Introduction
Pneumocephalus, also known as pneumatocele or intracranial aerocele, is the presence of air in the epidural, subdural, or subarachnoid spaces, the brain parenchyma, or ventricular cavities.[1] Lecat first described this condition in 1741, but Luckett independently coined the term "pneumocephalus" in 1913. Wolff used the same term to describe the condition in 1914.[2][3][4] The term "tension pneumocephalus" was proposed in 1962 by Ectors, Kessler, and Stern (see Image. Tension Pneumocephalus).[5][6]
Pneumocephalus can occur spontaneously or result from trauma or cranial surgery. This condition is classified as simple or tension pneumocephalus, depending on severity and progression. Pneumocephalus may also be acute or delayed based on disease onset. Acute pneumocephalus develops less than 72 hours before presentation, while the delayed type arises more than 72 hours after presentation.[7]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Pneumocephalus may be traumatic, infectious, neoplastic, iatrogenic, or spontaneous.[8] The causes are summarized below (see Table. Possible Causes of Pneumocephalus). The most common etiology of pneumocephalus is head or facial trauma, which accounts for almost 75% of cases. Air can enter the cranial cavity through skull fractures.[9]
Table. Possible Causes of Pneumocephalus
|
Traumatic
|
|
Infectious |
|
Neoplastic
|
|
Iatrogenic
|
|
Spontaneous
|
|
Congenital
|
|
Miscellaneous
|
*Hydrogen peroxide can release oxygen and water upon contact with catalase and egress through the epidural or subdural space, resulting in intracranial pneumatosis.
Epidemiology
The incidence of pneumocephalus varies with the underlying etiology. The condition is seen in almost all postcraniotomy patients. The incidence of pneumocephalus following head injury varies by study but ranges from 1% to as high as 82%. Approximately 74% of documented pneumocephalus cases are due to head trauma.[25][26]
Pathophysiology
Several theories regarding the pathogenic mechanisms of pneumocephalus exist. These theories include:
- Air moves unidirectionally through a dural tear from the outside environment and is trapped inside the cranial cavity. This mechanism is responsible for pneumocephalus following positive pressure ventilation, coughing, and sneezing. This theory is called the "one-way ball-valve theory of Dandy."
- Intracranial pressure (ICP) decreases due to excessive CSF loss, which may occur artificially via lumbar drainage or physiologically during Valsalva maneuvers. This intracranial hypotension creates a vacuum that paradoxically draws in atmospheric air and traps it inside the cranium. This state persists until equilibrium is achieved between intracranial and extracranial pressures. This theory is called the "inverted-soda-bottle effect of Horowitz and Lunsford."
- Blowing the nose, coughing, or sneezing causes a sudden pressure increase in the air sinuses. Air is then drawn into the brain through defects in the skull base.
- The loss-of-resistance technique, used to identify the epidural space, is thought to be responsible for the development of pneumocephalus after epidural injections.
- Air entry through the meninges may be due to accidental injection, inadvertent dural puncture, or pressure gradients between the cranial cavity and atmosphere.
- Nitrous oxide may cause pneumocephalus during anesthetic procedures. The blood–gas partition coefficient of nitrous oxide is 34 times greater than that of nitrogen. Therefore, nitrous oxide can diffuse into the cranial cavity faster than nitrogen or air.
- Boyle's law states that pressure and volume are inversely proportional at constant temperature. Pneumocephalus expands during flights because air volume increases when pressure decreases inside the cranial cavity.[27][28]
Intraoperative pneumocephalus can occur during cranial intervention owing to various risk variables, including:
- Concurrent brain atrophy
- Loss of the CSF negative-pressure gradient due to CSF egress
- Semisitting surgical position [29]
The anatomic location and portal of air entry divide the condition into the following categories:
- Intraarterial: Almost 80% of cases occur after surgical or interventional procedures. The SWIFT trial, which investigated the Solitaire and Merci clot retrieval devices, reported a 1.4% incidence of pneumocephalus. Intraarterial pneumocephalus may also arise from paradoxical air embolism due to right-to-left heart or lung shunting (eg, from a patent foramen ovale, atrial septal defect, or pulmonary arteriovenous fistula) or from barotrauma during deep diving.
- Intravenous: Cases typically arise from vascular access procedures (eg, peripheral intravenous or neck central-line placement), with air traveling primarily to the cavernous sinus via the internal jugular vein. The reported incidence is 0.034%. Air often spreads to multiple intracranial and extracranial sites and is usually benign, though air collection in the dural cavernous and sigmoid venous sinuses may result from septic thrombosis linked to infections such as sinusitis, otitis, mastoiditis, or dental infections, potentially presenting as acute cavernous sinus syndrome or thrombosis.
- Subdural and intraparenchymal: These cases comprise the most common forms of postoperative pneumocephalus. These types are mostly benign and often resolve in 3 weeks.
- Epidural: This type occurs mainly through skull fractures, including breaks involving the mastoid air cells or a paranasal sinus. However, gas and fluid-containing collections adjacent to opacified mastoid air cells or a paranasal sinus may be due to empyema.
- Subarachnoid or ventricular: Air can enter from the spine, most often after spinal epidural anesthesia. Cases resulting from mass lesions or infections carry a risk of meningitis. Subarachnoid gas has been reported in meningitis due to pathogens such as Streptococcus pneumonia and other streptococcal spp., as well as Clostridium perfringens. Air may reach the ventricular system through recirculation from the subarachnoid space after surgery or a penetrating injury. Subarachnoid gas with meningitis should prompt consideration of infectious pathologies.[30]
Skull fractures and dural defects leave the cranial cavity vulnerable to air entry. Large air pockets can compress intracranial structures and increase the ICP, leading to herniation syndrome. Air is also a potential source of intracranial infection. Air entering the meninges can likewise irritate the cerebral cortex and produce seizures.
