise | Continuation of the previous exercise | Comment |
| 0 to 4 weeks |
-Sling Immobilization -Passive ER (external rotation) only till neutral. |
_ | Avoid excessive external rotation. |
| 5 to 6 weeks |
-Discontinue Sling -Overhead stretching using rope and pulley. |
Passive external rotation only till neutral. | Avoid excessive external rotation. |
| 7 to 8 weeks |
-Passive external rotation stretching more than neutral. -Strengthening exercises with Thera band. -Resisted external rotation, internal rotation, one arm row, and biceps curl. |
Overhead stretching using rope and pulley. | The goal of passive external rotation is half of the external rotation of the opposite shoulder. |
| 4 to 6 months | Weight training in the gym |
-Strengthening exercises with Thera-band. -Resisted external rotation, internal rotation, one arm row, and biceps curl. |
_ |
| 6 months and onwards | Complete unrestrained activities, including contact sports. | _ | _ |
Rehabilitation Protocol After Open Latarjet Procedure
- 0 to 6 weeks- Sling immobilization, passive external rotation- till neutral
- 7 to 12 weeks- overhead and external rotation stretching only
- 12 weeks to 4 months- Strengthening exercises
- 4 to 6 months - Weight training in the gym
- From 6 months - Fully unrestrained activities[56]
Deterrence and Patient Education
Educating the athletes about the mechanism of injury of Bankart lesions will help them avoid such injuries. Discussing the various methods of treatment of Bankart lesion and their pros/cons with the patient is necessary. The patient must be educated about the importance of physical therapy and rehabilitation protocol for a good recovery. Patients are encouraged to do shoulder muscle strengthening exercises, avoid provocation maneuvers of shoulder dislocations, do shoulder girdle strengthening exercises, avoid redislocations, and wear protective gear while playing.
Enhancing Healthcare Team Outcomes
Progress in arthroscopic techniques has improved the surgical care of Bankart lesions. Arthroscopic Bankart repair is less morbid than open repair. Bankart lesions are more troublesome for young athletes involved in overhead activities. Treatment of the Bankart lesion is complicated by associated injuries to the glenoid rim and humeral head. Glenoid bone loss and the humeral head defect will mandate additional procedures to prevent the recurrence after Bankart repair. Strict adherence to structured rehabilitation protocol is crucial for returning to sport. This is where an interprofessional team approach to management is vital.
The comprehensive management of such injuries requires interprofessional coordination between the orthopedic surgeon, musculoskeletal radiologist, nursing staff, and physiotherapist. The surgeon will take the lead on these cases, but all team members must contribute from their specialties to guide the patient outcome. Nursing will assist in patient evaluation, serve as the liaison between specialties, and counsel patients. They will also often assist during surgical repair. Pharmacists can have a minor role in ensuring proper post-operative pain control is appropriate and that there are no drug interactions while counseling the patient on their medications. The physical therapist is undoubtedly a key player in managing these injuries, either through conservative management to avoid surgery or post-operatively to restore function. Everyone on the interprofessional care team must maintain accurate and updated records so all caregivers have accurate information from which to make decisions, and open lines of communication among all team members are crucial to successful patient outcomes. [Level 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Chang LR, Anand P, Varacallo M. Anatomy, Shoulder and Upper Limb, Glenohumeral Joint. StatPearls. 2024 Jan:(): [PubMed PMID: 30725703]
Saha AK. Dynamic stability of the glenohumeral joint. Acta orthopaedica Scandinavica. 1971:42(6):491-505 [PubMed PMID: 5144199]
Level 3 (low-level) evidenceClavert P. Glenoid labrum pathology. Orthopaedics & traumatology, surgery & research : OTSR. 2015 Feb:101(1 Suppl):S19-24. doi: 10.1016/j.otsr.2014.06.028. Epub 2015 Jan 14 [PubMed PMID: 25596985]
