Local and Regional Anesthesia in Ophthalmology and Ocular Trauma
Local and Regional Anesthesia in Ophthalmology and Ocular Trauma
Introduction
Appropriate selection of local and regional anesthesia in ophthalmic surgery depends on the planned procedure, necessary duration, and patient characteristics. There is considerable redundancy of sensory innervation to the face, and therefore a combination of anesthetic techniques is often needed to achieve optimal results. This chapter will briefly review types of ocular anesthesia with a focus on periocular anatomy and targeted anesthesia.
Topical Ocular Anesthesia
Topical anesthesia is a relatively fast and simple technique that provides superficial anesthesia without the potential hazards of injections. Its use is limited to low complexity cases with adequate patient cooperation, as it does not provide complete akinesia or intraocular pressure control.[1] Topical anesthesia may be achieved using eye drop applications (e.g., proparacaine hydrochloride 0.5%, tetracaine hydrochloride 0.5%), gel application (e.g., lidocaine hydrochloride 3.5% gel), or anesthetic-impregnated sponge application.[2][3][4]
Subconjunctival Anesthesia
Subconjunctival injection of local anesthesia involves direct infiltration of anesthetic under the conjunctiva. This local infiltration technique may be used in a variety of procedures, including intravitreal injections, cataracts, glaucoma, and pterygium surgery.[5][6] Following a drop of topical anesthetic, a small gauge needle (27 to 30G) is used to administer local anesthesia 5-8 mm from the limbus at either a superotemporal or inferotemporal site.[7] The needle is placed in a bevel-down position to reduce the risk of inadvertent penetration of the globe. A cotton-tipped applicator may be utilized to spread the anesthetic. The injection results in reliable concentrations of local anesthetic and improves patient comfort for ocular procedures.
Sub-Tenon Anesthesia
Sub-Tenon anesthesia involves the injection of local anesthetic into the potential space between the Tenon capsule and the sclera. The inferonasal conjunctival fornix is the site most commonly utilized for injection to avoid encountering the insertion of the medial rectus or inferior oblique muscles.[5] Anterior or posterior injection techniques may be used to accomplish sub-Tenon anesthesia. Anterior injections are performed superficially just beyond the equator using low volumes (3 to 5 ml) of anesthetic. In contrast, posterior injections provide more anesthetic into the posterior intra- and extraconal spaces; this allows for smaller volumes of anesthetic with a lower risk of chemosis.[1][8]