History and Physical
Pneumocephalus is a medical emergency despite its variable presentation. A quick primary survey—assessing the airway, breathing, circulation, disability, and exposure (ABCDE)—must be performed immediately upon receiving the patient. Unconscious individuals without respirations and pulses must be administered resuscitative measures promptly, regardless of cause. Once the patient's emergent needs are addressed, the secondary survey and diagnostic workup may be initiated.
The patient's history is likely to reveal a recent traumatic incident leading to a skull fracture. Symptoms depend on the pneumocephalus volume and intracranial area affected. Most patients are asymptomatic. However, symptomatic conscious patients may have nausea, vomiting, memory loss, speech and sensory changes, rhinorrhea or otorrhea, seizures, headaches, and motor weakness. Though rare, patients may describe a splashing sound during head movement, known as "bruit hydroaerique," which is pathognomonic of pneumocephalus. Cranial auscultation may confirm this sign. Tympany may be evident during skull percussion.[31]
An enlarging pneumatocele can have a mass effect that may lead to intracranial hypertension and neurological deterioration. Such cases are classified as tension pneumatocele, which is life-threatening. Severe tension pneumatocele may present with altered sensorium, abnormal breathing patterns (Cushing reflex), or cardiorespiratory arrest.[32] Tension pneumocephalus involving the posterior fossa manifests with brainstem signs, respiratory irregularities, and cardiac arrest. In individuals without a history of trauma, a recent neurosurgical or spinal procedure, infection symptoms, signs of intracranial mass effects, or a history of ventilator use or congenital anomalies may be elicited.
The head and neck examination may reveal scalp or skin lacerations, evidence of a skull fracture, blood and fluid in the nose or external auditory meatus, and tympanic membrane perforation. Evidence of multiple traumatic injuries includes respiratory distress signs, hypotension, tachycardia, abdominal rigidity, blood in the genitalia, bloody urine, and axioappendicular fractures. In patients with barotrauma, unilaterally decreased breath sounds (pneumothorax) or a positive Hamman sign (pneumomediastinum) may be noted on auscultation. Neurologic and musculoskeletal findings vary, depending on the site affected.
The following features of the patient's history or examination should make clinicians suspicious that the patient may have pneumocephalus:
- CSF leak from the nose, ear, or surgical site
- Persistent headache after cranial or spinal surgery
- Seizures following surgery
- Postoperative meningitis
- Frontal lobe syndrome
- Flapping scalp sign
- Oculomotor nerve palsy
- Papilledema
- Tinnitus [33][34]
Septic cavernous sinus thrombosis can present with headache, eye pain, ophthalmoplegia, cranial nerve deficits, and signs of infection (sinusitis, otitis, mastoiditis, or dental). Postoperative abscesses may present with fever, headache, altered sensorium, seizure, and purulent drainage from the surgical site. Epidural or subdural empyema may present with seizure, headache, fever, and lethargy alongside intracranial hypertension symptoms, focal neurological deficits, and papilledema.
Evaluation
Monitoring and Laboratory Testing
Individuals who appear unstable require continuous vital sign and cardiac monitoring. A capillary blood glucose must be performed for all unconscious patients to rule out or address hypoglycemia. Individuals requiring oxygen supplementation must be monitored by pulse oximetry.
Laboratory testing must be performed immediately for patients with trauma, especially if emergency surgery is considered. The initial tests may include a complete blood count, coagulation profile, blood typing, complete metabolic panel, and urinalysis. Arterial blood gases and electrocardiography may be considered if the patient exhibits cardiorespiratory distress. Imaging studies must be immediately scheduled.
Plain Radiography
Skull x-rays have been used to identify pneumocephalus, but plain films usually miss small quantities of air. Still, x-rays help evaluate multiple injuries or show opacities in the air sinuses, suggesting an infection.
Noncontrast Head Computed Tomography
Head computed tomography (CT) without contrast is the gold standard imaging modality in diagnosing pneumocephalus. This study can detect even 0.55 mL of intracranial air, while a skull radiograph requires at least 2 mL to be appreciable.[35] Air has a Hounsfield coefficient of -1000.
