Introduction
Osgood Schlatter disease, also known as osteochondrosis or traction apophysitis of the tibial tubercle, is a common cause of anterior knee pain in the skeletally immature athletic population. Common sports seen in association with the condition include:
- Basketball
- Volleyball
- Sprinters
- Gymnastics
- Football
Clinical presentation classically associates atraumatic, insidious onset of anterior knee pain, with tenderness at the patellar tendon insertion site at the tibial tuberosity. The condition is self-limited and occurs secondary to repetitive extensor mechanism stress activities such as jumping and sprinting. Pain level dictates overall treatment, and management includes symptomatic treatment with ice and NSAIDs, as well as activity modification and relative rest from inciting activities in association with lower extremities stretching regimen to correct underlying predisposing biomechanical factors.[1][2][3][4]
Even though the disorder is benign, the recovery can be prolonged and cause absence from sports. The onset of the disorder is gradual and commonly associated with repetitive activities of the knee. There is usually tenderness over the tibial tubercle.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The patellar tendon inserts at the tibial tubercle and consists of cartilaginous tissue. This is followed by ossification of the tibial tubercle at ages 10-12 in girls and at ages 12-14 in boys. It is during this stage of bone maturation when Osgood Schlatter disease develops. The prevailing theory is that there is repeated traction over the tubercle leading to microvascular tears, fractures, and inflammation; which then presents as swelling, pain, and tenderness.
Osgood Schlatter disease is an overuse injury that occurs in active adolescent patients. It occurs secondary to repetitive strain and microtrauma from the force applied by the strong patellar tendon at its insertion into the relatively soft apophysis of the tibial tubercle. This force results in irritation and severe cases partial avulsion of the tibial tubercle apophysis. Force is increased with higher levels of activity and especially after periods of rapid growth. Rarely trauma may lead to a full avulsion fracture. Predisposing factors include poor flexibility of quadriceps and hamstrings or other evidence of extensor mechanism misalignment.[5][6][7]
Risk factors for the disorder include:
- Male gender
- Ages: male 12-15, girls 8-12
- Sudden skeletal growth
- Repetitive activities like jumping and sprinting
Epidemiology
Osgood Schlatter disease is one of the most common causes of knee pain in the skeletally immature, adolescent athlete. Onset coincides with adolescent growth spurts between ages 10 to 15 years for males and 8 to 13 years for females. The condition is more common in males and occurs more frequently in athletes that participate in sports that involve running and jumping. In adolescents, age 12 to 15, the prevalence of Osgood Schlatter disease is 9.8% (11.4% in males, 8.3% in females). Symptoms present bilaterally in 20% to 30% of patients.[8][9]
Pathophysiology
The tibial tubercle develops as a secondary ossification center that provides attachment for the patellar tendon. Bone growth exceeds the ability of the muscle-tendon unit to stretch sufficiently to maintain previous flexibility leading to increased tension across the apophysis. The physis is the weakest point in the muscle-tendon-bone-attachment (as opposed to the tendon in an adult) and therefore, at risk of injury from repetitive stress. With repeated contraction of the quadriceps muscle mass, especially with repeated forced knee extension as seen in sports requiring running and jumping (basketball, football, gymnastics), softening and partial avulsion of the apophyseal ossification center may occur with a resulting osteochondritis.[3]
The appearance and closure/fusion of the tibial tubercle occurs in the following sequence pattern:
- Tibial tubercle is entirely cartilagenous (age < 11 years)
- Apophysis forms (age 11 to 14 years)
- Apophysis fuses with the proximal tibial epiphysis (age 14 to 18 years)
- The proximal tibial epiphysis and tibial tubercle apophysis fuses with the rest of the proximal tibia (age > 18 years) [7][8][10][11]
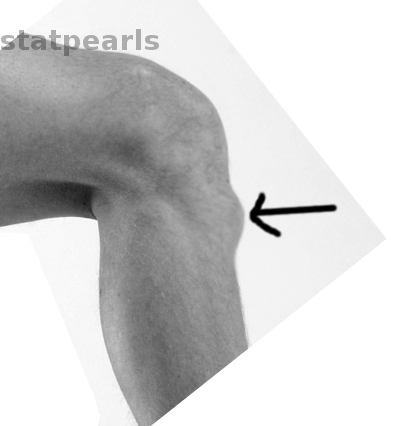
History and Physical
An 8 to 15-year-old child will typically present with anterior knee pain with or without swelling which can be unilateral or bilateral. Pain begins as a dull ache localized over tibial tubercle gradually increasing with activity. The presentation is typical of insidious onset without preceding trauma. Pain typically improves with rest and will subside minutes to hours after the inciting activity or sport is stopped. Pain is exacerbated particularly by running, jumping, direct knee trauma, kneeling, and squatting. An enlarged prominence at the tibial tubercle is present with tenderness over the site of patellar tendon insertion. Poor flexibility of quadriceps and hamstrings may be present as predisposing factors. Pain may be reproduced by resisted knee extension and active or passive knee flexion. [1][5] [10][12]