Intracameral Anesthesia
During intraocular procedures, intracameral injection of local anesthesia involves the administration of a small volume of anesthesia (0.1-0.5 mL) into the anterior chamber. Common intracameral agents include preservative-free lidocaine hydrochloride 1% and bupivacaine hydrochloride 0.5%. These agents must be free of preservatives, such as benzalkonium chloride or other agents, which may cause toxic anterior segment syndrome. Likewise, bisulfites may carry similar issues with corneal endothelial toxicity, although diluted forms of less than 0.025% appear safe.[9] However, not all medications are available in preservative and bisulfite-free form, and the surgeon must be aware of specific ingredients utilized in each product. Intracameral anesthesia is frequently combined with topical anesthetic agents and subconjunctival or sub-Tenon anesthetics as an effective and safe method to achieve analgesia in cataract surgery.[1][4][10]
Local and Regional Anesthesia
Targeted anesthesia can be administered through direct local infiltration or a regional nerve blockade. Local tissue infiltration is technically straightforward and sufficient for the exploration and repair of small soft tissue injuries. In cases of larger complex injuries, a nerve block is a useful tool to provide anesthesia to a larger area with a smaller amount of anesthetic while minimizing tissue distortion.[11]
The disadvantages of regional nerve block include pain with injection, the need for patient cooperation, and the risks associated with the injection technique and medication. Injection of any substance carries a risk of an allergic reaction, overdose, medication-specific side effects, bleeding, infection, and tissue damage. The more proximal the local anesthesia is injected to the nerve root and other important anatomical structures, the higher the risk of significant adverse reaction.[12][13]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Periocular Sensory Innervation
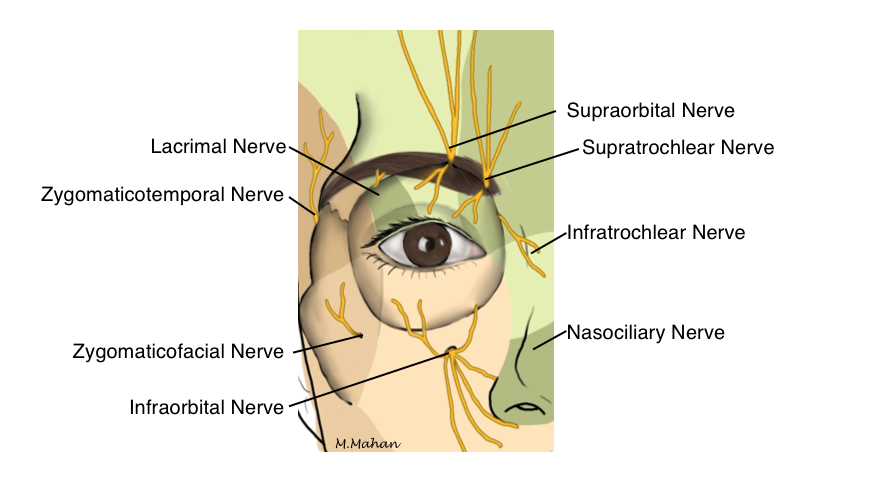
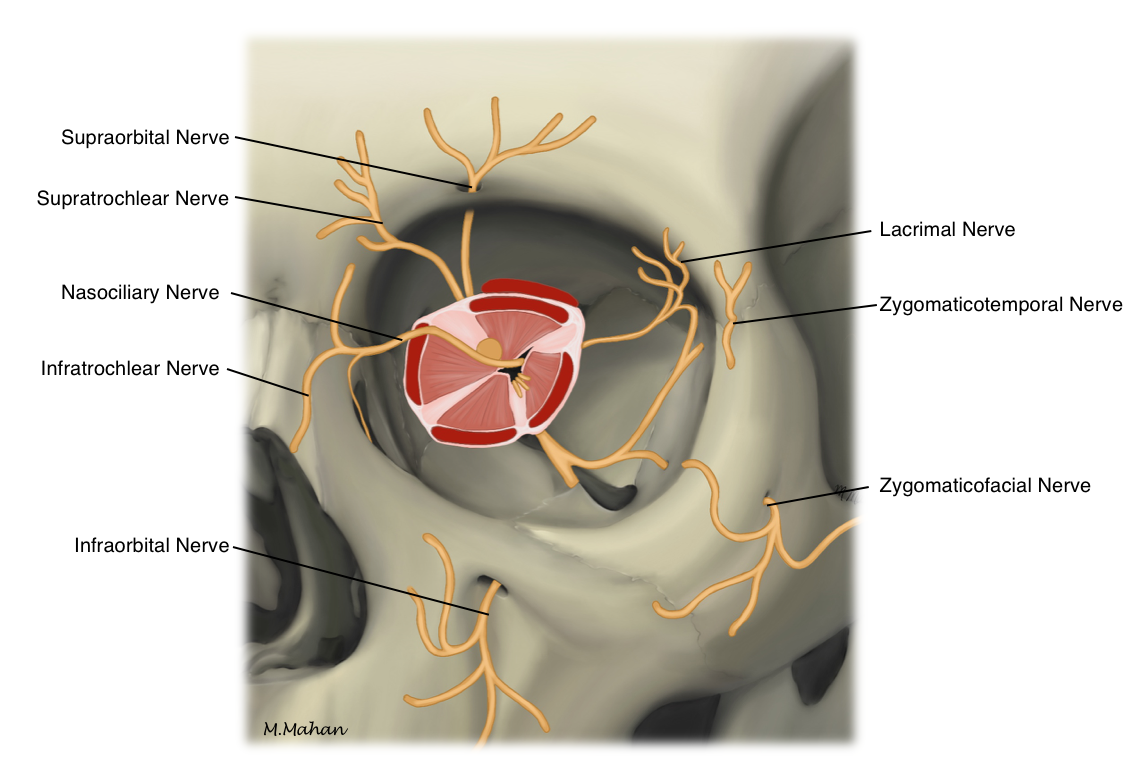
The first and second divisions of the trigeminal nerve provide sensory innervation to the brow and midface (figure 1). The ophthalmic division (V1) runs along the lateral wall of the cavernous sinus and enters the orbit through the superior orbital fissure. Within the orbit, the nerve divides into the supraorbital and supratrochlear nerves.
