Introduction
An anembryonic pregnancy is characterized by a gestational sac that forms and grows while an embryo fails to develop. Although the terms anembryonic pregnancy and blighted ovum are synonymous, the latter is falling out of favor with the more descriptive former term. Anembryonic pregnancy constitutes a significant but unknown proportion of miscarriages, with the American Pregnancy Association estimating anembryonic pregnancy to constitute half of all first-trimester miscarriages. Approximately 15% of all clinically recognized pregnancies end in first-trimester loss, with live births occurring in only 30% of all pregnancies.[1][2] Many patients with early pregnancy loss (including anembryonic pregnancies) are unaware of their miscarriage, particularly when the loss occurs in the early stages of pregnancy.
Early Pregnancy Loss
In the first trimester, the terms early pregnancy loss, miscarriage, or spontaneous abortion are often used interchangeably. Early pregnancy loss is defined as the spontaneous loss of a pregnancy before 13 weeks of gestation.[3][4]
Miscarriage
The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) define miscarriage as the loss of a pregnancy before 20 weeks of gestation or the ejection or removal of an embryo or fetus that weighs ≤500 g. This definition in the United States may vary based on state laws.[3][5]
Biochemical Miscarriage
Biochemical miscarriage is a loss that occurs after a positive urine pregnancy test (hCG) or a raised serum beta-hCG before ultrasound or histological verification and confirmation.
Clinical Miscarriage
Clinical miscarriage is diagnosed when ultrasound examination or histologic evidence has confirmed the existence of an intrauterine pregnancy. Clinical miscarriage is classified as early (before 12 weeks of pregnancy) and late (12 to 20 weeks of pregnancy).
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The exact etiology of anembryonic pregnancies is difficult to ascertain. The etiological factors for anembryonic pregnancies are generally understood and studied in the broader context of early pregnancy loss (EPL), which includes both embryonic and anembryonic pregnancies. Etiologies include the following:
- Morphological abnormalities of an embryo prevent implantation or prevent long-term survival of the embryo after implantation. These morphological abnormalities are thought to be related to chromosomal abnormalities.[4]
- Chromosomal abnormalities that collectively include autosomal trisomy, polyploidy, sex chromosomal polysomy, and monosomy X likely represent the most common etiologies for EPL. Trisomies are the primary fetal chromosomal abnormality in sporadic cases of miscarriage (30% of all miscarriages) and represent 60% of chromosomally abnormal miscarriages (recurrent miscarriages). Trisomies with monosomy X (15% to 25%) and triploidy (12% to 20%) account for over 90% of all chromosomal abnormalities found in sporadic cases of miscarriage. According to a study by Edmonds in 1992, trisomy 16 gave rise to rudimentary embryonic growth with an empty sac, while other trisomies often resulted in early embryonic demise.[6]
- Other genetic and chromosomal abnormalities include translocations, inversions, single-gene perturbations, and placental mosaicism.[7] Consanguineous marriages resulting in anembryonic pregnancies have also been noted, suggesting the role of single-gene determinants.[8] There is a probable link between DNA damage in sperm and miscarriage.[9]
- Obesity and advanced maternal age are well-established factors associated with EPL.[10]
- Infection is thought to play a role. Tuberculosis in the developing world, as well as reproductive tract infections worldwide, can predispose to EPL.[11] The complications of genital tract infections, including intrauterine adhesions, can impede implantation and embryo growth.
- Malformations of the uterus, including didelphic, bicornuate, and septate uteri, can impede or prevent the long-term implantation of an embryo.
- Immunologic disorders in the mother, such as NK cell dysfunction, autoantibodies, hereditary, and acquired thrombophilia, among others, can lead to the maternal immunological rejection of the implanting embryo in the uterus, resulting in miscarriage.
- Hormonal factors such as low levels of progesterone and endocrinological disorders, including thyroid autoimmunity and thyroid dysfunction, play a complex role in miscarriage. Polycystic ovarian syndrome is also associated with infertility and pregnancy loss.
