Introduction
The vast majority of tumors of the peripheral nervous system arise from the cells of Schwann, rather than from the nerve cells themselves. Schwann cells, or neurilemma, are cells that are responsible for the production of the myelin sheath around neuronal axons. Most of these tumors are benign and designated as "schwannomas" or "neurilemmomas," and may appear spontaneously as solitary lesions, or as part of an underlying clinical condition such as neurofibromatosis. These vast majority of these tumors are slow-growing, encapsulated tumors of these Schwann cells within a collagenous matrix.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Neurilemmomas arise from the cells of Schwann and may occur spontaneously, or in conjunction with clinical syndromes such as neurofibromatosis type 2, Schwannomatosis, and Carney complex.[1]
Epidemiology
Vestibular neurilemmomas were found to have an incidence ranging from 0.01% to 0.1% in the general population with a peak age of 20 to 50, without a clear preference for sex.[2] In an autopsy study of elderly patients with neurofibromatosis type 2, the incidence of sporadic central schwannoma was found to be much higher at 4.5%.[1][3][4][5][6]
Histopathology
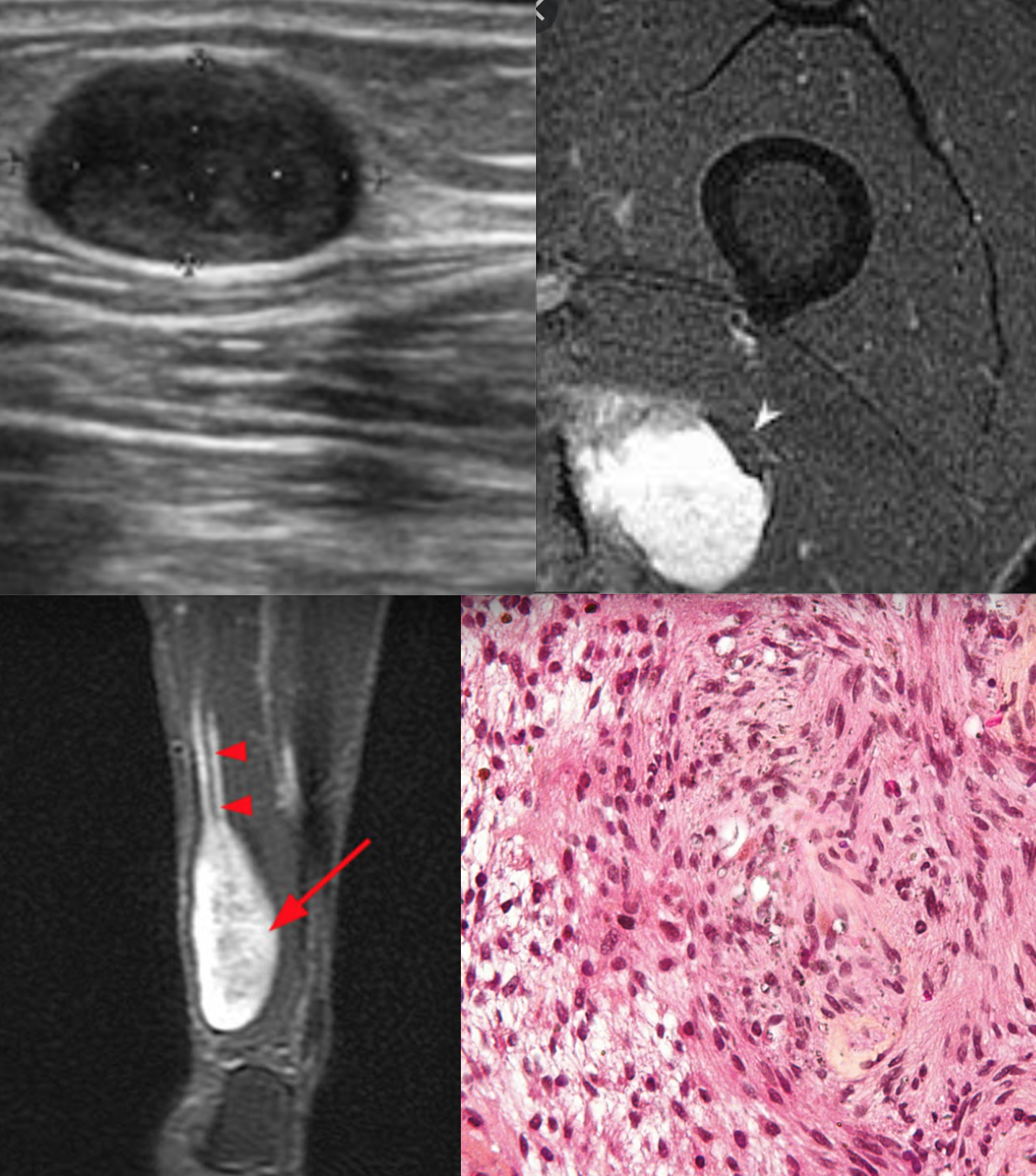
Histologic examination of the well-circumscribed neurilemmoma shows degenerative changes and a variable presentation of compact spindles, referred to as "Antoni A" bodies and microcystic areas with a high concentration of macrophages and collagen fibers, designated as "Antoni B" bodies. Additionally, nuclear palisading around cell bodies is described as Verocay bodies and is strongly suggestive of neurilemmomas. Schwannomas classically stain strongly for S100 protein expression on immunohistochemistry and will have pericellular type IV collagen in abundance. Glial fibrillary acid protein (GFAP), podoplanin, calretinin, and SOX10 may be present in varying degrees within different subtypes of neurilemmomas.[7][8][9][10]
History and Physical
Patients with a neurilemmoma typically present with an asymptomatic mass but may experience pain and paresthesias throughout the distribution of the entire nerve as the tumor grows larger and applies pressure to the nerve. Neurilemmomas of the posterior spinal nerve will produce sensory symptomatology, while compression of the anterior spinal nerves may produce motor deficits.
On physical exam, physicians may notice a palpable mass that can be mobilized in the plane orthogonal to the axis of the affected nerve, but not longitudinally aligned with the affected nerve.
Neurilemmomas most frequently occur in the neck and mediastinum, and when present in the extremities are far more common along the flexor surfaces.[1][11]
Evaluation