Burkhart SS,De Beer JF, Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy : the journal of arthroscopic [PubMed PMID: 11027751]
Sofu H, Gürsu S, Koçkara N, Oner A, Issın A, Camurcu Y. Recurrent anterior shoulder instability: Review of the literature and current concepts. World journal of clinical cases. 2014 Nov 16:2(11):676-82. doi: 10.12998/wjcc.v2.i11.676. Epub [PubMed PMID: 25405191]
Level 3 (low-level) evidenceTaylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. The American journal of sports medicine. 1997 May-Jun:25(3):306-11 [PubMed PMID: 9167808]
Aronen JG. Anterior shoulder dislocations in sports. Sports medicine (Auckland, N.Z.). 1986 May-Jun:3(3):224-34 [PubMed PMID: 3635924]
Murray IR,Ahmed I,White NJ,Robinson CM, Traumatic anterior shoulder instability in the athlete. Scandinavian journal of medicine [PubMed PMID: 22738342]
Mizuno K, Nabeshima Y, Hirohata K. Analysis of Bankart lesion in the recurrent dislocation or subluxation of the shoulder. Clinical orthopaedics and related research. 1993 Mar:(288):158-65 [PubMed PMID: 8458129]
Level 2 (mid-level) evidenceSu T, Chen GX, Yang L. Diagnosis and treatment of labral tear. Chinese medical journal. 2019 Jan 20:132(2):211-219. doi: 10.1097/CM9.0000000000000020. Epub [PubMed PMID: 30614856]
Kazár B, Relovszky E. Prognosis of primary dislocation of the shoulder. Acta orthopaedica Scandinavica. 1969:40(2):216-24 [PubMed PMID: 5365161]
Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. The Journal of bone and joint surgery. American volume. 1996 Nov:78(11):1677-84 [PubMed PMID: 8934481]
Level 1 (high-level) evidenceHovelius L. Incidence of shoulder dislocation in Sweden. Clinical orthopaedics and related research. 1982 Jun:(166):127-31 [PubMed PMID: 7083659]
Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from "engaging/non-engaging" lesion to "on-track/off-track" lesion. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2014 Jan:30(1):90-8. doi: 10.1016/j.arthro.2013.10.004. Epub [PubMed PMID: 24384275]
Gill TJ,Zarins B, Open repairs for the treatment of anterior shoulder instability. The American journal of sports medicine. 2003 Jan-Feb; [PubMed PMID: 12531772]
Gill TJ, Micheli LJ, Gebhard F, Binder C. Bankart repair for anterior instability of the shoulder. Long-term outcome. The Journal of bone and joint surgery. American volume. 1997 Jun:79(6):850-7 [PubMed PMID: 9199382]
Level 2 (mid-level) evidenceRowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. The Journal of bone and joint surgery. American volume. 1978 Jan:60(1):1-16 [PubMed PMID: 624747]
Level 3 (low-level) evidenceRobinson CM, Shur N, Sharpe T, Ray A, Murray IR. Injuries associated with traumatic anterior glenohumeral dislocations. The Journal of bone and joint surgery. American volume. 2012 Jan 4:94(1):18-26. doi: 10.2106/JBJS.J.01795. Epub [PubMed PMID: 22218378]
Skupiński J,Piechota MZ,Wawrzynek W,Maczuch J,Babińska A, The Bony Bankart Lesion: How to Measure the Glenoid Bone Loss. Polish journal of radiology. 2017; [PubMed PMID: 28243338]
Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2004 Feb:20(2):169-74 [PubMed PMID: 14760350]
Provencher MT, Frank RM, Leclere LE, Metzger PD, Ryu JJ, Bernhardson A, Romeo AA. The Hill-Sachs lesion: diagnosis, classification, and management. The Journal of the American Academy of Orthopaedic Surgeons. 2012 Apr:20(4):242-52. doi: 10.5435/JAAOS-20-04-242. Epub [PubMed PMID: 22474094]
Gyftopoulos S, Yemin A, Beltran L, Babb J, Bencardino J. Engaging Hill-Sachs lesion: is there an association between this lesion and findings on MRI? AJR. American journal of roentgenology. 2013 Oct:201(4):W633-8. doi: 10.2214/AJR.12.10206. Epub [PubMed PMID: 24059403]
Itoi E. 'On-track' and 'off-track' shoulder lesions. EFORT open reviews. 2017 Aug:2(8):343-351. doi: 10.1302/2058-5241.2.170007. Epub 2017 Aug 1 [PubMed PMID: 28932486]
Loh B, Lim JB, Tan AH. Is clinical evaluation alone sufficient for the diagnosis of a Bankart lesion without the use of magnetic resonance imaging? Annals of translational medicine. 2016 Nov:4(21):419 [PubMed PMID: 27942510]