Evaluation
Osgood Schlatter disease is a clinical diagnosis, and radiographic evaluation is usually not necessary. Plain radiographs may be used to rule out additional diagnoses such as fracture, infection, or bone tumor if the presentation is severe or atypical. The radiographic evaluation may also be indicated to evaluate for avulsion injury of the apophysis or other injuries after a traumatic event. Classic radiographic findings in Osgood-Schlatter disease include an elevated tibial tubercle with soft tissue swelling, fragmentation of the apophysis, or calcification in the distal patellar tendon. It is worth noting that these findings can also be seen as normal variants and do not always represent pathology, so clinical correlation is of utmost importance. If ordering radiographs consider comparing bilateral images to delineate normal versus abnormal in the individual patient. [1][5] [10][12]
Treatment / Management
Ultimately, the condition is self-limiting but may persist for up to 2 years until the apophysis fuses. Treatment includes relative rest and activity modification from the offending activity as guided by the level of pain. There is no evidence to suggest that rest speeds up recovery, but activity restriction is effective in reducing pain. Patients may participate in sports as long as the pain resolves with rest and does not limit sports-associated activities. Local application of ice and NSAIDs can be used for pain relief. A protective knee pad may be worn over tibial tubercle to protect from direct trauma. Hamstring stretching and both quadriceps stretching and strengthening exercises can be a useful adjunct. If the pain does not respond to conservative measures, formal physical therapy may be warranted. In severe, prolonged cases a short period of knee immobilization may be considered. There is no evidence to recommend injection therapy or surgical intervention for Osgood-Schlatter disease. Symptoms typically are self-limiting with a resolution of pain upon closure of the apophysis. Long-term sequelae may include a thickened or prominent tibial tubercle, but this is asymptomatic in the vast majority of cases.[10][11][12][4][6](A1)
Refractory Cases
In up to 10% of cases, symptoms may persist >1-2 years beyond skeletal maturity. In skeletally mature patients with persistent symptoms, ossicle excision may be performed.
Surgery is rarely indicated for the disorder but may be undertaken to excise the overlying bursa. Overall, surgery does not offer any more benefit than medical treatment and is more likely to cause complications.
Differential Diagnosis
- Patella tendonitis
- Osteomyelitis of the tibia
- Perthes disease
- Synovial plica injury
- Infectious apophysitis
Prognosis
The prognosis of Osgood-Schlatter disease is excellent. The disorder is self limiting but time to resolution can take months. In about 10% of patients, the symptoms may continue into adulthood. This long term sequelae occurs when the individual does not seek treatment or has poor compliance with the recommended treatment. There are reported cases when the pain may last several years.
Complications
Prominence of tibital tubercle
Ongoing pain
Enhancing Healthcare Team Outcomes
Osgood Schlatter disease is best managed by an interprofessional team that includes a sports physician, physical therapist, primary care provider, orthopedic nurse and an orthopedic surgeon.
As these injuries often present in extremely active adolescent patients, it may be effective to decrease the amount of athletic participation rather than cease activity altogether. For example, in a patient that participates in multiple sports or on multiple teams during the same season, it may be effective to recommend that the patient eliminates one of these teams or sports to decrease the amount of activity and strain that occurs with frequent and recurrent participation as opposed to complete rest. The decision to limit activity should be a shared decision including short term and long term goals of the both patient athlete and parent. Ultimately the decision should be driven by the level of pain experienced. Preventative measures for Osgood Schlatter include recommending a gradual increase in workload (less than 10% per week), using appropriate equipment and techniques, include stretching regimen to ensure flexibility in hamstrings and quadriceps, and consider avoiding early sports specialization. [1][10][12]
Outcomes
The condition is self-limiting but may persist for up to 2 years until the apophysis fuses. Treatment includes relative rest and activity modification from the offending activity as guided by the level of pain.