On CT scans, neurilemmomas are hypodense compared to muscle and enhance with contrast. On MRI, neurilemmomas are isointense to muscle on T1-weighted imaging and bright on T2-weighted imaging with occasional low signal cysts. While inconsistent, the best way to distinguish a neurilemmoma from a neurofibroma is an eccentric displacement of the nerve and heterogeneous appearance with cystic degeneration, suggestive of a schwannoma.[2][12]
Biopsy of the neoplasm, as discussed above, is the best way to confirm a diagnosis of a schwannoma, with a defined fibrous capsule and Antoni A and Antoni B bodies on histology.[13]
Treatment / Management
Neurilemmomas and neurofibromas can often be managed non-operatively, with observation if asymptomatic or causing minimal symptoms. If there is a concern for malignancy or are symptoms causing distress, surgery is the mainstay of intervention. The goal of any surgical treatment is the removal of the tumor without neurological impairment. Removing neurilemmomas without damaging the nerve is easier than in the removal of a neurofibroma due to the fibrous capsule containing neurilemmomas.[14][15][16](B3)
Electrophysiologic monitoring is important during the removal of neurilemmomas. A longitudinal incision is marked over the tumor site, allowing for exposure of normal nerve proximal and distal to the tumor. Using vessel loops, the healthy nerve is wrapped proximal and distal to the tumor, and the nerve is carefully dissected away from the tumor capsule using Metzenbaum scissors. The tumor is generally removed as a solitary mass when possible.[17]
Differential Diagnosis
Solitary neurofibromas are benign peripheral nerve tumors that also arise from cells of Schwann that more classically involve the skin or subcutaneous tissue. Like neurilemmomas, neurofibromas are very slow-growing tumors but differ in their histology in that they are not encapsulated as neurilemmomas are. Histopathologically compared to neurofibromas, and protein staining is classically limited to peripheral axons in neurilemmomas.[7][18]
Prognosis
In a study by Kim et al., patients that underwent surgical removal of neurilemmomas in the brachial plexus who had full strength pre-operatively maintained their normal strength in 88% of cases. 90% of those who had post-operative weakness had strength that was either improved or unchanged from their preoperative examination.[17] In another series by Young et al., 52% of patients who underwent resection had resolution of their symptoms, with 18% having improved symptoms.[19]
Complications
Neurilemmomas of the extremities are typically asymptomatic and only create a mass. Sometimes, however, the mass effect of the neoplasm can cause dysfunction of the nerve. While most symptoms are pain in the distribution of the nerve and sensory deficits or paresthesias, neurilemmomas of the anterior nerves of the spinal cord may produce symptoms of weakness and motor dysfunction as well.