Gül O, Okutan AE, Ayas MS. Arthroscopic glenoid labral lesion repair using all-suture anchor for traumatic anterior shoulder instability: short-term results. Journal of shoulder and elbow surgery. 2019 Oct:28(10):1991-1997. doi: 10.1016/j.jse.2019.03.003. Epub 2019 May 14 [PubMed PMID: 31101476]
Farber AJ,Castillo R,Clough M,Bahk M,McFarland EG, Clinical assessment of three common tests for traumatic anterior shoulder instability. The Journal of bone and joint surgery. American volume. 2006 Jul; [PubMed PMID: 16818971]
Level 1 (high-level) evidenceBushnell BD, Creighton RA, Herring MM. The bony apprehension test for instability of the shoulder: a prospective pilot analysis. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2008 Sep:24(9):974-82. doi: 10.1016/j.arthro.2008.07.019. Epub [PubMed PMID: 18760203]
Level 3 (low-level) evidenceProvencher MT, LeClere LE, King S, McDonald LS, Frank RM, Mologne TS, Ghodadra NS, Romeo AA. Posterior instability of the shoulder: diagnosis and management. The American journal of sports medicine. 2011 Apr:39(4):874-86. doi: 10.1177/0363546510384232. Epub 2010 Dec 4 [PubMed PMID: 21131678]
Morey VM, Singh H, Paladini P, Merolla G, Phadke V, Porcellini G. The Porcellini test: a novel test for accurate diagnosis of posterior labral tears of the shoulder: comparative analysis with the established tests. Musculoskeletal surgery. 2016 Dec:100(3):199-205 [PubMed PMID: 27591779]
Level 2 (mid-level) evidenceKim SH,Park JS,Jeong WK,Shin SK, The Kim test: a novel test for posteroinferior labral lesion of the shoulder--a comparison to the jerk test. The American journal of sports medicine. 2005 Aug; [PubMed PMID: 16000664]
Valencia Mora M,Ibán MÁR,Heredia JD,Gutiérrez-Gómez JC,Diaz RR,Aramberri M,Cobiella C, Physical Exam and Evaluation of the Unstable Shoulder. The open orthopaedics journal. 2017; [PubMed PMID: 29114336]
Smits-Engelsman B, Klerks M, Kirby A. Beighton score: a valid measure for generalized hypermobility in children. The Journal of pediatrics. 2011 Jan:158(1):119-23, 123.e1-4. doi: 10.1016/j.jpeds.2010.07.021. Epub 2010 Sep 17 [PubMed PMID: 20850761]
Rozing PM, de Bakker HM, Obermann WR. Radiographic views in recurrent anterior shoulder dislocation. Comparison of six methods for identification of typical lesions. Acta orthopaedica Scandinavica. 1986 Aug:57(4):328-30 [PubMed PMID: 3788496]
Yoo JC, Lee YS, Tae SK, Park JH, Park JW, Ha HC. Magnetic resonance imaging appearance of a repaired capsulolabral complex after arthroscopic bankart repair. The American journal of sports medicine. 2008 Dec:36(12):2310-6. doi: 10.1177/0363546508322477. Epub 2008 Sep 5 [PubMed PMID: 18776021]
Level 2 (mid-level) evidenceChuang TY,Adams CR,Burkhart SS, Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy : the journal of arthroscopic [PubMed PMID: 18375267]
Level 2 (mid-level) evidenceBottoni CR, Wilckens JH, DeBerardino TM, D'Alleyrand JC, Rooney RC, Harpstrite JK, Arciero RA. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. The American journal of sports medicine. 2002 Jul-Aug:30(4):576-80 [PubMed PMID: 12130413]
Level 1 (high-level) evidenceResch H, Benedetto KP, Kadletz R, Oberhammer J. [Indications for the Bankart operation]. Aktuelle Traumatologie. 1985 Jun:15(3):122-6 [PubMed PMID: 2863957]
DeFroda S, Bokshan S, Stern E, Sullivan K, Owens BD. Arthroscopic Bankart Repair for the Management of Anterior Shoulder Instability: Indications and Outcomes. Current reviews in musculoskeletal medicine. 2017 Dec:10(4):442-451. doi: 10.1007/s12178-017-9435-2. Epub [PubMed PMID: 28971317]
Davis DE,Abboud JA, Operative Management Options for Traumatic Anterior Shoulder Instability in Patients Younger Than 30 Years. Orthopedics. 2015 Sep; [PubMed PMID: 26375529]
Ranalletta M, Rossi LA, Alonso Hidalgo I, Sirio A, Puig Dubois J, Maignon GD, Bongiovanni SL. Arthroscopic Stabilization After a First-Time Dislocation: Collision Versus Contact Athletes. Orthopaedic journal of sports medicine. 2017 Sep:5(9):2325967117729321. doi: 10.1177/2325967117729321. Epub 2017 Sep 25 [PubMed PMID: 28979919]
Taverna E, Garavaglia G, Ufenast H, D'Ambrosi R. Arthroscopic treatment of glenoid bone loss. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2016 Feb:24(2):546-56. doi: 10.1007/s00167-015-3893-0. Epub 2015 Dec 12 [PubMed PMID: 26658567]