- Alcohol consumption has been established to have an associated increased risk of miscarriage.[12]
Epidemiology
Although difficult to definitively establish, anembryonic pregnancy possibly represents half of all miscarriages in the first trimester of pregnancy.[13][14] The incidence of early pregnancy loss (before 12 weeks) is estimated to be about 15% of clinically evident conceptions, with significant variations in incidence based on patient age. The incidence ranges from 10% in women aged 20 to 24 years to 51% in women aged 40 to 44 years.[15] A prior history of early pregnancy loss also predisposes a patient to miscarriage.[16]
History and Physical
The signs and symptoms of an anembryonic pregnancy can potentially mirror those of an ectopic pregnancy. Anembryonic pregnancy is often incidentally noted on an initial first-trimester obstetric sonogram. If an anembryonic pregnancy progresses to an early pregnancy loss, the patient can present with abdominal cramping and vaginal bleeding. Conversely, early pregnancy loss in the setting of an anembryonic pregnancy can be clinically silent.
Evaluation
Clinical signs and symptoms, a pregnancy test, and an ultrasound exam confirm the diagnosis of an anembryonic pregnancy.
A pregnancy test can be obtained using urine or serum hCG levels.
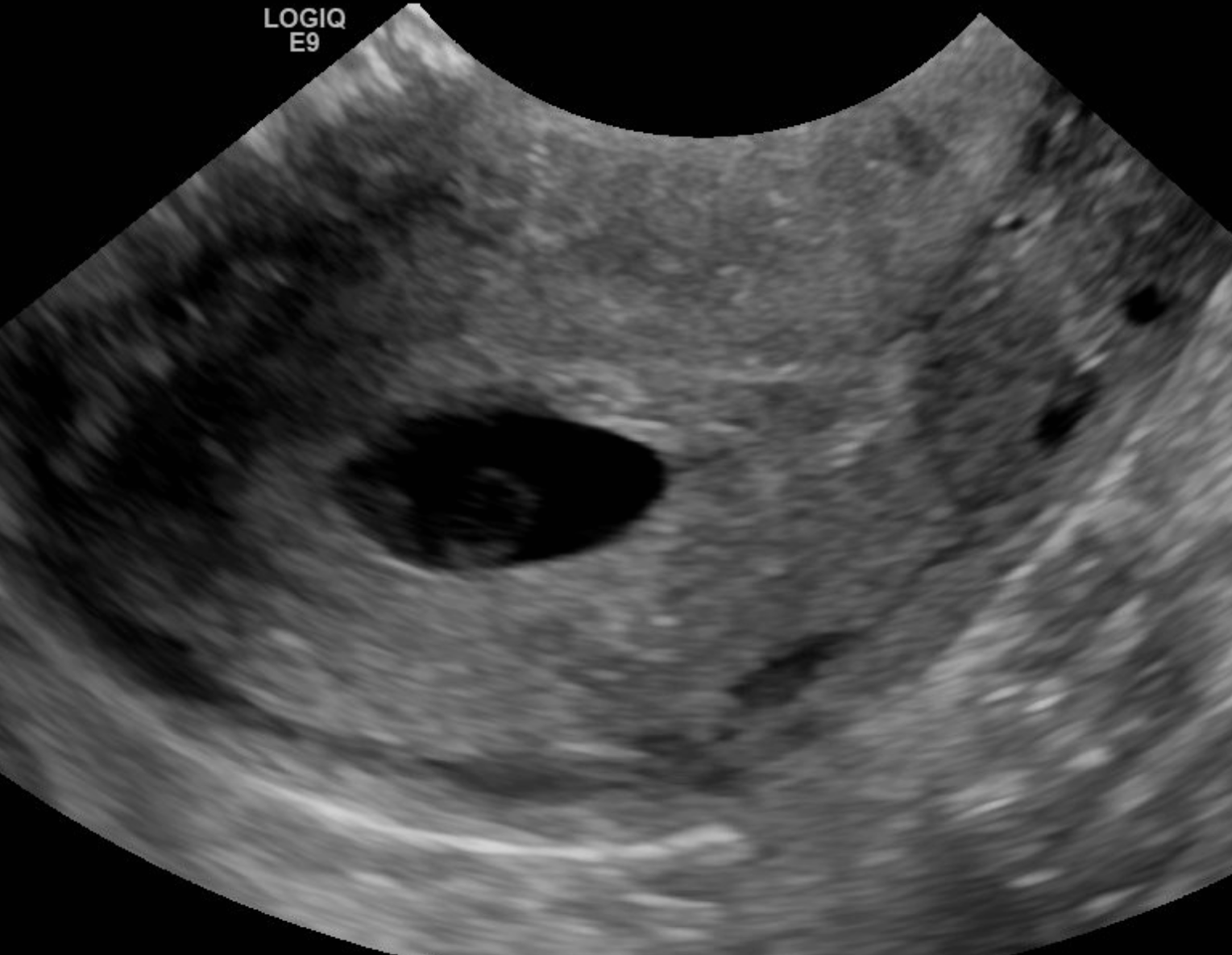
Ultrasound examination (transabdominal or transvaginal) classically demonstrates an empty gestational sac without an embryo (see Image. Anembryonic Pregnancy)
An anembryonic pregnancy is established on ultrasound imaging when no discernable embryo is seen in a gestational sac with a mean sac diameter of ≥25 mm.