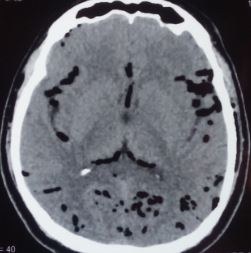
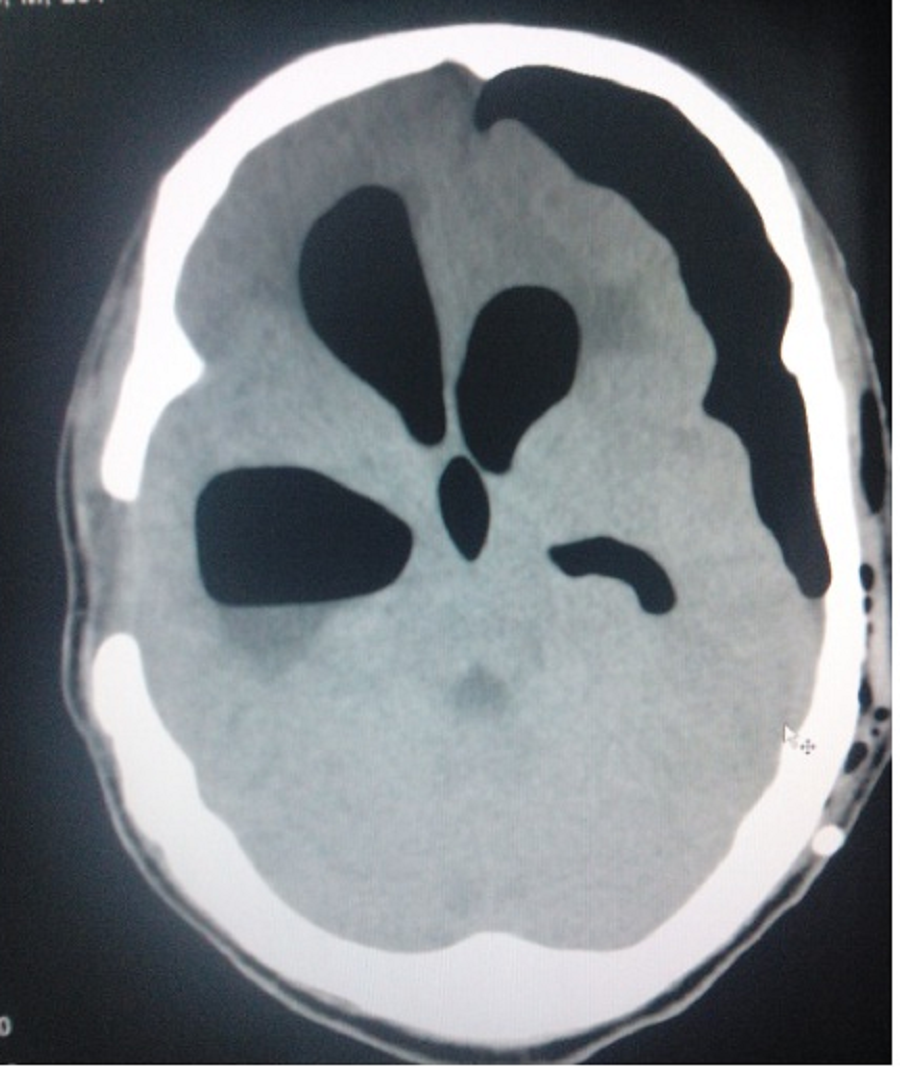
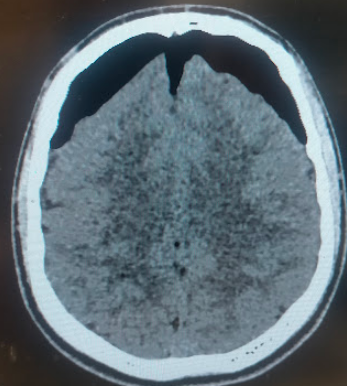
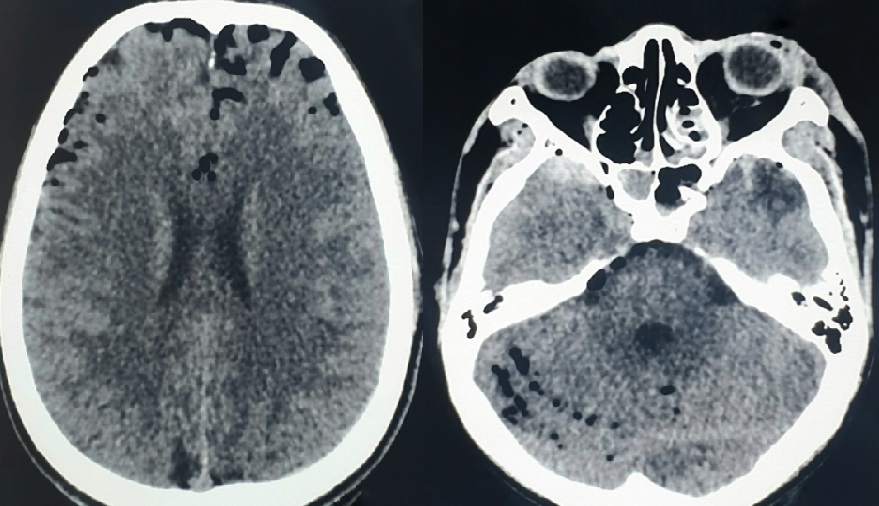
Ishiwata et al identified 2 signs as characteristic of tension pneumocephalus. The first is the "Mount Fuji" sign, named after Mount Fuji, the highest volcano in Japan. This sign is diagnostic of tension pneumocephalus and arises from the accumulation of air in the frontal region, separating the frontal lobes' tips in a patient in the supine position (see Image. Mount Fuji Sign in Tension Pneumocephalus). The second is the "air bubble sign," denoting the presence of multiple air bubbles scattered in several cisterns (see Image. Air Bubble Sign in Tension Pneumocephalus).[36]
On the other hand, the "peaking sign" denotes bilateral compression of the frontal lobes without separation of the tips. This sign indicates a less severe condition than the Mount Fuji sign.
Calculation of the Volume of Postoperative Pneumocephalus
The volume of intracranial air may be determined in 2 ways. The first is by computer-assisted volumetric measurement, which requires special software. The second is by using the ABC/2 formula at the bedside, which requires the following steps when determining the parameters:
- Select a representative image near the center of the pneumocephalus.
- Measure "A" or the greatest longitudinal length of the pneumocephalus in millimeters in the axial plane.
- Measure "B" or the maximum width in millimeters of the pneumocephalus from the skull's inner table perpendicular to "A" on the same slice.
- Measure "C" or the height of the air in the coronal plane, which is the same as the number of CT axial images showing the pneumocephalus multiplied by the slice thickness.
- Calculate the estimated volume in milliliters using the formula = (A x B x C)/2.
The ABC/2 formula correlates well with computer-derived values.[37]
Brain Magnetic Resonance Imaging
Brain magnetic resonance imaging (MRI) may also be useful but is less sensitive than CT in diagnosing pneumocephalus. On MRI, air may be mistaken for flow voids or blood products, appearing dark in almost all sequences.
Treatment / Management
The Advanced Trauma Life Support (ATLS) protocol is a widely recognized, systematic approach to trauma patient care that focuses on critical interventions during initial patient assessment and resuscitation. The initial management of any head injury should follow this protocol. Once the patient is stabilized and diagnostics have been obtained, the pneumocephalus must be classified to determine the appropriate treatment plan.