The maxillary division (V2) travels along the inferolateral wall of the cavernous sinus and exits through the foramen rotundum. The zygomatic nerve branches off within the pterygopalatine fossa and enters the orbit in the inferior orbital fissure before dividing into the zygomaticofacial and zygomaticotemporal nerves. After entering the orbit through the inferior orbital fissure, V2 becomes the infraorbital nerve (figure 2). Within the infraorbital canal, the anterior superior alveolar nerve branches off before the infraorbital nerve exits. Terminal nasal, labial, and palpebral branches provide sensation to the skin of the nose, eyelids, and face.
Indications
A wide variety of indications exist for local and regional anesthesia in ophthalmic surgery. Anatomical location and procedure length are important to consider when deciding the most appropriate anesthetic course. Specific indications for each technique are outside the scope of this chapter. General indications include but are not limited to:
- Intraocular surgery
- Periocular surgery
- Oculoplastic, lacrimal, and sinus surgery
- Facial reconstruction
- Migraine
- Primary and secondary neuralgia
- Dermatologic procedures
Contraindications
Absolute
- Patient refusal
- Allergy to anesthetic
Relative
- Open globe
- Local infection
- Distorted anatomy (traumatic, post-surgical, or due to underlying disease)
- Bleeding or clotting disorders
- Poor patient cooperation
Equipment
Retrobulbar Block
- Povidone-iodine 5% ophthalmic preparation
- Topical anesthetic drops (e.g. proparacaine hydrochloride 0.5%, tetracaine hydrochloride 0.5%)
- Anesthetic agent (generally without epinephrine in seeing eyes, as it may cause vasoconstriction with resultant central retinal artery occlusion and irreversible loss of vision)
- Sterile gauze
- Syringe: 5 to 10 mL
- Needle: 23 to 25 gauge, 30 to 38 mm in length
Periocular Nerve Blocks
- Povidone-iodine 10% preparation
- Anesthetic agent
- Sterile gauze
- Syringe: 5 to 10 mL
- Needle: 25 to 30 gauge
Anesthetic Agents
The choice of local anesthetic agent is based on its pharmacologic properties and availability. The surgeon or anesthesiologist may choose to use a single agent alone or a combination of agents. The injected anesthetic agents most often used include lidocaine, mepivacaine, bupivacaine, and ropivacaine. Lidocaine and mepivacaine have a quick onset of effect, typically within 2 to 3 minutes after infiltration. Bupivacaine onset can take more than 10 minutes, and given its longer duration, can have more postoperative residual effects. Systemic toxicity is rare given the typically low volumes of medication (Table 1).[14] Agents such as lidocaine, bupivacaine, or tetracaine may come in eyedrop or gel formulations to allow for topical use.[15][16]
Table 1. Anesthetic agents and maximum recommended doses[14]
| Anesthetic Agent | Maximum Anesthetic per Dose |
| Lidocaine |
4.5 mg/kg (not to exceed 300 mg total) |
| Lidocaine + Epinephrine |
7 mg/kg (not to exceed 500 mg total) |
| Bupivacaine |
2.5 mg/kg (not to exceed 175 mg per dose, with a maximum 24-hour dose of 400 mg) |
| Bupivacaine + Epinephrine |
3 mg/kg (not to exceed 225 mg per dose, with a maximum 24-hour dose of 400 mg) |
Adjunctive Medications
Some adjuncts have been used in conjunction with local anesthetics for improved effects and outcomes. Hyaluronidase is an enzyme widely used to enhance the spread of local anesthetic through the connective tissue. This, in turn, optimizes the rate of onset and surface area with preserved tissue contour; however, it may reduce the duration of the anesthetic effect.[17] Clonidine is an alpha2-adrenergic agonist used as a topical agent to reduce intraocular pressure, typically used in glaucoma cases, and provides enhanced intraoperative and postoperative analgesia when used in conjunction with an injected local anesthetic. Adverse effects of hypotension or excessive sedation are rarely encountered at the low utilized dose of 1mcg/kg. Dexmedetomidine is another alpha2-adrenergic agonist that may be used.[18] Using sodium bicarbonate for alkalinization of local anesthetics has been used to decrease the discomfort associated with the initial injection of the anesthetic and accelerate the onset of effect. Other adjuncts include epinephrine, muscle relaxants, opioids, and warming the local anesthetics. Many adjunctive agents have fallen out of favor due to associated risks.[19]
Personnel
Administration of ocular and periocular anesthesia requires advanced knowledge of orbital anatomy to prevent vision-threatening complications. These techniques must be performed by trained providers, including anesthesiologists and ophthalmologists. Additional sedation is often necessary to improve patient comfort, and trained assistants can help facilitate safe and effective anesthetic delivery.