Alternatively, an anembryonic pregnancy can be established when there is no embryo on a follow-up endovaginal scan:
- ≥11 days after a scan demonstrating a gestational sac with a yolk sac but an absent embryo
- ≥ 2 weeks (14 days) after a scan demonstrating a gestational sac without an embryo or a yolk sac
Treatment / Management
The 3 treatment options for early pregnancy loss include expectant management, medical management, and surgical treatment. Medical management with mifepristone and/or misoprostol and surgical management are effective treatment options for anembryonic gestations. Ultimately, the decision on which option to proceed with is based on an informed conversation between the patient and clinician.
- Expectant Management
- This constitutes the "watchful waiting" approach.
- The patient is closely followed without intervention for spontaneous and complete passage of tissue.
- Repeat sonograms and trending hCG levels may be employed to confirm the complete passage of tissue.
- A negative hCG level after the passage of tissue vaginally is recommended.
- Medical Management
- This employs mifepristone and/or misoprostol administered vaginally, orally, or buccally, with various doses and timing regimens that may be utilized.
- Optimal dosage is an ongoing area of research.
- This management option allows for a more predictable treatment course.
- Surgical Treatment
- Surgical management employs uterine evacuation with a manual vacuum or dilation and curettage.
- This approach is frequently employed in patients with hemodynamic instability or who cannot tolerate the cramping and bleeding associated with medical management.
- Uterine aspiration/evacuation is quicker to complete, especially when performed on an outpatient basis.[5]
Differential Diagnosis
The differential diagnosis for an anembryonic pregnancy includes the following:
- Pseudogestational sac, which reveals a small amount of intrauterine fluid but no pregnancy tissue
- Early intrauterine pregnancy
- An ectopic pregnancy
- Implantation bleeding from an otherwise viable pregnancy
- Gestational trophoblastic disease
- Complications relating to a viable pregnancy
Prognosis
The prognosis and successful management of an anembryonic pregnancy depends on various factors, including gestational age. The prognosis is generally considered good with all 3 management options.
- Expectant management: In a meta-analysis of 20 studies, expectant management and medical management were deemed acceptable treatment options for incomplete abortion.[17]
- Medical management: Medical management is more successful with multiple-dose regimens of misoprostol. Patients with incomplete abortions are treated more successfully with medical management than expectant management.
- Surgical Treatment: At least 1 large randomized control trial determined a higher success rate with surgical treatment than with medical management, although it concluded the general safety of both treatment options.[18]
Complications
Serious complications of treatment are uncommon. Such complications can include the following:
- Heavy bleeding/hemorrhage
- Uterine perforation from surgical management
- Infection or septic abortion, which can be fatal
- Complications from a missed diagnosis of ectopic pregnancy [5]
Consultations
Necessary consultations may include the following:
- OB/GYN
- Primary care clinician
- Psychologist/psychiatrist
- Emergency department physician
- Radiologist/sonographer(especially when there is a concern for ectopic pregnancy)
Deterrence and Patient Education
The following represent critical points in patient education:
- Pregnant patients in the first trimester should be advised to present to their emergency department if they experience severe pain or heavy vaginal bleeding (2 pads per hour for approximately 2 consecutive hours).
- Signs and symptoms of infection should be discussed with patients, especially following surgical management and with those choosing expectant management.
- Treatment with mifepristone and misoprostol can cause a febrile reaction, which can be misinterpreted as a sign of infection.
- Prophylactic antibiotics are not routinely administered except with surgical management.
- Patients should adhere to follow-up sonograms and outpatient appointments, particularly when additional doses of misoprostol are considered clinically necessary.