Most patients present with simple pneumocephalus, lacking neurological symptoms and signs of increased ICP. The head CT typically reveals intracranial air without tension pneumocephalus indicators like the Mount Fuji sign. Intracranial air disappears over time through tissue absorption. Management is conservative and involves the following measures:
- Bed rest
- Placing the patient in a 30° Fowler position
- Avoiding Valsalva maneuvers like nose-blowing, coughing, and sneezing
- Analgesics and antipyretics
- Osmotic diuretics, if indicated
- High-flow oxygen therapy is given at 5 L/min for at least 5 days via a face tent or 100% nonrebreather mask with absolute avoidance of positive pressure and
- Hyperbaric oxygen therapy [37] (B3)
Atmospheric air is composed of 78% nitrogen and 21% oxygen. The rate of nitrogen absorption from intracranial air depends on nitrogen's partial pressure in the blood, which is inversely proportional to the fraction of inspired oxygen.
Oxygen supplementation reduces blood and brain nitrogen concentration, increasing the nitrogen gradient between the pneumocephalus air collection and surrounding brain tissue. Over time, oxygen replaces intracranial nitrogen—which is well-absorbed in brain tissue and blood—by diffusion, facilitating nitrogen absorption and eventual pneumocephalus resolution.[38] Despite the heterogeneity in delivery modes, which include nonrebreather masks, endotracheal tubes, and hyperbaric chambers, oxygen therapy enhances the reabsorption and resolution of pneumocephalus.[39] Serial CT imaging studies may be obtained to monitor the condition.(A1)
Although pneumocephalus poses an increased intracranial infection risk, prophylactic antibiotics do not appear to provide a protective advantage in patients with traumatic pneumocephalus. However, emergent surgical decompression is required when clinical signs manifest. In cases of pneumocephalus complicated with abscess and empyema, surgical drainage, eradication of the infection source, and broad-spectrum antibiotics are recommended.
Surgery is also indicated in the following conditions:
- Symptomatic pneumocephalus
- Tension pneumocephalus
- Recurrent pneumocephalus
- Persistent traumatic pneumocephalus lasting more than 1 week
- Tension pneumoventricle (see Image. Pneumocephalus and Pneumoventriculi)
Strategies for surgical decompression include the following:
- Needle aspiration, either blind or under radiological guidance through an existing burr hole or craniotomy
- Controlled decompression via a subdural drain connected to an underwater seal followed by dural defect closure
- Ventriculostomy for tension pneumoventricle
- Emergency decompression by the creation of fresh cranial burr holes
- Decompressive craniectomy
- Saline-primed Camino bolt insertion
- Subdural evacuating port system (SEPS) insertion
- Endoscopic endonasal eustachian tube obliteration during lateral skull base surgery
- Placing the patient in the Trendelenburg position in the presence of a subarachnoid-pleural fistula facilitates the dissipation of some intracranial air into the spinal canal. This maneuver also helps create an epidural patch at the pleural apex, thereby sealing the dural rent and obliterating the fistula.
- Endovascular suctioning of intraarterial air [40][41][42][43] (B3)
Specific preventive strategies for preventing the occurrence of pneumocephalus following cranial surgeries include the following:
- Water-tight sealing of the surgical site during endoscopic transsphenoidal surgery
- Using a prophylactic frontal drainage system
- Placing the patient in the recombinant position before opening the dura
- Initiating liberal irrigation of the surgical site and potentially injured venous sinus, with wax closure of the burr holes to prevent air embolism [44][45] (A1)
Differential Diagnosis
Pneumocephalus must be differentiated from the following terms:
- Pneumorrhachis, which denotes intraspinal air
- Pneumocele, which is a focal or diffuse paranasal sinus (usually frontal) enlargement with bone thinning and hyperpneumatization
- Pneumosinus dilatans, which may appear the same on imaging as a pneumocele but have the sinus walls intact and normal
Pneumocephalus may be confused with other structures on imaging studies. For example, intracranial fat may appear hypodense on CT scans and be mistaken for pneumocephalus, though it has a much higher density (-90 HU) than air (-1000 HU). Pneumocephalus may also resemble blood products or flow voids on MRI.
Prognosis
Simple pneumocephalus usually resolves spontaneously with conservative therapy. However, this condition occasionally produces seizures and meningitis. Prognosis is generally good even with tension pneumocephalus, provided timely treatment is given.
The presence of pneumocephalus may suggest chemical meningitis following corpus callosotomy.[46] The postsurgical appearance of pneumocephalus is also a predictor of chronic subdural hematoma recurrence after evacuation. Thus, pneumocephalus is a component of the Puerto Rico Recurrence Scale.[47]
Complications
The potential complications of pneumocephalus include meningitis, seizures, brain abscess, brain herniation secondary to tension pneumocephalus, and death. Early intervention can prevent these complications and improve patient outcomes.
Extensive postoperative convexity pneumocephalus increases the risk of recurrent chronic subdural hematoma.[48] In functional surgeries such as deep brain stimulation, pneumocephalus may indicate targeting inaccuracies, leading to suboptimal clinical outcomes.[49]
Deterrence and Patient Education
The following methods can help prevent the development of pneumocephalus during or after surgical procedures:
- Filling of the surgical site with saline at the time of dural closure
- Administering the Valsalva maneuver during closure, before the last dural suture, to allow air to escape outside
- Using a smaller-gauge spinal needle for lumbar puncture to make a smaller dural perforation and minimize CSF leakage
- Keeping the patient in the supine position with no head-end of bed elevation following chronic subdural hematoma evacuation
- Positioning the head during dural closure so that the last part of the dural defect becomes the highest point. This step facilitates the escape of residual air while filling the subdural space with saline.