Preparation
Informed consent, including discussing risks, benefits, and alternatives, is an essential step prior to any procedure. Anatomical landmarks should be evaluated before starting the procedure, with special attention to potential challenges and complications. Required equipment should be collected and organized, and the location of the procedure should be confirmed and marked.
Technique or Treatment
Targeted Nerve Blocks
Retrobulbar Block
A retrobulbar blockade provides anesthesia and akinesia through the infiltration of the intraconal space. The technique is frequently performed prior to intraocular surgery and is favored by many surgeons for its quick onset and longer duration. Knowledge of the orbital anatomy and meticulous technique is important to avoid potential vision- and life-threatening complications, including retrobulbar hemorrhage, damage to the globe, optic nerve, extraocular muscles, and central spread with brain stem depression.[20]
For this reason, extra caution is advised in patients with orbital pathology, high axial myopia, or coagulopathies. Mixtures containing epinephrine are generally avoided due to the risk of vasospasm and retinal ischemia. To start, the inferior lid is prepared with an alcohol swab or povidone-iodine. The inferior orbital rim is then palpated, and the globe is displaced superiorly to expand the space between the orbital floor and globe. With the needle bevel-up (to reduce the risk of globe perforation), the needle is inserted into the skin at or just superior to the level of the inferior orbital rim. The needle is advanced along the orbital floor until the first “pop” is felt, signifying passage through the orbital septum. The needle is then redirected approximately 45 degrees medially and superiorly and advanced through the second “pop,” signifying passage through the muscular cone and entry into the intraconal space.
It is important to draw back the syringe to ensure the needle is not in a vessel. Approximately 3 to 5 ml of anesthetic is injected into this space, paying attention to the expected anterior displacement of the globe, signifying injection of anesthetic into the intraconal space, and palpation of the globe to assess for posterior pressure. The needle is then withdrawn, and pressure is applied to the globe using gauze for 60 to 120 seconds to tamponade potential retrobulbar hemorrhage.
Supraorbital Block
The supraorbital nerve arises from the ophthalmic branch of the trigeminal nerve (V1). The nerve courses through either a supraorbital notch (73.8%) or foramen (26.2%) and divides into a superficial medial branch and a deep lateral branch.[21]
The location of the supraorbital notch or foramen can be approximated by measuring 2 cm from the midline of the face. The notch is often palpable, and marking this site helps ensure proper positioning and targeted blockade. The needle is inserted from an inferolateral position 0.5 cm below the supraorbital notch/foramen and advanced with care taken to avoid penetration of the foramen.[14] Regional supraorbital blockade provides anesthesia to a large area, including the upper eyelid, brow, forehead, and anterior scalp. It has the benefit of anesthetizing a large area with a smaller volume of anesthetic compared to local tissue infiltration.
Supratrochlear Block
The supratrochlear nerve, another branch of V1, exits the supraorbital margin medially to the supraorbital nerve. This location is approximated by identifying the supraorbital margin 3 mm medial to a vertical line from the medial canthus. The block is performed by placing the needle at the site where the supratrochlear nerve emerges at the supraorbital margin and slowly advancing along the course of the nerve.[22] This block is often used in conjunction with the supraorbital block to maximize anesthesia of the forehead.
