Introduction
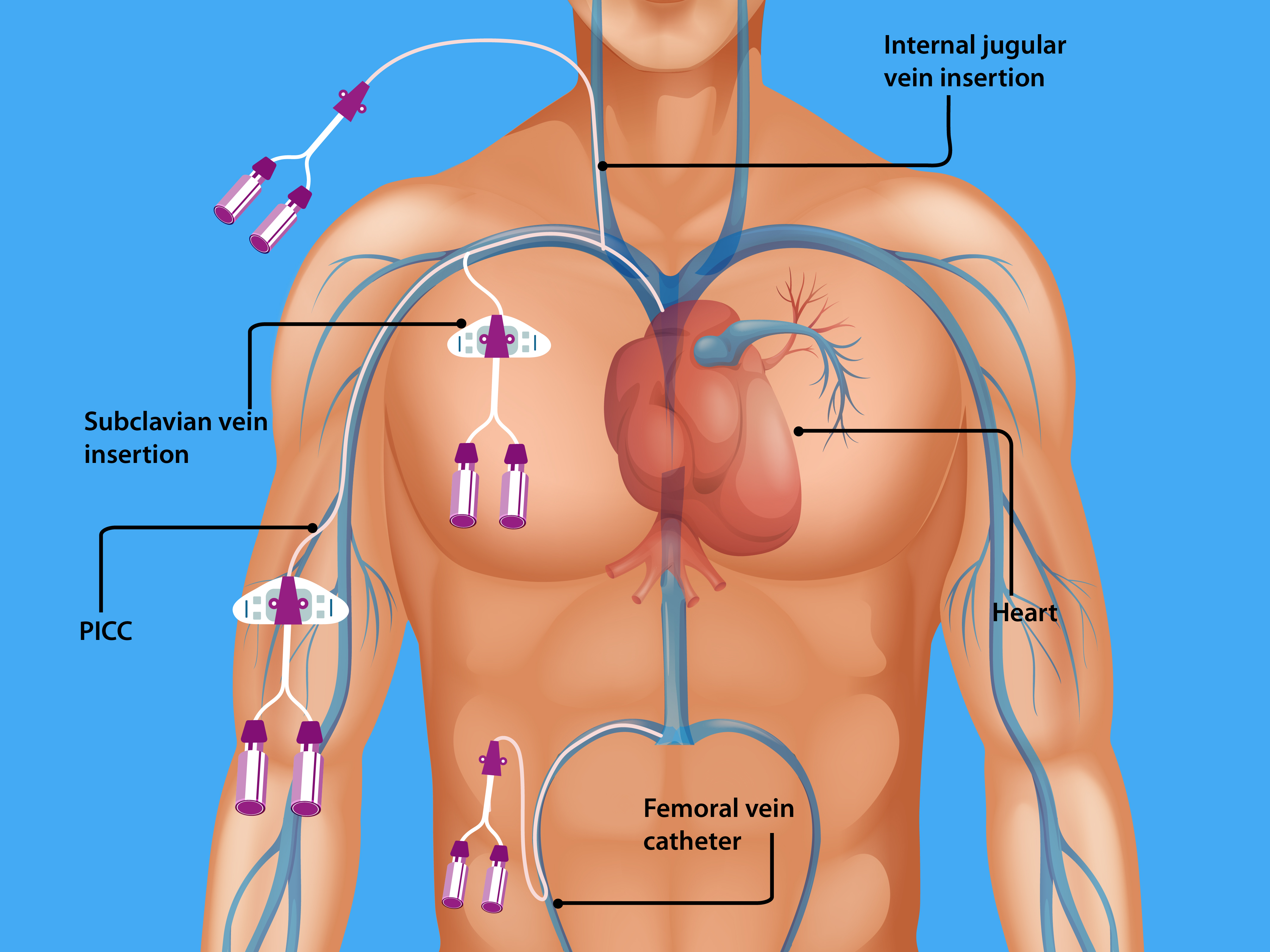
A central venous catheter (CVC) is an indwelling device inserted into a large, central vein (most commonly the internal jugular, subclavian, or femoral) and advanced until the terminal lumen resides within the inferior vena cava, superior vena cava, or right atrium. These devices and the techniques employed to place them are synonymous with "central line", “central venous line” (CVL), or "central venous access." The placement of a CVC was first described in 1929.[1] Over the following decades, central venous access rapidly developed into an essential experimental instrument for studying cardiac physiology and an indispensable clinical tool in treating many disease processes.[2]
Various access techniques and devices were developed for many indications, including total parenteral nutrition administration, dialysis, plasmapheresis, medication administration, and hemodynamic monitoring, and to facilitate further complex interventions such as transvenous pacemaker placement.[1][3][4][5][6][7]
Despite these advancements, the procedure has remained relatively unchanged since the advent of the (now universally employed) Seldinger technique in the 1960s.[8] A notable exception is the adjunct of ultrasound guidance, which has recently become the standard of care for CVCs placed in the internal jugular vein, owing to associated decreases in complications and an increase in first-pass success.[5][9][10][11][12][13] Some controversy persists about the merits of specific site selection (e.g., which vein) and the relative associated complication rates of CVCs placed in different central veins. However, there is broad consensus that today, in the modern era, the competency to establish and manage a central venous catheter is an indisputably essential skill set for clinicians involved in the care of critically ill patients. The purpose of this article is to review the indications, contraindications, techniques, complications, and management of centrally placed venous catheters.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
There are various access sites for the placement of central venous catheters.The internal jugular, common femoral, and subclavian veins are the preferred sites for temporary prominent venous catheter placement, whereas the basilic and brachial veins are primarily utilized for mid-term and long-term central venous access in the form of peripherally inserted central catheters (PICCs). A discussion of tunneled catheters and other central access obtained via advanced interventional radiology techniques is beyond the scope of this article. We will focus on the three main sites of access routinely used for short-term, or temporary(days to weeks), central access.
Understanding the relevant anatomy and adjacent structures is crucial when placing a CVC. The decision of where to place a central line is typically based on clinical parameters and individual clinician experience and preference. Each anatomical site has relative advantages and disadvantages; placement selection is largely driven by an individual patient’s clinical history.