- Using saline rather than air to identify the epidural space during epidural injections
- Avoiding high airway pressure and hyperventilation during invasive ventilation
The inhalational anesthetic nitrous oxide was previously thought to cause pneumocephalus if not withdrawn before dural closure. However, a randomized control trial demonstrated that nitrous oxide did not cause a significant ICP increase or produce large pneumocephalus volumes even if administered postoperatively.[50]
Evidence does not support the prophylactic administration of ceftriaxone for preventing meningitis in patients with traumatic pneumocephalus.[51]
Neurosurgical procedures may result in residual intracranial air and also cause continuous air entry into the cranial cavity. Hence, patients must be advised to wait at least 7 days before flying, as cabin pressure changes can introduce air intracranially.[52] Air travel is not advisable for patients with an intracranial air volume of more than 30 mL. An intracranial air volume of 20 mL and an initial ICP of 15 mm Hg are considered conservative thresholds for safe air travel among such patients.[53]
The following measures may be recommended to patients at risk to avoid complications from pneumocephalus during a flight:
- Taking a low-level flight or maintaining ground-level cabin pressure during the flight
- Avoiding frequent cabin pressure changes
- Seeking a position that reduces CSF leaks
- Administering supplementary oxygen
- Taking preflight decongestants
- Avoiding Valsalva maneuvers
Healthcare providers may also help avoid complications in these individuals by performing the following:
- Preventing hypoventilation and carbon dioxide accumulation if the patient is ventilated
- Obtaining imaging studies immediately before the flight to assess the volume of pneumocephalus and rule out an extracranial-intracranial fistulous process
- Educating patients regarding patient activity-related pathophysiology and the time course of pneumocephalus
- Reducing the stresses induced by acceleration (including changing g-forces), noise, or hypoxemia [54]
Avoiding air travel for 2 to 8 weeks after intracranial surgery is recommended.[55]
Pearls and Other Issues
The most important points to remember when evaluating and managing pneumocephalus are the following:
- Pneumocephalus has various causes, but most are trauma-related.
- Determining the intracranial location and point of air entry allows for the classification of pneumocephalus into benign or complex subtypes, facilitating the development of specific management algorithms.
- The condition presents variably. Most patients have the simple type and are asymptomatic, but complications can develop if tension pneumocephalus is not treated immediately.
- The management of all patients with suspected head trauma should follow ATLS protocol.
- Noncontrast CT is the imaging modality of choice for pneumocephalus.
- Simple pneumocephalus may be managed conservatively. Antibiotics have little effect on intracranial infection risk in patients with pneumocephalus.
- Surgery is reserved for patients with symptomatic, recurrent, or persistent traumatic pneumocephalus lasting more than a week and tension pneumocephalus or pneumoventricle.
- The prognosis is generally good for patients with simple pneumocephalus. Prompt intervention significantly improves the prognosis of tension pneumocephalus.
Notably, the definitive treatment depends on the specific etiology of pneumocephalus and the patient's clinical condition. Pneumocephalus typically resolves in 3 weeks. Otherwise, a subtle but persistent defect in the skull base or air sinuses should be considered.
Enhancing Healthcare Team Outcomes
The management of pneumocephalus must involve an interprofessional healthcare team to produce the best outcomes. The team members should include the following care providers:
- Emergency medicine physician: often the first healthcare professional to encounter patients with head trauma or acute neurological symptoms. This provider performs the initial assessment, stabilizes the patient, and coordinates with specialists for further management.
- Radiologist: interprets imaging studies to confirm the diagnosis, assess the extent of pneumocephalus, and identify any associated injuries or conditions. The radiologist's expertise is crucial in guiding the treatment plan.
- Neurosurgeon: assesses the extent of pneumocephalus and may perform necessary surgical procedures.
- Intensivist: may treat patients with pneumocephalus in the intensive care unit.
- Anesthesiologists: may be involved in cases requiring surgical intervention.
- Infectious disease specialist: may be consulted to guide the appropriate antimicrobial therapy and overall management if an intracranial infection develops as a complication of pneumocephalus.
- Respiratory therapist: assists in managing ventilator settings, ensuring adequate oxygenation, and monitoring the patient's respiratory status when mechanical ventilation is required.
- Occupational and physical therapists: providers who may be involved in the later stages of care to assess and facilitate the patient's recovery, primarily if neurological deficits or functional impairments exist.
- Primary care physician: monitors patients and coordinates care in the outpatient setting.