Nasociliary Block
The nasociliary nerve branches off the ophthalmic nerve within the orbit. The nerve further branches supply the mucosal surface of the sphenoid, ethmoid, frontal sinuses, and the anterior septum, lateral nasal cavity, ala, and apex of the nose. An anesthetic block is optimally aimed toward the anterior and posterior ethmoidal foramina, which additionally delivers the anesthetic to the infratrochlear nerve.[23] Epinephrine is not often used to reduce the risk of retinal artery spasm, and the duration of this block is shortened as a result.
Infratrochlear Block
The infratrochlear nerve, another branch of V1, runs along with the medial rectus muscle within the orbit. It provides sensation to the inferior portion of the medial canthus, lateral nose, medial conjunctiva, and caruncle.[24][25]
The external location of this nerve, which is palpable below the trochlea, enables targeted blockade via infiltration at the superomedial orbit. This block is often used during nasal surgery or skin laceration repairs in this anatomic location.[26]
Anterior Ethmoid Block
The anterior ethmoid nerve supply is composed of internal and external nasal branches innervating the anterior part of the septum, the lateral wall of the nasal cavity, the nasal bone, and skin to the tip of the nose. The anterior ethmoidal foramen is located medially from the halfway point between the posterior palpebral fold and the eyebrow and at a depth of 1.5 cm. A small gauge needle (25–27 G) is used to complete the block, completing a continuous injection while removing the needle. Needle insertion 9 mm superior to the superior border of the medial canthal tendon will prevent injury to the lacrimal sac.[27][28][29]
Infraorbital Block
The maxillary branch of the trigeminal nerve (V2) courses along the inferior orbit within the infraorbital groove before emerging through the infraorbital foramen, located approximately 1 cm below the inferior orbital rim. The infraorbital nerve and its branches provide sensory innervation to the lower eyelid, lateral nose, upper lip, and maxillary teeth. This nerve block is therefore useful for a variety of lower eyelid and maxillofacial procedures.[30]
The block is performed through either an intraoral or extraoral approach and requires careful landmark identification. The intraoral approach is accomplished by inserting a needle into the mucosa superiorly parallel to the upper second bicuspid and advancing it toward the foramen. Careful palpation is necessary to prevent injection into the foramen. The extraoral approach is straightforward. However, adjunctive vasoconstrictive medication is not recommended, given the proximity of the facial nerve.
Zygomaticofacial and Zygomaticotemporal Nerve Blocks
The zygomatic nerve originates from V2 as it exits the pterygopalatine fossa. The zygomaticofacial branch emerges onto the face within the zygomatic bone and innervates the overlying skin. It can be targeted by injecting laterally at the inferolateral orbital rim. The zygomaticotemporal branch enters the temporal fossa through a foramen and innervates the overlying temporal skin. Additionally, the zygomaticotemporal nerve provides secretomotor fibers to the lacrimal nerve.[31] Anesthetic placed towards the concave surface of the posterolateral orbital rim and advanced inferiorly to the level of the lateral canthus will target the zygomaticotemporal branch.
Facial Nerve Blocks
Facial nerve blocks may be used in ambulatory surgery as a single technique or combined with general anesthesia or intravenous sedation. The facial nerve block for ocular surgery targets the periocular branches of the facial nerve with the aim to prevent excessive blinking during surgery via orbicular muscle akinesia. The three classic techniques include the O’Brien’s block, Atkinson block, and van Lint block.[12] Modifications and alternative techniques have been described in the literature with variable efficacy. This mixed success is attributed to the normal anatomical variants of the facial nerve that exists in the population.[12][32]
The utilization of local anesthesia alone is ideal for patients who would not be optimal candidates for general anesthesia. Advantages include a conscious and alert patient, the avoidance of general anesthetics, and its associated risks of systemic complications such as postoperative confusion, gastrointestinal upset, and cardiovascular compromise. Using a facial nerve block as a local anesthesia technique may be preferable in a number of ophthalmic surgeries, including cataract surgery, pterygium excision, keratoplasty, dacryocystorhinostomy, glaucoma procedures, and minor oculoplastic surgeries. The akinetic blocks may be used in conjunction with general anesthesia in cases requiring more complex intraocular and periocular procedures.