The internal jugular vein (IJ) is often chosen for its reliable anatomy, accessibility, low complication rates, and ability to employ ultrasound guidance during the procedure.[9] The individual clinical scenario may dictate laterality in some cases (such as with trauma, history of head and neck cancer, or the presence/history of other invasive devices or catheters). In the standard patient, the right IJ is the preferred access as it allows a more direct path to the superior vena cava (SVC) and right atrium. It is also wider and more superficial, thus presumably easier to cannulate.[14]
The IJ is located anterolateral to the common carotid artery, typically in the superior portion of the triangle created by the two heads of the sternocleidomastoid (SCM) muscle and the clavicle. The internal jugular vein joins the subclavian vein to form the brachiocephalic vein. The right and left brachiocephalic veins join to form the SVC. When anatomic landmarks are used, the IJ site can be accessed anteriorly, centrally, or posteriorly about the bifurcation of the SCM. Generally speaking, the central approach is most commonly used. Still, some have argued that the posterior approach is safest (being furthest from the lung apex and the carotid artery) and that the anterior approach is the easiest (as the carotid artery forms a readily palpable reference landmark). While there may still be no consensus about the correct landmark-based approach, most experts agree that ultrasound guidance provides the best chance of locating the vein and avoiding other structures owing to anatomic variability.[15][16]
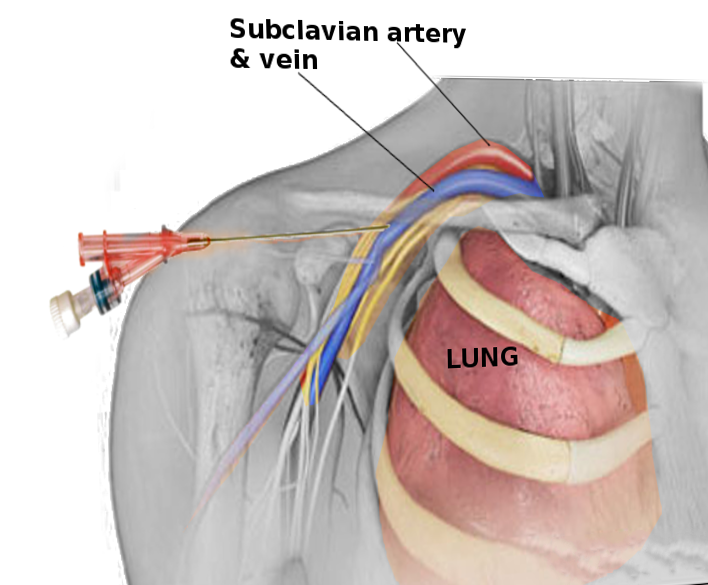
The subclavian vein site has the advantage of low rates of both infectious and thrombotic complications.[17] Additionally, the SC site is accessible in trauma when a cervical collar negates the choice of the IJ. However, disadvantages include a higher relative risk of pneumothorax, less accessibility to use ultrasound for CVC placement, and the non-compressible location posterior to the clavicle. At the site of puncture for CVC placement, the subclavian vein lies just posterior to the clavicle. Still, the vessel takes a tortuous route as it extends medially from the axillary vein. As the vein courses along the clavicle, from lateral to medial, it progresses from the lateral border of the first rib, slopes cephalad at the middle third of the clavicle, then caudally merges with the internal jugular vein just posterior to the sternoclavicular joint. Of note, the subclavian vein is closely associated with several important structures. The vein is typically anterior and superior to the subclavian artery. The lung is just inferomedially to the subclavian vein, in close approximation to the lateral first rib. The phrenic nerve courses just deep to the brachiocephalic vein at the confluence of the subclavian vein and internal jugular vein. The brachial plexus and right-sided thoracic duct are also nearby and vulnerable to injury.[18] While ultrasound (US) guidance methods have been documented, access at this site is often performed without US guidance in a landmark-guided technique.[19] Data suggests that US guidance may reduce the rates of arterial puncture, pneumothorax, and brachial plexus injury; however, many clinicians are still more comfortable with landmark-guided placement for SC central venous catheters.[16][20][21][22]
The SC vein can be accessed above or below the clavicle, though the infraclavicular method is far more commonly employed. The supraclavicular approach offers a well-defined landmark for insertion at the clavisternomastoid angle, a shorter distance from a puncture to the vein, and a straighter path to the SVC, with less proximity to the lung.[22] Authors have used these findings and the observation that ultrasound guidance is easier to perform with the supraclavicular approach to suggest that the infraclavicular approach should no longer be the SC CVC insertion method.[23] However, other studies have found that the supraclavicular approach leads to a higher incidence of hematoma formation, with comparable rates of other complications, offering support for maintaining the status quo.[24]
The femoral site is sometimes preferable in critically ill patients because the groin is free of other resuscitation equipment and devices which may be required for monitoring and airway access. Central venous access in the common femoral vein offers the advantage of being an easily compressible site, which may be helpful in trauma and other coagulopathic patients.[25] Additionally, unlike the IJ and SC sites, iatrogenic pneumothorax is not a concern. Patients may be more comfortable with a femoral CVC because it allows relatively free movement of the arms and legs compared to other sites. However, femoral CVCs are typically associated with increased thrombotic complications and likely an increased rate of catheter-associated infections. However, studies have shown conflicting results about the real risk of infection when the proper sterile technique is used.[5][26][27][28]
Unlike IJ or SC lines, femoral central lines do not allow for accurate measurement of central venous pressure (CVP), though this is not important in every clinical scenario. The common femoral vein is located within the femoral triangle. This region is outlined by the adductor longus medially, sartorius muscle laterally, and the inguinal ligament superiorly. There are important anatomical considerations to keep in mind when accessing this particular site. Whereas in the neck, the (carotid) artery is medial to the (internal jugular) vein, the artery is lateral to the vein in the leg. The mnemonic NAVEL is useful for recalling the order of lateral to medial structures: femoral nerve, femoral artery, common femoral vein, "space" (femoral canal), and lymphatics.[29] Knowing this anatomy or landmark-guided central line placement band is important because ultrasonography may appear similar.[11]
Indications
Central lines are placed for the following indications:
- Hemodynamic instability that requires vasopressor support
- Need for hemodynamic monitoring, including central venous pressure
- Need to instill hyperosmolar agents or agents known to cause vein scarring (phlebosclerosis)
- Inadequate peripheral IV access (either failure to obtain peripheral access in urgent/emergent situations, or requirement of multiple IVs to sustain and resuscitate a patient)
- Initiation of high fluid volume extracorporeal therapies, such as hemodialysis plasmapheresis, or continuous renal replacement therapy
- Initiation of multiple infusions that may be incompatible with peripheral intravenous access, including total parenteral nutrition, chemotherapy, and other acidic medications to peripheral veins
- Mass transfusion protocol in patients with inadequate peripheral access
- Venous interventions, including inferior vena cava filter placement, thrombolytic therapy, transvenous cardiac pacing, and intra-venous stenting
Contraindications
There are relative and absolute contraindications to placing central venous catheters, and contraindications may be site-specific. Relative contraindications may be overruled by the urgency with which the catheter needs to be identified and thus require careful consideration of the patient’s underlying pathology and hemodynamic status.