Effective communication and collaboration among these healthcare professionals are essential to ensuring a coordinated and well-rounded approach to pneumocephalus's short and long-term management.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Álvarez-Holzapfel MJ, Aibar Durán JÁ, Brió Sanagustin S, de Quintana-Schmidt C. [Diffuse pneumocephalus after lumbar stab wound]. Anales de pediatria. 2019 Jan:90(1):63-64. doi: 10.1016/j.anpedi.2018.04.012. Epub 2018 Jun 11 [PubMed PMID: 29903638]
Yates H, Hamill M, Borel CO, Toung TJ. Incidence and perioperative management of tension pneumocephalus following craniofacial resection. Journal of neurosurgical anesthesiology. 1994 Jan:6(1):15-20 [PubMed PMID: 8298259]
Level 3 (low-level) evidenceJELSMA F, MOORE DF. Cranial aerocele. American journal of surgery. 1954 Mar:87(3):437-51 [PubMed PMID: 13124659]
Schirmer CM, Heilman CB, Bhardwaj A. Pneumocephalus: case illustrations and review. Neurocritical care. 2010 Aug:13(1):152-8. doi: 10.1007/s12028-010-9363-0. Epub [PubMed PMID: 20405340]
Level 3 (low-level) evidenceKankane VK, Jaiswal G, Gupta TK. Posttraumatic delayed tension pneumocephalus: Rare case with review of literature. Asian journal of neurosurgery. 2016 Oct-Dec:11(4):343-347 [PubMed PMID: 27695534]
Level 3 (low-level) evidenceWankhade BS, Beniamein MMK, Alrais ZF, Mathew JI, Alrais GZ. What should an intensivist know about pneumocephalus and tension pneumocephalus? Acute and critical care. 2023 May:38(2):244-248. doi: 10.4266/acc.2021.01102. Epub 2022 Apr 13 [PubMed PMID: 35545242]
Pillai P, Sharma R, MacKenzie L, Reilly EF, Beery PR 2nd, Papadimos TJ, Stawicki SP. Traumatic tension pneumocephalus - Two cases and comprehensive review of literature. International journal of critical illness and injury science. 2017 Jan-Mar:7(1):58-64. doi: 10.4103/IJCIIS.IJCIIS_8_17. Epub [PubMed PMID: 28382259]
Level 3 (low-level) evidenceAwad A, Al-Ali A, Ahmad A, Al-Abdullah H. A suprasellar Aerocele as a Complication of Endoscopic Transsphenoidal Surgery: A Case Report. Ear, nose, & throat journal. 2024 Sep 17:():1455613241276767. doi: 10.1177/01455613241276767. Epub 2024 Sep 17 [PubMed PMID: 39286913]
Level 3 (low-level) evidenceŚmiłowska K, Sznajder-Stacha K, Kocyłowski D, Popek A, Rozpondek K, Grechuta M, Salari M. Pneumocephalus as a rare complication: a systematic review plus clinical vignette. Neurologia i neurochirurgia polska. 2021:55(3):253-268. doi: 10.5603/PJNNS.a2021.0014. Epub 2021 Feb 5 [PubMed PMID: 33543469]
Level 1 (high-level) evidenceBurkhardt E, Savardekar A, Sin A. Traumatic Subarachnoid-Pleural Fistula with Pneumocephalus. World neurosurgery. 2022 Nov:167():229-229.e3. doi: 10.1016/j.wneu.2022.07.080. Epub 2022 Jul 30 [PubMed PMID: 35917920]
Mamani-Rodriguez CE, Goyo Pinto JA, Soler C. [Ventricular and cisternal pneumocephalus secondary to open periorbital trauma]. Medicina. 2024:84(5):1032 [PubMed PMID: 39399954]
Brandvold B, Lee D, Garcon J. Tension Pneumocephalus Caused by a Communicating Pneumothorax via a Nerve Root Avulsion. Cureus. 2024 Aug:16(8):e67317. doi: 10.7759/cureus.67317. Epub 2024 Aug 20 [PubMed PMID: 39301331]
Brueske B, He C, Chauhan V. Devastating Neurological Outcome Following a Subarachnoid-Pleural Fistula During Thoracic Surgery. Cureus. 2024 Apr:16(4):e57838. doi: 10.7759/cureus.57838. Epub 2024 Apr 8 [PubMed PMID: 38721223]
McCarthy S, Villarreal N, Sailor M. Acute Streptococcus pneumoniae Meningitis: A Case Report. AACN advanced critical care. 2024 Sep 15:35(3):244-250. doi: 10.4037/aacnacc2024820. Epub [PubMed PMID: 39213628]
Level 3 (low-level) evidenceGrewal N, Hager K, Pinelo AC, Duddukunta Y, Tolla GG, Gasmelseed H. Unique Presentation of a Ubiquitous Organism: Capnocytophaga canimorsus Meningitis With Pneumocephalus. Cureus. 2024 May:16(5):e59529. doi: 10.7759/cureus.59529. Epub 2024 May 2 [PubMed PMID: 38826958]
Yesilyurt M, Dostbil A, Sakci Z, Ince I, Ogul H. Postpartum intraventricular pneumocephalus following epidural anaesthesia. British journal of hospital medicine (London, England : 2005). 2021 May 2:82(5):1. doi: 10.12968/hmed.2020.0566. Epub 2021 May 3 [PubMed PMID: 34076523]
Lee J, Lee DC. Delayed unilateral pneumocephalus after bilateral endoscopic dacryocystorhinostomy in an elderly patient. BMJ case reports. 2021 May 25:14(5):. doi: 10.1136/bcr-2020-241540. Epub 2021 May 25 [PubMed PMID: 34035023]
Level 3 (low-level) evidenceAlharbi A, Khairy S, Alkhani A. Pneumocephalus after subcutaneous emphysema. Surgical neurology international. 2022:13():249. doi: 10.25259/SNI_994_2021. Epub 2022 Jun 17 [PubMed PMID: 35855157]
Luo L, Tang L, Tan M, Fu W. Intracranial air following spinal anesthesia: A case report. Zhong nan da xue xue bao. Yi xue ban = Journal of Central South University. Medical sciences. 2024 Jun 28:49(6):998-1004. doi: 10.11817/j.issn.1672-7347.2024.230511. Epub [PubMed PMID: 39311796]