If pain does not respond to conservative measures, formal physical therapy may be warranted. In severe, prolonged cases a short period of knee immobilization may be considered. There is no evidence to recommend injection therapy or surgical intervention for Osgood-Schlatter disease.
While recovery is slow, most patients are eventually free of pain.[6] [1][10][12]
Media
(Click Image to Enlarge)
References
Rathleff MS, Straszek CL, Blønd L, Thomsen JL. [Knee pain in children and adolescents]. Ugeskrift for laeger. 2019 Mar 25:181(13):. pii: V01180081. Epub [PubMed PMID: 30935452]
Murphy CE, Kenny CM. Not just for boys: a rare case of symptomatic Osgood-Schlatter disease in a skeletally mature woman. BMJ case reports. 2019 Mar 26:12(3):. doi: 10.1136/bcr-2018-228963. Epub 2019 Mar 26 [PubMed PMID: 30914412]
Level 3 (low-level) evidenceSeyfettinoğlu F, Köse Ö, Oğur HU, Tuhanioğlu Ü, Çiçek H, Acar B. Is There a Relationship between Patellofemoral Alignment and Osgood-Schlatter Disease? A Case-Control Study. The journal of knee surgery. 2020 Jan:33(1):67-72. doi: 10.1055/s-0038-1676523. Epub 2018 Dec 21 [PubMed PMID: 30577051]
Level 2 (mid-level) evidenceSiddiq MAB. Osgood-Schlatter Disease Unveiled Under High-frequency Ultrasonogram. Cureus. 2018 Oct 4:10(10):e3411. doi: 10.7759/cureus.3411. Epub 2018 Oct 4 [PubMed PMID: 30538899]
Hart E, Meehan WP 3rd, Bae DS, d'Hemecourt P, Stracciolini A. The Young Injured Gymnast: A Literature Review and Discussion. Current sports medicine reports. 2018 Nov:17(11):366-375. doi: 10.1249/JSR.0000000000000536. Epub [PubMed PMID: 30407945]
Midtiby SL, Wedderkopp N, Larsen RT, Carlsen AF, Mavridis D, Shrier I. Effectiveness of interventions for treating apophysitis in children and adolescents: protocol for a systematic review and network meta-analysis. Chiropractic & manual therapies. 2018:26():41. doi: 10.1186/s12998-018-0209-8. Epub 2018 Oct 23 [PubMed PMID: 30386556]
Level 1 (high-level) evidenceWatanabe H, Fujii M, Yoshimoto M, Abe H, Toda N, Higashiyama R, Takahira N. Pathogenic Factors Associated With Osgood-Schlatter Disease in Adolescent Male Soccer Players: A Prospective Cohort Study. Orthopaedic journal of sports medicine. 2018 Aug:6(8):2325967118792192. doi: 10.1177/2325967118792192. Epub 2018 Aug 28 [PubMed PMID: 30182029]
Indiran V, Jagannathan D. Osgood-Schlatter Disease. The New England journal of medicine. 2018 Mar 15:378(11):e15. doi: 10.1056/NEJMicm1711831. Epub [PubMed PMID: 29539285]
Nkaoui M, El Alouani EM. Osgood-schlatter disease: risk of a disease deemed banal. The Pan African medical journal. 2017:28():56. doi: 10.11604/pamj.2017.28.56.13185. Epub 2017 Sep 21 [PubMed PMID: 29230258]
Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW. Osgood Schlatter syndrome. Current opinion in pediatrics. 2007 Feb:19(1):44-50 [PubMed PMID: 17224661]
Level 3 (low-level) evidenceItoh G, Ishii H, Kato H, Nagano Y, Hayashi H, Funasaki H. Risk assessment of the onset of Osgood-Schlatter disease using kinetic analysis of various motions in sports. PloS one. 2018:13(1):e0190503. doi: 10.1371/journal.pone.0190503. Epub 2018 Jan 8 [PubMed PMID: 29309422]
Patel DR, Villalobos A. Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Translational pediatrics. 2017 Jul:6(3):190-198. doi: 10.21037/tp.2017.04.05. Epub [PubMed PMID: 28795010]