Absolute contraindications:
- Active skin or soft tissue infection at the potential site of the central line.
- Anatomical distortion at the site includes implantable/indwelling hardware, such as hemodialysis catheters and pacemakers.
- Vascular injury proximal or distal to the site of the catheter insertion, such as in traumatic injuries.
Relative contraindications:
- Coagulopathy, though the actual incidence of clinically significant bleeding is around 0.8%.[30]
- Thrombocytopenia seems to correlate with a greater risk of adverse events.
- Uncooperative awake patient.
- Distortion of landmarks by congenital anomalies or trauma.
- Morbid obesity.
Typically, patients with an international normalized ratio (INR) of greater than 3.0 or platelets less than 20 x 10^9/L have severe coagulopathy and an increased risk of bleeding.[31] It may be warranted to consider giving fresh frozen plasma and platelets before the procedure or shortly after that, depending on the urgency of the clinical situation. Site-specific contraindications must be assessed on a case-by-case basis. The SC site is contraindicated in coagulopathic patients, given its anatomical proximity to several other significant vessels and the inability of the proceduralist to hold pressure in the event of an accidental arterial puncture or laceration of the vein itself. The IJ site may be relatively contraindicated if a cervical collar is in place or if the IJ site will be required for another invasive procedure during the same admission. Similarly, the femoral site should be avoided if it is anticipated that femoral access will be needed for a procedure such as cardiac catheterization.
Equipment
Various manufacturers of central venous catheter insertion kits and several different types of catheters exist. Generally speaking, one will require an ultrasound machine with a high-frequency linear transducer, sterile products, mask, and head covering, the introducer kit with a central venous catheter, lidocaine, various sterile syringes, sterile saline flushes in 10 cc syringes, a sterile occlusive dressing, and a bio-patch if available.
- Nonsterile products:
- Bouffant or surgeon cap
- Mask with eye shield
- Sterile products:
- Personal protective equipment: including gloves, gown
- Drape
- Gauze (4x4)
- Chlorhexidine swabs or similar antiseptic agent
- Sterile ultrasound probe cover with sterile ultrasound gel
- Biopatch
- "Luer locks" or catheter caps for each lumen
- Central venous catheter kit, which generally includes:
- Central venous catheter (triple-lumen, dual-lumen, or large bore single-lumen)
- 18 gauge introducer needle, with a syringe
- #11 blade Scalpel
- Guidewire
- Vasodilator
- Suture material (generally 3-0 silk suture with a straight needle or a needle driver)
- Saline lock (number depends on the type of device)
- 1% lidocaine, small gauge needle (25 or 27 gauge), syringe
- Ultrasound machine with a high-frequency linear transducer
Personnel
CVC insertion should be performed by a proceduralist skilled in the technique. The procedure can either be performed with or without a nurse to assist.
Preparation
It is essential first to obtain consent for the procedure, if possible. Discuss the risks, benefits, and potential complications of the procedure. Once consent is obtained, inform nursing that the patient will be undergoing central venous catheter insertion. Gather the above equipment and necessary personnel, and clear the room of any visitors or non-essential staff to maintain maximum sterility. Use the ultrasound machine to assess the preferable access site (internal jugular, subclavian, or common femoral veins), taking note of anatomical variations, adjacent structures, and the ease with which the procedure can be performed at that site. Place the patient in an anatomically advantageous position for the procedure.
With all access options, the proceduralist should adjust the height of the bed, and clear away clothing, jewelry, and any non-essential equipment which may impede the preparation of a clear sterile field. The patient should be placed on a cardiac monitor that can cycle vital signs every 5 minutes and maintain telemetry. For placement of a central line utilizing either the internal jugular vein or and subclavian vein access, the patient should be placed in the Trendelenburg position to increase the size of the vessel and improve the chance of first-pass success. For femoral vein access, the patient should be in a supine position.
Once a cursory anatomy scan is performed with ultrasound, the patient’s access site should be cleaned to remove all ultrasound jelly. After completing appropriate hand hygiene and donning non-sterile personal protective equipment, open all sterile equipment, creating a “sterile field.” This can be accomplished by grasping the corners of the pure wraps and opening them out and away from the proceduralist. Once a sterile field has been created, clean the site with your chosen antisept; this is typically performed using chlorhexidine, or in the event of a trauma, betadine. Prepare the vascular probe to be easily sheathed with a sterile probe cover. After that, don the sterile personal protective equipment, and prepare the central venous catheter by attaching saline locks with saline flushes and flushing all of the ports to ensure that there are no equipment issues. Next, remove the saline lock from the most distal port. Place the sterile drape over the patient, with the access point over the procedure site. Sheath the ultrasound probe with the sterile probe cover. The needle driver from the central line kit may clamp the proximal portion of the probe cover to the sterile drape to avoid the probe falling off the sterile field during the procedure. Assure that all equipment is within reach before initiating the procedure. Immediately before the procedure, the proceduralist should perform a “time out” with nursing.
Technique or Treatment
The patient should be positioned in Trendelenburg for IJ or flat for common femoral or subclavian venous access. Depending on the patient's anatomy, a cushion may be placed beneath the vertebral column, facilitating needle insertion and dilation of the SC vein.
After preparation is completed, the following steps should be followed:
- Under ultrasound guidance, identify the vein (check that the vessel is compressible, and if in doubt, check doppler color flow) and use 1% lidocaine to anesthetize the skin and subcutaneous tissue (in awake patients).