If excised surgically, neurilemmomas are typically removed without damage to the nerve, as the tumor is derived from the surrounding cells of Schwann and not directly from the nerve axon themselves. That being said, any surgery carries risk. Injury to the nerve itself is uncommon, but always a possibility through traction injuries or disruption of the axon. As with all surgery, wound complications may occur as well. Recurrence is possible, but rare in benign tumors of the nerve sheath.
Deterrence and Patient Education
Neurilemmomas are benign findings, and while they can produce symptoms due to mass effects on surrounding tissues, they generally are not a cause for concern. If a patient experiences pain or neurologic deficit, disfigurement, bleeding, or if there is suspicion for a developing malignancy, surgery may be indicated. Surgical intervention does yield very favorable outcomes, with some expected risk of associated nerve damage.
Enhancing Healthcare Team Outcomes
Appropriate management of neurilemmomas requires a cooperative effort of the interdisciplinary healthcare team. Any mass of unknown etiology should be evaluated by an appropriate healthcare professional. First-line providers should have a basic knowledge of benign nerve sheath tumors to order appropriate testing and help patients choose the best course of management. Referral to specialists such as neurologists and surgeons as appropriate will also be critical for the appropriate monitoring of tumors and guiding the patient towards an optimal outcome.
As always, the cooperation of the entire medical team is critical. Nurses and office staff must be comfortable in their working environment to provide the best possible care, and communication is key to enacting the agreed-upon plan of management. Furthermore, if surgical intervention is required, operating room nurses and staff must be familiar with standard surgical procedures and comfortable with executing the operative plan. [Level 5]
Media
References
Hilton DA, Hanemann CO. Schwannomas and their pathogenesis. Brain pathology (Zurich, Switzerland). 2014 Apr:24(3):205-20. doi: 10.1111/bpa.12125. Epub 2014 Feb 25 [PubMed PMID: 24450866]
Level 3 (low-level) evidencePilavaki M, Chourmouzi D, Kiziridou A, Skordalaki A, Zarampoukas T, Drevelengas A. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. European journal of radiology. 2004 Dec:52(3):229-39 [PubMed PMID: 15544900]
Evans DG, Moran A, King A, Saeed S, Gurusinghe N, Ramsden R. Incidence of vestibular schwannoma and neurofibromatosis 2 in the North West of England over a 10-year period: higher incidence than previously thought. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2005 Jan:26(1):93-7 [PubMed PMID: 15699726]
Level 2 (mid-level) evidenceLin D, Hegarty JL, Fischbein NJ, Jackler RK. The prevalence of "incidental" acoustic neuroma. Archives of otolaryngology--head & neck surgery. 2005 Mar:131(3):241-4 [PubMed PMID: 15781765]
Level 2 (mid-level) evidencePropp JM, McCarthy BJ, Davis FG, Preston-Martin S. Descriptive epidemiology of vestibular schwannomas. Neuro-oncology. 2006 Jan:8(1):1-11 [PubMed PMID: 16443943]
Tos M, Stangerup SE, Cayé-Thomasen P, Tos T, Thomsen J. What is the real incidence of vestibular schwannoma? Archives of otolaryngology--head & neck surgery. 2004 Feb:130(2):216-20 [PubMed PMID: 14967754]