- O'Brien Technique
The O’Brien block achieves temporary palsy of the orbicularis oculi muscle at the facial nerve trunk. The original version of this block is completed proximally at the level of the mandible near the condyloid process. The modified O’Brien block uses a posterior and inferior position along the most superior palpable aspect of the mandible ramus, approximately 3 cm above the mandible angle. This modified technique provides a highly effective nerve block and lid akinesia at a site closer to the stylomastoid foramen.[12][32]
Either form of this technique leads to akinesia of the facial/temporal and zygomatic branches of the facial nerve that supplies the motor function to the orbicularis oculi.[32] Although the O’Brien block achieves a more akinetic effect than its counterparts, it carries risks of unilateral facial nerve paresis and nerve root injury. Due to the proximity of the glossopharyngeal and vagus nerves, the internal carotid artery, internal jugular vein, and parotid gland, injection sites closer to the stylomastoid foramen in the modified O’Brien version has been implicated in severe complications such as respiratory and vocal cord paralysis.[33][32]
- Atkinson Technique
The Atkinson block injection site is located at the inferior margin of the zygomatic bone; this provides blockade of mostly the facial/temporal branch of the facial nerve and the zygomatic branches depending on the patient’s facial nerve anatomy.[34]
- Van Lint Technique
The van Lint block provides a more peripheral blockade, achieving effect at the facial, temporal, and zygomatic terminal ramifications at the rim of the orbit.[12] It should be noted that the Van Lint block carries a risk of eyelid edema and lid hemorrhage, which may contribute to postoperative ptosis.
- Upper and Lower Eyelid Blocks
The eyelid blocks involve infiltration of local anesthesia directly into the eyelids to achieve akinesia of the orbicularis oculi. The upper eyelid block is completed at 1cm above the medial canthus, and the lower eyelid block is performed 0.5 cm below the medial canthus.[2][12] The lid block has been shown as a highly effective proximal block of the facial nerve without bearing the risks of direct nerve root trauma.[35]
Comparison of Facial Nerve Blocks
Variable success at orbicularis muscle akinesia has been reported between the three blocks. One study comparing the effectiveness of O’Brien, Atkinson, Van Lint, and eyelid blocks during cataract surgery found that the modified O’Brien and Lid blocks provided the best akinesia with nearly no muscle activity recorded post-injection.[12] The Atkinson and van Lint blocks did not produce the same complete akinesia results. The main attributive factor is the numerous anastomoses that are known to exist between the facial, temporal, and cervical branches, as well as between the temporal, zygomatic, and buccal branches of the facial nerve. These anastomoses prevent complete paresis of the orbicularis muscle in cases of trauma but also prevent the selective block of both the temporal and zygomatic branches of the facial nerve.[12]
Complications
Complications vary greatly depending on the specific technique performed. Retrobulbar blockade carries increased risks of retrobulbar hemorrhage, damage to the globe, optic nerve, or extraocular muscles, and central spread with brain stem depression. The risks of other periocular local and regional blocks include:
- Bleeding, hematoma, ecchymosis
- Edema, local tissue damage
- Infection
- Vascular injection of anesthetic
- Temporary or permanent nerve injury
- Systemic toxicity of the anesthetic
- Allergic reaction to the anesthetic
Clinical Significance
Appropriate selection and delivery of anesthesia are essential to perform procedures safely and improve patient comfort. For surgical procedures localized to a specific anatomical area, direct anesthetic infiltration is often adequate. However, for larger procedures or those requiring minimal tissue distortion, regional nerve blockade offers a distinct advantage in that a relatively smaller amount of anesthesia is necessary to anesthetize a specific area.
Given the complex sensory innervation of the face, knowledge of anatomy is required to safely and effectively deliver local and regional anesthesia. In addition, targeted anesthesia, either through local tissue infiltration or regional nerve blockade, enables the delivery of an anesthetic as an adjunct or alternative to systemic anesthesia.