Gouveia K, Abidi SK, Shamshoon S, Gohal C, Madden K, Degen RM, Leroux T, Alolabi B, Khan M. Arthroscopic Bankart Repair With Remplissage in Comparison to Bone Block Augmentation for Anterior Shoulder Instability With Bipolar Bone Loss: A Systematic Review. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2021 Feb:37(2):706-717. doi: 10.1016/j.arthro.2020.08.033. Epub 2020 Sep 7 [PubMed PMID: 32911004]
Level 1 (high-level) evidenceHaroun HK,Sobhy MH,Abdelrahman AA, Arthroscopic Bankart repair with remplissage versus Latarjet procedure for management of engaging Hill-Sachs lesions with subcritical glenoid bone loss in traumatic anterior shoulder instability: a systematic review and meta-analysis. Journal of shoulder and elbow surgery. 2020 Oct; [PubMed PMID: 32807370]
Level 1 (high-level) evidenceShin SJ, Kim RG, Jeon YS, Kwon TH. Critical Value of Anterior Glenoid Bone Loss That Leads to Recurrent Glenohumeral Instability After Arthroscopic Bankart Repair. The American journal of sports medicine. 2017 Jul:45(9):1975-1981. doi: 10.1177/0363546517697963. Epub 2017 Mar 23 [PubMed PMID: 28333542]
Dickens JF,Owens BD,Cameron KL,DeBerardino TM,Masini BD,Peck KY,Svoboda SJ, The Effect of Subcritical Bone Loss and Exposure on Recurrent Instability After Arthroscopic Bankart Repair in Intercollegiate American Football. The American journal of sports medicine. 2017 Jul; [PubMed PMID: 28474965]
Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. Journal of shoulder and elbow surgery. 2011 Mar:20(2 Suppl):S61-9. doi: 10.1016/j.jse.2010.07.022. Epub 2010 Dec 9 [PubMed PMID: 21145262]
Lorenzetti A, Streit JJ, Cabezas AF, Christmas KN, LaMartina J 2nd, Simon P, Frankle MA. Bone Graft Augmentation for Severe Glenoid Bone Loss in Primary Reverse Total Shoulder Arthroplasty: Outcomes and Evaluation of Host Bone Contact by 2D-3D Image Registration. JB & JS open access. 2017 Sep 28:2(3):e0015. doi: 10.2106/JBJS.OA.17.00015. Epub 2017 Jul 28 [PubMed PMID: 30229222]
Neviaser TJ, The anterior labroligamentous periosteal sleeve avulsion lesion: a cause of anterior instability of the shoulder. Arthroscopy : the journal of arthroscopic [PubMed PMID: 8442824]
Wischer TK, Bredella MA, Genant HK, Stoller DW, Bost FW, Tirman PF. Perthes lesion (a variant of the Bankart lesion): MR imaging and MR arthrographic findings with surgical correlation. AJR. American journal of roentgenology. 2002 Jan:178(1):233-7 [PubMed PMID: 11756126]
Kelley TD, Clegg S, Rodenhouse P, Hinz J, Busconi BD. Functional Rehabilitation and Return to Play After Arthroscopic Surgical Stabilization for Anterior Shoulder Instability. Sports health. 2022 Sep-Oct:14(5):733-739. doi: 10.1177/19417381211062852. Epub 2021 Dec 17 [PubMed PMID: 34918564]
Level 2 (mid-level) evidenceGreen MR, Christensen KP. Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 1993:9(4):371-4 [PubMed PMID: 8216566]
Level 2 (mid-level) evidenceSommaire C,Penz C,Clavert P,Klouche S,Hardy P,Kempf JF, Recurrence after arthroscopic Bankart repair: Is quantitative radiological analysis of bone loss of any predictive value? Orthopaedics [PubMed PMID: 22884854]
Level 2 (mid-level) evidenceMatsuki K, Sugaya H. Complications after arthroscopic labral repair for shoulder instability. Current reviews in musculoskeletal medicine. 2015 Mar:8(1):53-58. doi: 10.1007/s12178-014-9248-5. Epub [PubMed PMID: 25532917]
Lützner J, Krummenauer F, Lübke J, Kirschner S, Günther KP, Bottesi M. Fuctional outcome after open and arthroscopic bankart repair for traumatic shoulder instability. European journal of medical research. 2009 Jan 28:14(1):18-24 [PubMed PMID: 19258206]
Level 2 (mid-level) evidenceDeFroda SF, Mehta N, Owens BD. Physical Therapy Protocols for Arthroscopic Bankart Repair. Sports health. 2018 May/Jun:10(3):250-258. doi: 10.1177/1941738117750553. Epub 2018 Jan 3 [PubMed PMID: 29298132]
Fedorka CJ, Mulcahey MK. Recurrent anterior shoulder instability: a review of the Latarjet procedure and its postoperative rehabilitation. The Physician and sportsmedicine. 2015 Feb:43(1):73-9. doi: 10.1080/00913847.2015.1005543. Epub 2015 Jan 19 [PubMed PMID: 25598036]