Rodriguez FJ, Folpe AL, Giannini C, Perry A. Pathology of peripheral nerve sheath tumors: diagnostic overview and update on selected diagnostic problems. Acta neuropathologica. 2012 Mar:123(3):295-319. doi: 10.1007/s00401-012-0954-z. Epub 2012 Feb 12 [PubMed PMID: 22327363]
Level 3 (low-level) evidenceWeiss SW, Langloss JM, Enzinger FM. Value of S-100 protein in the diagnosis of soft tissue tumors with particular reference to benign and malignant Schwann cell tumors. Laboratory investigation; a journal of technical methods and pathology. 1983 Sep:49(3):299-308 [PubMed PMID: 6310227]
Ogawa K, Oguchi M, Yamabe H, Nakashima Y, Hamashima Y. Distribution of collagen type IV in soft tissue tumors. An immunohistochemical study. Cancer. 1986 Jul 15:58(2):269-77 [PubMed PMID: 3521829]
Kawahara E, Oda Y, Ooi A, Katsuda S, Nakanishi I, Umeda S. Expression of glial fibrillary acidic protein (GFAP) in peripheral nerve sheath tumors. A comparative study of immunoreactivity of GFAP, vimentin, S-100 protein, and neurofilament in 38 schwannomas and 18 neurofibromas. The American journal of surgical pathology. 1988 Feb:12(2):115-20 [PubMed PMID: 3124642]
Level 2 (mid-level) evidencePerry A, Roth KA, Banerjee R, Fuller CE, Gutmann DH. NF1 deletions in S-100 protein-positive and negative cells of sporadic and neurofibromatosis 1 (NF1)-associated plexiform neurofibromas and malignant peripheral nerve sheath tumors. The American journal of pathology. 2001 Jul:159(1):57-61 [PubMed PMID: 11438454]
Crist J, Hodge JR, Frick M, Leung FP, Hsu E, Gi MT, Venkatesh SK. Magnetic Resonance Imaging Appearance of Schwannomas from Head to Toe: A Pictorial Review. Journal of clinical imaging science. 2017:7():38. doi: 10.4103/jcis.JCIS_40_17. Epub 2017 Oct 3 [PubMed PMID: 29114437]
Skovronsky DM, Oberholtzer JC. Pathologic classification of peripheral nerve tumors. Neurosurgery clinics of North America. 2004 Apr:15(2):157-66 [PubMed PMID: 15177315]
Golan JD, Jacques L. Nonneoplastic peripheral nerve tumors. Neurosurgery clinics of North America. 2004 Apr:15(2):223-30 [PubMed PMID: 15177321]
Bhattacharyya AK, Perrin R, Guha A. Peripheral nerve tumors: management strategies and molecular insights. Journal of neuro-oncology. 2004 Aug-Sep:69(1-3):335-49 [PubMed PMID: 15527099]
Mrugala MM, Batchelor TT, Plotkin SR. Peripheral and cranial nerve sheath tumors. Current opinion in neurology. 2005 Oct:18(5):604-10 [PubMed PMID: 16155448]
Level 3 (low-level) evidenceKim DH, Murovic JA, Tiel RL, Kline DG. Operative outcomes of 546 Louisiana State University Health Sciences Center peripheral nerve tumors. Neurosurgery clinics of North America. 2004 Apr:15(2):177-92 [PubMed PMID: 15177317]
Nascimento AF, Fletcher CD. The controversial nosology of benign nerve sheath tumors: neurofilament protein staining demonstrates intratumoral axons in many sporadic schwannomas. The American journal of surgical pathology. 2007 Sep:31(9):1363-70 [PubMed PMID: 17721192]
Young ED, Ingram D, Metcalf-Doetsch W, Khan D, Al Sannaa G, Le Loarer F, Lazar AJF, Slopis J, Torres KE, Lev D, Pollock RE, McCutcheon IE. Clinicopathological variables of sporadic schwannomas of peripheral nerve in 291 patients and expression of biologically relevant markers. Journal of neurosurgery. 2018 Sep:129(3):805-814. doi: 10.3171/2017.2.JNS153004. Epub 2017 Sep 8 [PubMed PMID: 28885122]