Enhancing Healthcare Team Outcomes
The administration of local anesthesia is best performed in conjunction with a healthcare team. Physicians, nurses, pharmacists, and other assistants are all responsible for confirming the appropriateness and safety of any proposed procedure. A focused patient assessment is essential, including discussing prior adverse drug reactions or complications related to previous anesthetic use. A team approach with verification of appropriate medication, concentration, maximum dosage, and patient monitoring techniques is needed to minimize potential complications.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Eke T, Anesthesia for glaucoma surgery. Ophthalmology clinics of North America. 2006 Jun; [PubMed PMID: 16701162]
Rafailov L,Kulak A,Weedon J,Shinder R, Comparison of Lidocaine Gel-Assisted Transconjunctival and Transcutaneous Local Anesthesia for Outpatient Eyelid Surgery. Ophthalmic plastic and reconstructive surgery. 2015 Nov-Dec; [PubMed PMID: 25675169]
Level 1 (high-level) evidenceHutchisson B,Nicoladis CB, Topical anesthesia--a new approach to cataract surgery. AORN journal. 2001 Sep; [PubMed PMID: 11565156]
Kohnen T, Is intracameral anesthetic application the final solution to topical anesthesia for cataract surgery? Journal of cataract and refractive surgery. 1999 May; [PubMed PMID: 10330622]
Bryant JS,Busbee BG,Reichel E, Overview of ocular anesthesia: past and present. Current opinion in ophthalmology. 2011 May; [PubMed PMID: 21427572]
Level 3 (low-level) evidenceKhurana AK,Sachdeva RK,Gombar KK,Ahluwalia BK, Evaluation of subconjunctival anaesthesia vs peribulbar anaesthesia in cataract surgery. Acta ophthalmologica. 1994 Dec; [PubMed PMID: 7747584]
Level 1 (high-level) evidenceMeades K,Schebesta A, Subconjunctival local anaesthesia. Australian and New Zealand journal of ophthalmology. 1993 Nov; [PubMed PMID: 8148152]
Level 3 (low-level) evidenceDavison M,Padroni S,Bunce C,Rüschen H, Sub-Tenon's anaesthesia versus topical anaesthesia for cataract surgery. The Cochrane database of systematic reviews. 2007 Jul 18; [PubMed PMID: 17636839]
Level 1 (high-level) evidenceMyers WG,Edelhauser HF, Shortage of bisulfite-free preservative-free epinephrine for intracameral use. Journal of cataract and refractive surgery. 2011 Mar; [PubMed PMID: 21333884]
Level 3 (low-level) evidenceNaor J,Slomovic AR, Anesthesia modalities for cataract surgery. Current opinion in ophthalmology. 2000 Feb; [PubMed PMID: 10724831]
Level 3 (low-level) evidenceFolino TB,Mahboobi SK, Regional Anesthetic Blocks StatPearls. 2021 Jan; [PubMed PMID: 33085385]
Schimek F,Fahle M, Techniques of facial nerve block. The British journal of ophthalmology. 1995 Feb; [PubMed PMID: 7696239]
Lindquist TD,Kopietz LA,Spigelman AV,Nichols BD,Lindstrom RL, Complications of Nadbath facial nerve block and a review of the literature. Ophthalmic surgery. 1988 Apr; [PubMed PMID: 3362499]
Level 3 (low-level) evidenceNapier A,De Jesus O,Taylor A, Supraorbital Nerve Block StatPearls. 2021 Jan; [PubMed PMID: 30725622]
Lodhi O,Tripathy K, Anesthesia For Eye Surgery StatPearls. 2021 Jan; [PubMed PMID: 34283497]
Cass GD, Choices of local anesthetics for ocular surgery. Ophthalmology clinics of North America. 2006 Jun; [PubMed PMID: 16701157]
Rüschen H,Aravinth K,Bunce C,Bokre D, Use of hyaluronidase as an adjunct to local anaesthetic eye blocks to reduce intraoperative pain in adults. The Cochrane database of systematic reviews. 2018 Mar 2; [PubMed PMID: 29498413]