Level 3 (low-level) evidenceZhang K, Jia H. Simultaneous gas embolism and pneumocephalus after paravertebral irrigation with hydrogen peroxide: A rare case report. International journal of surgery case reports. 2024 Mar:116():109387. doi: 10.1016/j.ijscr.2024.109387. Epub 2024 Feb 15 [PubMed PMID: 38367418]
Level 3 (low-level) evidencePulickal GG, Sitoh YY, Ng WH. Tension pneumocephalus. Singapore medical journal. 2014 Mar:55(3):e46-8 [PubMed PMID: 24664394]
Level 3 (low-level) evidenceAaron KA, Eltawil Y, Fernandez-Miranda JC, Jackler RK. Spontaneous Otogenic Pneumocephalus Triggered by Air Travel. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2024 Jan 1:45(1):e68-e70. doi: 10.1097/MAO.0000000000004054. Epub [PubMed PMID: 38085769]
Tankersley A, Khan S, Estes K, Paisley C. Non-surgical resolution of pneumocephalus following a sneeze. BMJ case reports. 2024 Sep 25:17(9):. doi: 10.1136/bcr-2024-261096. Epub 2024 Sep 25 [PubMed PMID: 39322573]
Level 3 (low-level) evidenceLopez L, Hauber J, Wyler B. Spontaneous pneumocephalus on the fastest elevator in North America: a case report. CJEM. 2022 Aug:24(5):547-549. doi: 10.1007/s43678-022-00316-x. Epub 2022 May 11 [PubMed PMID: 35543925]
Level 3 (low-level) evidenceJacobs JB, Persky MS. Traumatic pneumocephalus. The Laryngoscope. 1980 Mar:90(3):515-21 [PubMed PMID: 7359973]
Level 3 (low-level) evidenceSteudel WI, Hacker H. Prognosis, incidence and management of acute traumatic intracranial pneumocephalus. A retrospective analysis of 49 cases. Acta neurochirurgica. 1986:80(3-4):93-9 [PubMed PMID: 3716896]
Level 2 (mid-level) evidenceClevens RA, Marentette LJ, Esclamado RM, Wolf GT, Ross DA. Incidence and management of tension pneumocephalus after anterior craniofacial resection: case reports and review of the literature. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1999 Apr:120(4):579-83 [PubMed PMID: 10187965]
Level 3 (low-level) evidenceSweni S, Senthilkumaran S, Balamurugan N, Thirumalaikolundusubramanian P. Tension pneumocephalus: a case report with review of literature. Emergency radiology. 2013 Dec:20(6):573-8. doi: 10.1007/s10140-013-1135-7. Epub 2013 Jun 11 [PubMed PMID: 23748929]
Level 3 (low-level) evidenceMartinez-Nunez AE, Wong JK, Hilliard JD, Foote KD, Okun MS. Preventing Shift from Pneumocephalus During Deep Brain Stimulation Surgery: Don't Give Up the 'Fork in the Brain'. Tremor and other hyperkinetic movements (New York, N.Y.). 2024:14():18. doi: 10.5334/tohm.873. Epub 2024 Apr 10 [PubMed PMID: 38617832]
Cunqueiro A, Scheinfeld MH. Causes of pneumocephalus and when to be concerned about it. Emergency radiology. 2018 Aug:25(4):331-340. doi: 10.1007/s10140-018-1595-x. Epub 2018 Mar 15 [PubMed PMID: 29546674]
Leong KM, Vijayananthan A, Sia SF, Waran V. Pneumocephalus: an uncommon finding in trauma. The Medical journal of Malaysia. 2008 Aug:63(3):256-8 [PubMed PMID: 19248704]
Omer GL, Maurizi R, Velletrani G, Francavilla B, Ali SS, Abdullah AS, Di Girolamo S. Traumatic tension pneumocephalus: a case report and perspective from Indonesia. Frontiers in neurology. 2024:15():1391270. doi: 10.3389/fneur.2024.1391270. Epub 2024 May 3 [PubMed PMID: 38765266]
Level 3 (low-level) evidenceMunakomi S, Bhattarai B, Sah SB. Flapping Scalp Sign as a Rare and Interesting Presentation in Delayed Postoperative Tension Pneumocephalus. JAMA neurology. 2021 Jul 1:78(7):874-875. doi: 10.1001/jamaneurol.2021.1149. Epub [PubMed PMID: 33970209]
Ikeda R, Kikuchi T, Sato S, Oshima H, Kawamura Y, Kusano Y, Kawase T, Katori Y, Kobayashi T. Pulsatile tinnitus caused by pneumocephalus after Janneta surgery. Auris, nasus, larynx. 2021 Aug:48(4):793-796. doi: 10.1016/j.anl.2020.05.024. Epub 2020 Jun 22 [PubMed PMID: 32586740]
Karavelioglu E, Eser O, Haktanir A. Pneumocephalus and pneumorrhachis after spinal surgery: case report and review of the literature. Neurologia medico-chirurgica. 2014:54(5):405-7 [PubMed PMID: 24305016]
Level 3 (low-level) evidenceIshiwata Y, Fujitsu K, Sekino T, Fujino H, Kubokura T, Tsubone K, Kuwabara T. Subdural tension pneumocephalus following surgery for chronic subdural hematoma. Journal of neurosurgery. 1988 Jan:68(1):58-61 [PubMed PMID: 3335913]
Castedo J, Ferreira AP, Camacho Ó. Hyperbaric oxygen therapy in the treatment of pneumocephalus associated with epidural block: case report. Brazilian journal of anesthesiology (Elsevier). 2021 May-Jun:71(3):295-298. doi: 10.1016/j.bjane.2021.02.058. Epub 2021 May 3 [PubMed PMID: 33957186]
Level 3 (low-level) evidenceDexter F, Reasoner DK. Theoretical assessment of normobaric oxygen therapy to treat pneumocephalus. Anesthesiology. 1996 Feb:84(2):442-7 [PubMed PMID: 8602677]
Kim BJH, Ji MY, Chen JCC, Correia JA, Law AJJ, Kow CY. Use of oxygen therapy for pneumocephalus: a systematic review. Neurosurgical review. 2024 Jan 4:47(1):30. doi: 10.1007/s10143-023-02261-4. Epub 2024 Jan 4 [PubMed PMID: 38172487]