- Under ultrasound guidance, use the finder needle with a ten cc syringe attached; at a 45 to 90-degree angle, advance the hand through the skin, holding negative pressure on the syringe until a flash of dark venous blood appears. Be sure to maintain dynamic visualization of the needle tip as it enters the vessel.
- Following the aspiration of venous blood, stabilize the needle with the dominant hand, disconnect the needle from the syringe, and thread the guidewire through the needle. The wire should advance quickly. If there is any resistance, you may not be in the vessel; there may be an obstruction distal to the entry site, or the j-tip of the wire may be advancing retrograde. Attempt to remove the wire and re-thread. If the wire enters the right atrium, ectopy can be appreciated. Should telemetry demonstrate any ectopy or arrhythmia, the wire should be immediately pulled back until the arrhythmia resolves. Typically the wire does not need to be pulled out completely.
- Once the wire is at 15 cm (three hash marks), stabilize the wire between two or more fingertips and withdraw the needle making sure not to sustain a needlestick inadvertently. Never let go of the wire!
- Once the needle has been removed, re-image the vessel with ultrasound in both a transverse and longitudinal plane. The wire should be visualized within the vessel lumen. If you do not see the wire within the lumen, do not proceed to the next step. If you are uncertain that the wire is in the vessel's lumen, remove the wire, hold pressure on the site, and either re-attempt obtaining access to the boat with the finder needle or switch to a different anatomic site.
- In addition to the dynamic visualization of the procedure with ultrasound, some practitioners use manometry to ensure that the catheter is in the venous system and not the arterial system. To do this, an angiocatheter is threaded over the wire, the wire is removed, and the included extension set for the central venous catheter is attached and held upright in the air. The meniscus formed by the column of blood that slowly fills the extension tubing should plateau if the angiocath is in the venous system. However, this method is time-consuming and unreliable in shock states. Regardless, it can be helpful with the subclavian approach, which is often difficult to fully accomplish with dynamic ultrasound visualization.
- Once the wire is verified to be within the vessel lumen, "preload" the dilator onto the guidewire and thread it toward the junction of the skin and wire. Leave approximately 2 or 3 cm between the dilator and the skin edge. Use the scalpel to create a small nick in the skin by sliding the blunt end of the scalpel blade along the wire to make a skin incision approximately 0.5 cm in width and half the depth of the scalpel blade. Remove the scalpel, and thread the dilator into the incision. Pre-loading the dilator minimizes blood loss and improves the ease of insertion.
- Grasping the dilator in the middle portion, apply gentle, steady pressure, sometimes with a slight twisting motion, to dilate the soft tissue and enable passage of the central venous catheter. Approximately 1/3 to 1/2 of the length of the dilator will need to be inserted into the skin/soft tissue space. This depends upon the anatomic site and the specific type of central venous catheter. Dialysis catheters will require several stages of dilation with increasingly larger dilators and potentially multiple uses of a scalpel to widen the incision.
- Remove the dilator, and place sterile gauze over the site to maintain sterility and minimize bleeding. Again, at no point should the proceduralist lose control of the guidewire.
- Thread the central venous catheter over the guidewire. Slide the guidewire slightly out of the skin to help control the guidewire while advancing the catheter.
- Holding the distal aspect of the central venous catheter, slowly insert the central venous catheter through the vessel lumen until the proximal hub is adjacent to the insertion site. Throughout this process, always ensure one hand is holding the guidewire. Sliding the guidewire slightly out of the skin can help control the guidewire when advancing the catheter. Once the catheter is fully inserted, the guidewire can be gently pulled through the distal port (usually brown)
- Using a syringe, aspirate blood, remove air from each port, and flush with sterile saline solution. "Luer locks" may be attached to the end of each port either before or after this step.
- The central venous catheter should be sutured with two sutures, a bio-patch should be placed between the catheter hub and the skin, and a sterile occlusive dressing should be placed over the catheter/skin entry site. Clean drapes and soiled non-sharp products should be disposed of in biohazard bins. All sharps should be placed in sharps bins. The patient should be put back into a position of comfort, and the proceduralist should verify that the line is appropriately set within a central vein.
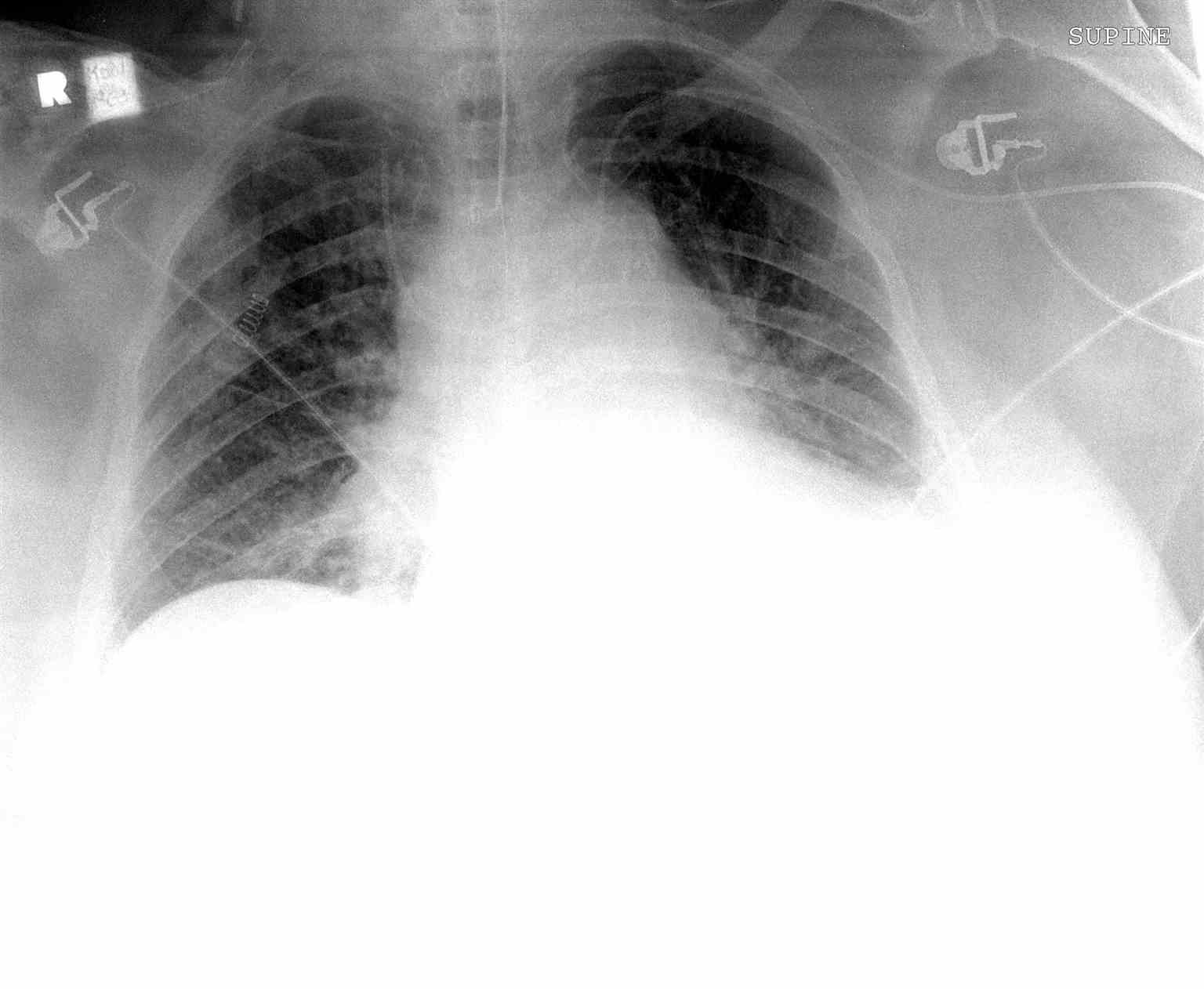
- In addition to dynamic ultrasound guidance, three methods ensure that a central venous catheter is placed correctly. A venous blood gas can be obtained from the distal port of the central line, a chest x-ray can be performed, and central venous pressure can be obtained from the distal port. The blood gas and central venous pressure (CVP) are optional. Still, a chest x-ray should be performed in all IJ and SC CVC insertions to confirm placement and verify that no complications (such as iatrogenic pneumothorax) have occurred. The x-ray should demonstrate the distal tip of the central venous line within either the superior vena cava (SC/IJ) or inferior vena cava (femoral).
Complications