Level 1 (high-level) evidencePrabhakar A,Lambert T,Kaye RJ,Gaignard SM,Ragusa J,Wheat S,Moll V,Cornett EM,Urman RD,Kaye AD, Adjuvants in clinical regional anesthesia practice: A comprehensive review. Best practice [PubMed PMID: 31791560]
Adams L, Adjuvants to local anaesthesia in ophthalmic surgery. The British journal of ophthalmology. 2011 Oct; [PubMed PMID: 21441237]
Polania Gutierrez JJ,Riveros Perez E, Retrobulbar Block StatPearls. 2021 Jan; [PubMed PMID: 32491380]
Nanayakkara D,Manawaratne R,Sampath H,Vadysinghe A,Peiris R, Supraorbital nerve exits: positional variations and localization relative to surgical landmarks. Anatomy [PubMed PMID: 29644106]
Yaghoubian JM,Aminpour S,Anilus V, Supertrochlear Nerve Block StatPearls. 2021 Jan; [PubMed PMID: 32644465]
Molliex S,Navez M,Baylot D,Prades JM,Elkhoury Z,Auboyer C, Regional anaesthesia for outpatient nasal surgery. British journal of anaesthesia. 1996 Jan; [PubMed PMID: 8672358]
Kim SH,Shin HJ, Effects of an infratrochlear nerve block on reducing the oculocardiac reflex during strabismus surgery: a randomized controlled trial. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2018 Sep; [PubMed PMID: 29730798]
Level 1 (high-level) evidenceBoselli E,Bouvet L,Augris-Mathieu C,Bégou G,Diot-Junique N,Rahali N,Vertu-Ciolino D,Gérard C,Pivot C,Disant F,Allaouchiche B, Infraorbital and infratrochlear nerve blocks combined with general anaesthesia for outpatient rhinoseptoplasty: A prospective randomised, double-blind, placebo-controlled study. Anaesthesia, critical care [PubMed PMID: 26549134]
Level 1 (high-level) evidenceMistry RK,Al Khalili Y, Neuroanatomy, Infratrochlear Nerve StatPearls. 2021 Jan; [PubMed PMID: 31869160]
Takahashi Y,Kinoshita H,Nakano T,Asamoto K,Ichinose A,Kakizaki H, Anatomy of anterior ethmoidal foramen, medial canthal tendon, and lacrimal fossa for transcutaneous anterior ethmoidal nerve block in Japanese individuals. Ophthalmic plastic and reconstructive surgery. 2014 Sep-Oct; [PubMed PMID: 25025384]
Kim HS,Lee HK,Jeong HS,Shin HW, Decreased postoperative pain after reduction of fractured nasal bones using a nerve block of the anterior ethmoidal nerve. International journal of oral and maxillofacial surgery. 2013 Jun; [PubMed PMID: 23528745]
Level 2 (mid-level) evidenceSeitchik MW, Anterior ethmoid nerve block for the treatment of nasal fractures. Plastic and reconstructive surgery. 1971 Aug; [PubMed PMID: 5561895]
Nardi NM,Alvarado AC,Schaefer TJ, Infraorbital Nerve Block StatPearls. 2021 Jan; [PubMed PMID: 29763056]
Shafique S,M Das J, Anatomy, Head and Neck, Maxillary Nerve StatPearls. 2021 Jan; [PubMed PMID: 31194417]
Ellis GS, Akinesia of the facial nerve: a laboratory investigation of the surgical anatomy. Transactions of the American Ophthalmological Society. 1968; [PubMed PMID: 5720853]
Hessemer V, [Peribulbar anesthesia versus retrobulbar anesthesia with facial nerve block. Techniques, local anesthetics and additives, akinesia and sensory block, complications]. Klinische Monatsblatter fur Augenheilkunde. 1994 Feb; [PubMed PMID: 8170098]
ATKINSON WS, Akinesia of the orbicularis. American journal of ophthalmology. 1953 Sep; [PubMed PMID: 13080401]
Ismail AR,Anthony T,Mordant DJ,MacLean H, Regional nerve block of the upper eyelid in oculoplastic surgery. European journal of ophthalmology. 2006 Jul-Aug; [PubMed PMID: 16952086]