- A miscarriage can be a traumatic experience for a patient. Reassurance and empathy are vital in helping patients navigate the grieving process.
Pearls and Other Issues
Pertinent pearls include the following:
- Pregnancy loss is a common complication in the first trimester of pregnancy
- Most losses occur in the first trimester
- Early pregnancy loss without embryo development is likely due to chromosomal and genetic abnormalities.
- There are specific sonographic criteria for diagnosing an anembryonic pregnancy.
- A pseudogestational sac, an ectopic pregnancy, and an early viable pregnancy are important differential diagnoses to consider when evaluating an anembryonic pregnancy.
- Expectant management, medical treatment, and surgical treatment are the 3 primary options for management.
Enhancing Healthcare Team Outcomes
Interprofessional teams are more effective when they work collaboratively and efficiently. Developing a well-defined strategy for managing anembryonic pregnancies is vital. Healthcare teams should establish standardized protocols for diagnosis, treatment options, and patient counseling. An evidence-based approach should guide decision-making, ensuring strategies align with the latest research and guidelines.
Each healthcare team member, from physicians to advanced care practitioners, nurses, and pharmacists, has distinct responsibilities. Physicians are responsible for diagnosing and developing treatment plans for anembryonic pregnancies. Nurses provide patient care, emotional support, and education. Pharmacists may be involved in prescribing or dispensing medications. All team members must respect patients' autonomy by providing clear information about their condition and available choices, including expectant management, medication, and surgery. Mental health professionals play a critical role in following up with patients and ensuring the appropriate mental health management of a possibly traumatic experience for patients.
Physicians, advanced care practitioners, nurses, and pharmacists should communicate and collaborate seamlessly to provide consistent patient-centered care. Confirming the diagnosis of an anembryonic pregnancy can be difficult by ultrasound at times. Communication with the radiologist relaying hCG lab values and patient presentation can help avoid a missed diagnosis of an ectopic pregnancy. The sonographer is also essential in accurately evaluating a patient to exclude an ectopic pregnancy appropriately. Patients presenting with complications on initial presentation or from treatment often present to the emergency department. Close communication between an emergency department provider and an OB/GYN specialist includes communicating a detailed and thorough patient history and physical exam. This particularly includes signs of sepsis and/or hemodynamic instability.
Regular team meetings, continuing education, and shared decision-making processes enhance team performance. Reducing the physical complications and emotional impact of these losses through a coordinated, patient-centered approach is essential for providing high-quality care. Recognizing the unique contributions of each team member and fostering a culture of mutual respect and trust further strengthens the team's ability to provide optimal care for patients with anembryonic pregnancies.
Media
(Click Image to Enlarge)
References
Macklon NS, Geraedts JP, Fauser BC. Conception to ongoing pregnancy: the 'black box' of early pregnancy loss. Human reproduction update. 2002 Jul-Aug:8(4):333-43 [PubMed PMID: 12206468]
Level 3 (low-level) evidenceGoldhaber MK, Fireman BH. The fetal life table revisited: spontaneous abortion rates in three Kaiser Permanente cohorts. Epidemiology (Cambridge, Mass.). 1991 Jan:2(1):33-9 [PubMed PMID: 2021664]
Level 2 (mid-level) evidenceYin Y, Zhang T, Dai Y, Bao Y, Chen X, Lu X. The effect of plasma lead on anembryonic pregnancy. Annals of the New York Academy of Sciences. 2008 Oct:1140():184-9. doi: 10.1196/annals.1454.042. Epub [PubMed PMID: 18991916]
Hertig AT, Rock J. Searching for early fertilized human ova. Gynecologic investigation. 1973:4(3):121-39 [PubMed PMID: 4593973]