Numerous potential complications can occur during the procedural placement of a central venous catheter but also due to the indwelling equipment.
Procedural complications include the following:
- Arrhythmias – typically ventricular or bundle branch blocks due to guidewire irritation of the atria or ventricles
- Arterial puncture
- Pulmonary puncture with or without resultant pneumothorax
- Bleeding – hematoma formation, which can obstruct the airway
- Tracheal injury
- Air emboli during venous puncture or removal of the catheter[32]
Post-procedural complications include the following:
Clinical Significance
When performed correctly, the insertion of a central venous catheter is safe, productive, and potentially life-saving. However, particular clinical pearls should be at the forefront of the proceduralist’s mind when performing this procedure.
- Whenever possible, take the time to prepare for the procedure thoroughly, and ensure that all necessary personnel and equipment are in the room and readily available. Lack of preparation will compound any potential complications that may be encountered.
- Ensure that sterile products are not contaminated and that there is no evidence of damage to the packaging. Follow sterile procedures at all times. Central line infections can be severe and life-threatening illnesses.
- When using the IJ or SC site for access, obtain a stat portable chest x-ray immediately after line placement to ensure no pneumothorax and that the line terminates in the superior vena cava.
- Suppose one has a failed attempt at the IJ site and needs to seek access at another location. In that case, the ipsilateral subclavian is preferred, given the risk of bilateral pneumothoraces with an attempt at the contralateral internal jugular vein. One may anticipate this possibility by cleaning and prepping the IJ and SC site on the procedure side.
- If unsure of the placement of a guidewire within the vein and limited views on ultrasound, manometry is a valuable tool to establish that the guidewire is within the venous system. However, this may be falsely reassuring in shock states where arterial pressure is low.
- Subclavian access does appear to have fewer infections but potentially higher procedural complications, mainly if performed by a clinician with limited experience.[35]
- The internal jugular, subclavian, and femoral veins have higher success rates and fewer complications when access is performed with ultrasound.
- The clinician must maintain hold of the guidewire at all times while it is inside the patient. The wire can be lost inside the patient and may migrate into the right ventricle or inferior vena cava, leading to additional invasive procedures to recover the wire.
- Always ensure that the catheter is appropriately placed through one or several methods: radiographic evidence, measurement of CVP, or analyzing venous blood gas.[36]
- Never use excessive force during any part of this procedure. It will lead to damage to local structures.
Enhancing Healthcare Team Outcomes
After a CVC placement, nurses are charged with maintaining, monitoring, and utilizing central venous catheters. The bedside nurse must be adept at recognizing complications such as infections, hematoma, thrombosis of the catheter, and signs of pneumothorax and bleeding. Nurses are also responsible for ensuring that the site is maintained in a clean and sterile fashion. Beyond the immediate complications of the procedure itself, nursing must be immediately aware of any ongoing issues and delayed complications. Their role in the interprofessional team is of monumental importance in maintaining the central venous catheter and recognizing potential complications.
Clear communication between all team members is essential to appropriate patient care.[37] The clinician should inform the nurse as soon as the proper placement of the CVC is confirmed, and nursing should wait for this confirmation before using the line to administer medications. The nurse and the clinician should be aware of and track when the line was placed. CVCs are temporary, and complication rates increase when lines are left in too long.
Nursing, Allied Health, and Interprofessional Team Interventions
Daily inspection of the access site and device patency should be performed during nursing rounds. In particular, nursing must disinfect injection ports, catheter hubs, and needleless connectors with institutionally approved antiseptics. Intravenous administration sets should be changed regularly per hospital policy. The site should be checked for bleeding, hematoma formation, and cellulitis signs, including erythema, purulent drainage, and warmth.[38]
Dressings should be changed if visibly soiled. This must be performed with proper sterile technique. Importantly, any manipulation of the catheter site should be done using a sterile procedure. A bouffant cap, mask, and sterile gloves must be worn to minimize infection. The area should be cleaned with approved antiseptics, allowed to dry, and a sterile occlusive dressing must be replaced.[38]
At interprofessional team rounds, there should be a daily discussion about whether or not the central venous catheter is still indicated. If deemed unnecessary for further management, the central venous catheter should be removed expeditiously.[39]
Nursing, Allied Health, and Interprofessional Team Monitoring
Many potential complications can arise from the placement of central venous catheters. Nursing staff should be aware of the immediate and delayed complications and alert the clinician in charge of the patient’s care.[39] However, clinicians should also be wary of complications and always consider the catheter (as a source) if the patient shows signs of infection.