Level 1 (high-level) evidenceHarvey JJ, Harvey SC, Belli A. Tension pneumocephalus: the neurosurgical emergency equivalent of tension pneumothorax. BJR case reports. 2016:2(2):20150127. doi: 10.1259/bjrcr.20150127. Epub 2016 May 8 [PubMed PMID: 30363668]
Level 3 (low-level) evidenceArbit E, Shah J, Bedford R, Carlon G. Tension pneumocephalus: treatment with controlled decompression via a closed water-seal drainage system. Case report. Journal of neurosurgery. 1991 Jan:74(1):139-42 [PubMed PMID: 1984495]
Level 3 (low-level) evidenceDoron O, Schneider JR, Ellis JA. Application of the subdural evacuating port system for the drainage of postoperative tension pneumocephalus: A technical note. Surgical neurology international. 2022:13():204. doi: 10.25259/SNI_120_2022. Epub 2022 May 20 [PubMed PMID: 35673650]
Ji KSY, Rimmer R, Dogan A, Cetas JS, Ciporen JN, Sanusi O, Gupta S, Geltzeiler M. Endoscopic Endonasal Eustachian Tube Obliteration as a Treatment for Tension Pneumocephalus After Translabyrinthine Resection of Vestibular Schwannoma. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2022 Sep 1:43(8):e856-e860. doi: 10.1097/MAO.0000000000003606. Epub [PubMed PMID: 35970161]
Moran-Guerrero JA, Martínez HR, Gonzalez-Sanchez DG, Perez-Martinez LE, Flores-Salcido RE, Ferrigno AS, Caro-Osorio E, Salazar-Alejo M, Avalos-Montes PJ, Figueroa-Sanchez JA. Backup Frontal Drainage System for Urgent Tension Pneumocephalus Management After Chronic Subdural Hematoma Surgery: A Retrospective Cohort Study. World neurosurgery. 2024 Aug:188():68-75. doi: 10.1016/j.wneu.2024.04.138. Epub 2024 Apr 29 [PubMed PMID: 38692567]
Level 2 (mid-level) evidenceAljabali A, Serag I, Diab S, Alhadeethi AZ, Abdelhady M, Alkhawaldeh IM, Abouzid M. Irrigation versus no irrigation in the treatment of chronic subdural hematoma: An updated systematic review and meta-analysis of 1581 patients. Neurosurgical review. 2024 Mar 28:47(1):130. doi: 10.1007/s10143-024-02368-2. Epub 2024 Mar 28 [PubMed PMID: 38538863]
Level 1 (high-level) evidenceFujimoto A, Hatano K, Nozaki T, Sato K, Enoki H, Okanishi T. Postoperative Pneumocephalus on Computed Tomography Might Predict Post-Corpus Callosotomy Chemical Meningitis. Brain sciences. 2021 May 15:11(5):. doi: 10.3390/brainsci11050638. Epub 2021 May 15 [PubMed PMID: 34063350]
Mignucci-Jiménez G, Matos-Cruz AJ, Abramov I, Hanalioglu S, Kovacs MS, Preul MC, Feliciano-Valls CE. Puerto Rico Recurrence Scale: Predicting chronic subdural hematoma recurrence risk after initial surgical drainage. Surgical neurology international. 2022:13():230. doi: 10.25259/SNI_240_2022. Epub 2022 Jun 3 [PubMed PMID: 35855136]
Umekawa M, Hasegawa H, Shinya Y, Shin M, Saito N. Incidence of and risk factors for chronic subdural hematoma after endoscopic endonasal surgery: quantitative analysis of pneumocephalus. Journal of neurosurgery. 2024 Aug 1:141(2):484-490. doi: 10.3171/2024.1.JNS231953. Epub 2024 Mar 8 [PubMed PMID: 38457806]
Zhang DY, Pearce JJ, Petrosyan E, Borghei A, Byrne RW, Sani S. Minimizing pneumocephalus during deep brain stimulation surgery. Clinical neurology and neurosurgery. 2024 Mar:238():108174. doi: 10.1016/j.clineuro.2024.108174. Epub 2024 Feb 16 [PubMed PMID: 38422743]
Domino KB, Hemstad JR, Lam AM, Laohaprasit V, Mayberg TA, Harrison SD, Grady MS, Winn HR. Effect of nitrous oxide on intracranial pressure after cranial-dural closure in patients undergoing craniotomy. Anesthesiology. 1992 Sep:77(3):421-5 [PubMed PMID: 1519779]
Level 1 (high-level) evidenceEftekhar B, Ghodsi M, Nejat F, Ketabchi E, Esmaeeli B. Prophylactic administration of ceftriaxone for the prevention of meningitis after traumatic pneumocephalus: results of a clinical trial. Journal of neurosurgery. 2004 Nov:101(5):757-61 [PubMed PMID: 15540912]
Level 1 (high-level) evidenceHuh J. Barotrauma-induced pneumocephalus experienced by a high risk patient after commercial air travel. Journal of Korean Neurosurgical Society. 2013 Aug:54(2):142-4. doi: 10.3340/jkns.2013.54.2.142. Epub 2013 Aug 31 [PubMed PMID: 24175032]
Level 3 (low-level) evidenceLim E, Lan BL, Ooi EH, Low HL. Pneumocephalus and air travel: an experimental investigation on the effects of aircraft cabin pressure on intracranial pressure. Scientific reports. 2020 Aug 12:10(1):13626. doi: 10.1038/s41598-020-70614-w. Epub 2020 Aug 12 [PubMed PMID: 32788610]
Bichsel O, Hauck A, Oertel M. Air travel with pneumocephalus: a systematic review. Acta neurochirurgica. 2022 Sep:164(9):2395-2400. doi: 10.1007/s00701-022-05297-5. Epub 2022 Jul 6 [PubMed PMID: 35794427]
Level 1 (high-level) evidenceAmato-Watkins A, Rao VM, Leach P. Air travel after intracranial surgery: a survey of advice given to patients by consultant neurosurgeons in the UK. British journal of neurosurgery. 2013 Feb:27(1):9-11. doi: 10.3109/02688697.2012.716176. Epub 2012 Aug 30 [PubMed PMID: 22931355]
Level 3 (low-level) evidence