Sakko Y, Turesheva A, Gaipov A, Aimagambetova G, Ukybassova T, Marat A, Kaldygulova L, Amanzholkyzy A, Nogay A, Khamidullina Z, Mussenov Y, Almawi WY, Atageldiyeva K. Epidemiology of spontaneous pregnancy loss in Kazakhstan: A national population-based cohort analysis during 2014-2019 using the national electronic healthcare system. Acta obstetricia et gynecologica Scandinavica. 2023 Dec:102(12):1682-1693. doi: 10.1111/aogs.14669. Epub 2023 Sep 4 [PubMed PMID: 37667510]
Nikitina TV, Sazhenova EA, Tolmacheva EN, Sukhanova NN, Vasilyev SA, Lebedev IN. Comparative cytogenetics of anembryonic pregnancies and missed abortions in human. Vavilovskii zhurnal genetiki i selektsii. 2023 Mar:27(1):28-35. doi: 10.18699/VJGB-23-05. Epub [PubMed PMID: 36923481]
Level 2 (mid-level) evidenceBerglund G. Preparation of antiserum to an antigen of low molecular weight. Nature. 1965 May 1:206(983):523-4 [PubMed PMID: 4953500]
Level 3 (low-level) evidenceShekoohi S, Mojarrad M, Raoofian R, Ahmadzadeh S, Mirzaie S, Hassanzadeh-Nazarabadi M. Chromosomal study of couples with the history of recurrent spontaneous abortions with diagnosed blightded ovum. International journal of molecular and cellular medicine. 2013 Fall:2(4):164-8 [PubMed PMID: 24551808]
Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, Kirkman-Brown J, Coomarasamy A. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Human reproduction (Oxford, England). 2012 Oct:27(10):2908-17. doi: 10.1093/humrep/des261. Epub 2012 Jul 12 [PubMed PMID: 22791753]
Level 2 (mid-level) evidenceCavalcante MB, Sarno M, Peixoto AB, Araujo Júnior E, Barini R. Obesity and recurrent miscarriage: A systematic review and meta-analysis. The journal of obstetrics and gynaecology research. 2019 Jan:45(1):30-38. doi: 10.1111/jog.13799. Epub 2018 Aug 28 [PubMed PMID: 30156037]
Level 1 (high-level) evidencePatki A, Chauhan N. An Epidemiology Study to Determine the Prevalence and Risk Factors Associated with Recurrent Spontaneous Miscarriage in India. Journal of obstetrics and gynaecology of India. 2016 Oct:66(5):310-5. doi: 10.1007/s13224-015-0682-0. Epub 2015 Mar 17 [PubMed PMID: 27486274]
Sundermann AC, Zhao S, Young CL, Lam L, Jones SH, Velez Edwards DR, Hartmann KE. Alcohol Use in Pregnancy and Miscarriage: A Systematic Review and Meta-Analysis. Alcoholism, clinical and experimental research. 2019 Aug:43(8):1606-1616. doi: 10.1111/acer.14124. Epub 2019 Jul 3 [PubMed PMID: 31194258]
Level 1 (high-level) evidenceAndersen LB, Dechend R, Karumanchi SA, Nielsen J, Joergensen JS, Jensen TK, Christesen HT. Early pregnancy angiogenic markers and spontaneous abortion: an Odense Child Cohort study. American journal of obstetrics and gynecology. 2016 Nov:215(5):594.e1-594.e11. doi: 10.1016/j.ajog.2016.06.007. Epub 2016 Jun 8 [PubMed PMID: 27287686]
Homan G, Brown S, Moran J, Homan S, Kerin J. Human chorionic gonadotropin as a predictor of outcome in assisted reproductive technology pregnancies. Fertility and sterility. 2000 Feb:73(2):270-4 [PubMed PMID: 10685527]
Level 2 (mid-level) evidenceMagnus MC, Wilcox AJ, Morken NH, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ (Clinical research ed.). 2019 Mar 20:364():l869. doi: 10.1136/bmj.l869. Epub 2019 Mar 20 [PubMed PMID: 30894356]
Regan L, Braude PR, Trembath PL. Influence of past reproductive performance on risk of spontaneous abortion. BMJ (Clinical research ed.). 1989 Aug 26:299(6698):541-5 [PubMed PMID: 2507063]
Kim C, Barnard S, Neilson JP, Hickey M, Vazquez JC, Dou L. Medical treatments for incomplete miscarriage. The Cochrane database of systematic reviews. 2017 Jan 31:1(1):CD007223. doi: 10.1002/14651858.CD007223.pub4. Epub 2017 Jan 31 [PubMed PMID: 28138973]
Level 1 (high-level) evidenceZhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM, National Institute of Child Health Human Development (NICHD) Management of Early Pregnancy Failure Trial. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. The New England journal of medicine. 2005 Aug 25:353(8):761-9 [PubMed PMID: 16120856]
Level 1 (high-level) evidence