Media
(Click Image to Enlarge)
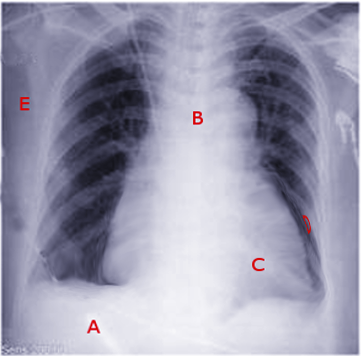
(Click Image to Enlarge)
(Click Image to Enlarge)
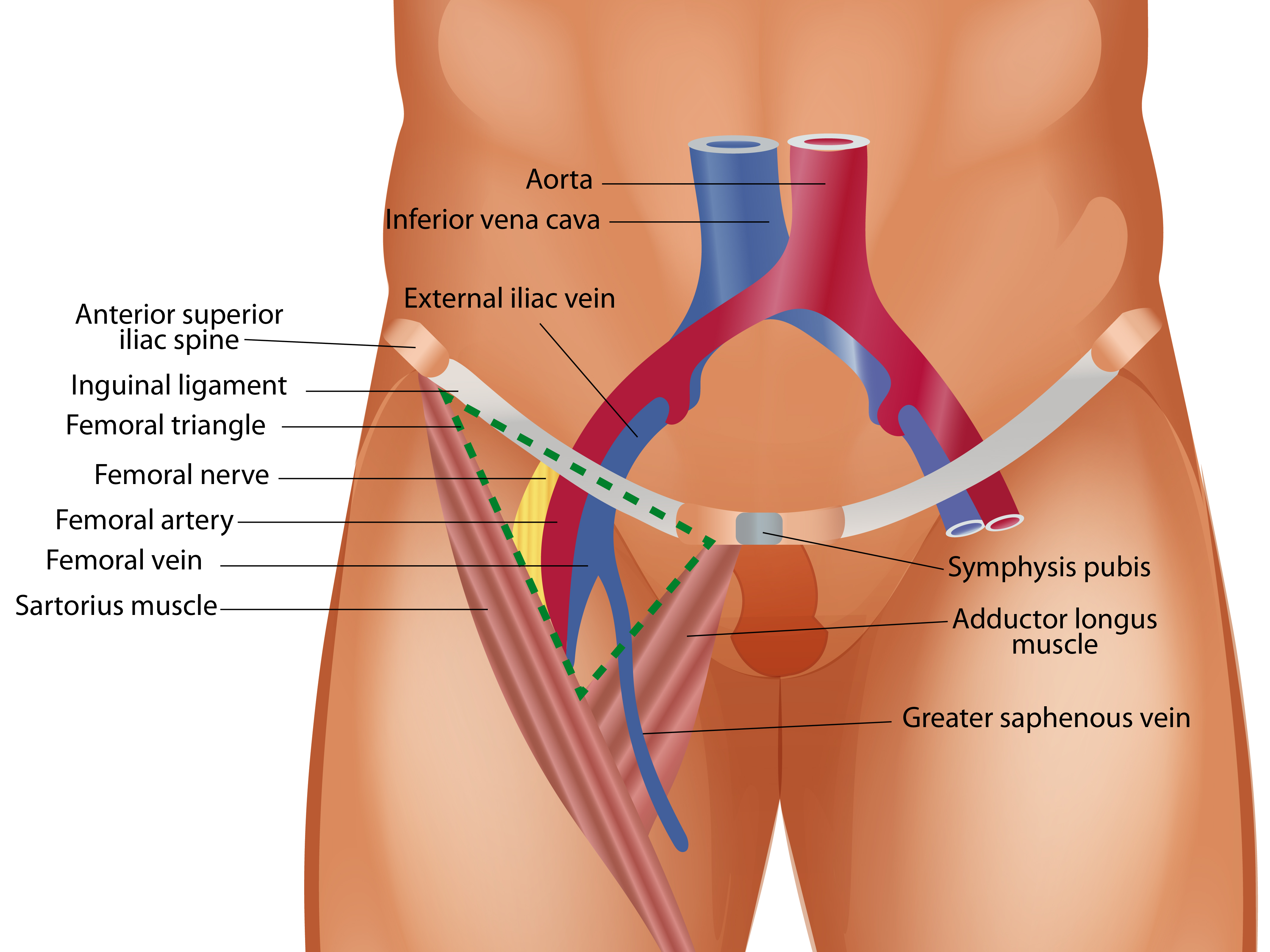
Femoral Triangle. This figure illustrates the femoral triangle, which is bounded superiorly by the inguinal ligament, laterally by the medial border of the sartorius muscle, and medially by the lateral border of the adductor longus muscle. Clinically, this area is used for femoral vein access for central venous catheterization. From medial to lateral, the structures are in the following order VAN: femoral vein, femoral artery, and femoral nerve.
Contributed by Amina Tariq, MD
References
Beheshti MV. A concise history of central venous access. Techniques in vascular and interventional radiology. 2011 Dec:14(4):184-5. doi: 10.1053/j.tvir.2011.05.002. Epub [PubMed PMID: 22099008]
BOLT W, KNIPPING HW. [Congratulations to Werner Forssmann on winning the 1956 Nobel prize for medicine]. Medizinische Klinik. 1956 Dec 7:51(49):2073-6 [PubMed PMID: 13386873]
Konner K. History of vascular access for haemodialysis. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2005 Dec:20(12):2629-35 [PubMed PMID: 16204277]
Ipe TS, Marques MB. Vascular access for therapeutic plasma exchange. Transfusion. 2018 Feb:58 Suppl 1():580-589. doi: 10.1111/trf.14479. Epub [PubMed PMID: 29443413]
American Society of Anesthesiologists Task Force on Central Venous Access, Rupp SM, Apfelbaum JL, Blitt C, Caplan RA, Connis RT, Domino KB, Fleisher LA, Grant S, Mark JB, Morray JP, Nickinovich DG, Tung A. Practice guidelines for central venous access: a report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2012 Mar:116(3):539-73. doi: 10.1097/ALN.0b013e31823c9569. Epub [PubMed PMID: 22307320]
Level 1 (high-level) evidenceSuess EM, Pinsky MR. Hemodynamic Monitoring for the Evaluation and Treatment of Shock: What Is the Current State of the Art? Seminars in respiratory and critical care medicine. 2015 Dec:36(6):890-8. doi: 10.1055/s-0035-1564874. Epub 2015 Nov 23 [PubMed PMID: 26595049]
Lau EW. Upper body venous access for transvenous lead placement--review of existent techniques. Pacing and clinical electrophysiology : PACE. 2007 Jul:30(7):901-9 [PubMed PMID: 17584273]
Seldinger SI. Catheter replacement of the needle in percutaneous arteriography. A new technique. Acta radiologica. Supplement. 2008 Aug:434():47-52. doi: 10.1080/02841850802133386. Epub [PubMed PMID: 19023715]
Saugel B, Scheeren TWL, Teboul JL. Ultrasound-guided central venous catheter placement: a structured review and recommendations for clinical practice. Critical care (London, England). 2017 Aug 28:21(1):225. doi: 10.1186/s13054-017-1814-y. Epub 2017 Aug 28 [PubMed PMID: 28844205]
Lamperti M, Bodenham AR, Pittiruti M, Blaivas M, Augoustides JG, Elbarbary M, Pirotte T, Karakitsos D, Ledonne J, Doniger S, Scoppettuolo G, Feller-Kopman D, Schummer W, Biffi R, Desruennes E, Melniker LA, Verghese ST. International evidence-based recommendations on ultrasound-guided vascular access. Intensive care medicine. 2012 Jul:38(7):1105-17. doi: 10.1007/s00134-012-2597-x. Epub 2012 May 22 [PubMed PMID: 22614241]
Dietrich CF, Horn R, Morf S, Chiorean L, Dong Y, Cui XW, Atkinson NS, Jenssen C. Ultrasound-guided central vascular interventions, comments on the European Federation of Societies for Ultrasound in Medicine and Biology guidelines on interventional ultrasound. Journal of thoracic disease. 2016 Sep:8(9):E851-E868 [PubMed PMID: 27747022]
Level 3 (low-level) evidenceTroianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, Reeves ST, Councils on Intraoperative Echocardiography and Vascular Ultrasound of the American Society of Echocardiography, Society of Cardiovascular Anesthesiologists. Special articles: guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society Of Cardiovascular Anesthesiologists. Anesthesia and analgesia. 2012 Jan:114(1):46-72. doi: 10.1213/ANE.0b013e3182407cd8. Epub 2011 Nov 29 [PubMed PMID: 22127816]
Bodenham Chair A, Babu S, Bennett J, Binks R, Fee P, Fox B, Johnston AJ, Klein AA, Langton JA, Mclure H, Tighe SQ. Association of Anaesthetists of Great Britain and Ireland: Safe vascular access 2016. Anaesthesia. 2016 May:71(5):573-85. doi: 10.1111/anae.13360. Epub 2016 Feb 17 [PubMed PMID: 26888253]
Ishizuka M, Nagata H, Takagi K, Kubota K. Right internal jugular vein is recommended for central venous catheterization. Journal of investigative surgery : the official journal of the Academy of Surgical Research. 2010 Apr:23(2):110-4. doi: 10.3109/08941930903469342. Epub [PubMed PMID: 20497014]
Level 2 (mid-level) evidenceHessel EA 2nd. Landmark-guided internal jugular vein cannulation: is there still a role and, if so, what should we do about it? Journal of cardiothoracic and vascular anesthesia. 2012 Dec:26(6):979-81. doi: 10.1053/j.jvca.2012.08.002. Epub 2012 Sep 18 [PubMed PMID: 22995456]
Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. The Cochrane database of systematic reviews. 2015 Jan 9:1(1):CD011447. doi: 10.1002/14651858.CD011447. Epub 2015 Jan 9 [PubMed PMID: 25575245]
Level 1 (high-level) evidenceParienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, Marqué S, Thuong M, Pottier V, Ramakers M, Savary B, Seguin A, Valette X, Terzi N, Sauneuf B, Cattoir V, Mermel LA, du Cheyron D, 3SITES Study Group. Intravascular Complications of Central Venous Catheterization by Insertion Site. The New England journal of medicine. 2015 Sep 24:373(13):1220-9. doi: 10.1056/NEJMoa1500964. Epub [PubMed PMID: 26398070]
Woodhouse P, Waheed A, Bordoni B. Anatomy, Thorax, Brachiocephalic (Innominate) Veins. StatPearls. 2025 Jan:(): [PubMed PMID: 31335059]
Rezayat T, Stowell JR, Kendall JL, Turner E, Fox JC, Barjaktarevic I. Ultrasound-Guided Cannulation: Time to Bring Subclavian Central Lines Back. The western journal of emergency medicine. 2016 Mar:17(2):216-21. doi: 10.5811/westjem.2016.1.29462. Epub 2016 Mar 2 [PubMed PMID: 26973755]
Fragou M, Gravvanis A, Dimitriou V, Papalois A, Kouraklis G, Karabinis A, Saranteas T, Poularas J, Papanikolaou J, Davlouros P, Labropoulos N, Karakitsos D. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Critical care medicine. 2011 Jul:39(7):1607-12. doi: 10.1097/CCM.0b013e318218a1ae. Epub [PubMed PMID: 21494105]
Level 1 (high-level) evidenceLalu MM, Fayad A, Ahmed O, Bryson GL, Fergusson DA, Barron CC, Sullivan P, Thompson C, Canadian Perioperative Anesthesia Clinical Trials Group. Ultrasound-Guided Subclavian Vein Catheterization: A Systematic Review and Meta-Analysis. Critical care medicine. 2015 Jul:43(7):1498-507. doi: 10.1097/CCM.0000000000000973. Epub [PubMed PMID: 25803646]
Level 1 (high-level) evidencePatrick SP, Tijunelis MA, Johnson S, Herbert ME. Supraclavicular subclavian vein catheterization: the forgotten central line. The western journal of emergency medicine. 2009 May:10(2):110-4 [PubMed PMID: 19561831]
Muhm M, Sunder-Plassmann G, Apsner R, Kritzinger M, Hiesmayr M, Druml W. Supraclavicular approach to the subclavian/innominate vein for large-bore central venous catheters. American journal of kidney diseases : the official journal of the National Kidney Foundation. 1997 Dec:30(6):802-8 [PubMed PMID: 9398124]
Lu WH, Yao ML, Hsieh KS, Chiu PC, Chen YY, Lin CC, Huang TC, Chen CC. Supraclavicular versus infraclavicular subclavian vein catheterization in infants. Journal of the Chinese Medical Association : JCMA. 2006 Apr:69(4):153-6 [PubMed PMID: 16689195]
Nasr-Esfahani M, Kolahdouzan M, Mousavi SA. Inserting central venous catheter in emergency conditions in coagulopathic patients in comparison to noncoagulopathic patients. Journal of research in medical sciences : the official journal of Isfahan University of Medical Sciences. 2016:21():120. doi: 10.4103/1735-1995.193511. Epub 2016 Nov 7 [PubMed PMID: 28255328]
Desmond J, Teece S. Best evidence topic report. Thrombotic complications of a femoral central venous catheter. Emergency medicine journal : EMJ. 2004 Nov:21(6):714-5 [PubMed PMID: 15496705]
Marik PE, Flemmer M, Harrison W. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: a systematic review of the literature and meta-analysis. Critical care medicine. 2012 Aug:40(8):2479-85. doi: 10.1097/CCM.0b013e318255d9bc. Epub [PubMed PMID: 22809915]
Level 1 (high-level) evidenceArvaniti K, Lathyris D, Blot S, Apostolidou-Kiouti F, Koulenti D, Haidich AB. Cumulative Evidence of Randomized Controlled and Observational Studies on Catheter-Related Infection Risk of Central Venous Catheter Insertion Site in ICU Patients: A Pairwise and Network Meta-Analysis. Critical care medicine. 2017 Apr:45(4):e437-e448. doi: 10.1097/CCM.0000000000002092. Epub [PubMed PMID: 27632678]
Level 1 (high-level) evidenceClar DT, Arbor TC, Bordoni B. Anatomy, Abdomen and Pelvis: Femoral Region. StatPearls. 2025 Jan:(): [PubMed PMID: 30860736]
Hall DP, Lone NI, Watson DM, Stanworth SJ, Walsh TS, Intensive Care Study of Coagulopathy (ISOC) Investigators. Factors associated with prophylactic plasma transfusion before vascular catheterization in non-bleeding critically ill adults with prolonged prothrombin time: a case-control study. British journal of anaesthesia. 2012 Dec:109(6):919-27. doi: 10.1093/bja/aes337. Epub 2012 Sep 30 [PubMed PMID: 23025970]
Level 2 (mid-level) evidenceKaufman RM, Djulbegovic B, Gernsheimer T, Kleinman S, Tinmouth AT, Capocelli KE, Cipolle MD, Cohn CS, Fung MK, Grossman BJ, Mintz PD, O'Malley BA, Sesok-Pizzini DA, Shander A, Stack GE, Webert KE, Weinstein R, Welch BG, Whitman GJ, Wong EC, Tobian AA, AABB. Platelet transfusion: a clinical practice guideline from the AABB. Annals of internal medicine. 2015 Feb 3:162(3):205-13. doi: 10.7326/M14-1589. Epub [PubMed PMID: 25383671]
Kornbau C, Lee KC, Hughes GD, Firstenberg MS. Central line complications. International journal of critical illness and injury science. 2015 Jul-Sep:5(3):170-8. doi: 10.4103/2229-5151.164940. Epub [PubMed PMID: 26557487]
Garcia X, Pye S, Tang X, Gossett J, Prodhan P, Bhutta A. Catheter-Associated Blood Stream Infections in Intracardiac Lines. Journal of pediatric intensive care. 2017 Sep:6(3):159-164. doi: 10.1055/s-0036-1596064. Epub 2016 Dec 5 [PubMed PMID: 31073442]
van de Weerdt EK, Biemond BJ, Baake B, Vermin B, Binnekade JM, van Lienden KP, Vlaar APJ. Central venous catheter placement in coagulopathic patients: risk factors and incidence of bleeding complications. Transfusion. 2017 Oct:57(10):2512-2525. doi: 10.1111/trf.14248. Epub 2017 Aug 30 [PubMed PMID: 28856685]
Akaraborworn O. A review in emergency central venous catheterization. Chinese journal of traumatology = Zhonghua chuang shang za zhi. 2017 Jun:20(3):137-140. doi: 10.1016/j.cjtee.2017.03.003. Epub 2017 May 17 [PubMed PMID: 28552330]
Abood GJ, Davis KA, Esposito TJ, Luchette FA, Gamelli RL. Comparison of routine chest radiograph versus clinician judgment to determine adequate central line placement in critically ill patients. The Journal of trauma. 2007 Jul:63(1):50-6 [PubMed PMID: 17622868]
Velasquez Reyes DC, Bloomer M, Morphet J. Prevention of central venous line associated bloodstream infections in adult intensive care units: A systematic review. Intensive & critical care nursing. 2017 Dec:43():12-22. doi: 10.1016/j.iccn.2017.05.006. Epub 2017 Jun 26 [PubMed PMID: 28663107]
Level 1 (high-level) evidencePerin DC, Erdmann AL, Higashi GD, Sasso GT. Evidence-based measures to prevent central line-associated bloodstream infections: a systematic review. Revista latino-americana de enfermagem. 2016 Sep 1:24():e2787. doi: 10.1590/1518-8345.1233.2787. Epub 2016 Sep 1 [PubMed PMID: 27598378]
Level 1 (high-level) evidenceSchiffer CA, Mangu PB, Wade JC, Camp-Sorrell D, Cope DG, El-Rayes BF, Gorman M, Ligibel J, Mansfield P, Levine M. Central venous catheter care for the patient with cancer: American Society of Clinical Oncology clinical practice guideline. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2013 Apr 1:31(10):1357-70. doi: 10.1200/JCO.2012.45.5733. Epub 2013 Mar 4 [PubMed PMID: 23460705]
Level 1 (high-level) evidence