Anatomy, Thorax, Mediastinum Superior and Great Vessels
Anatomy, Thorax, Mediastinum Superior and Great Vessels
Introduction
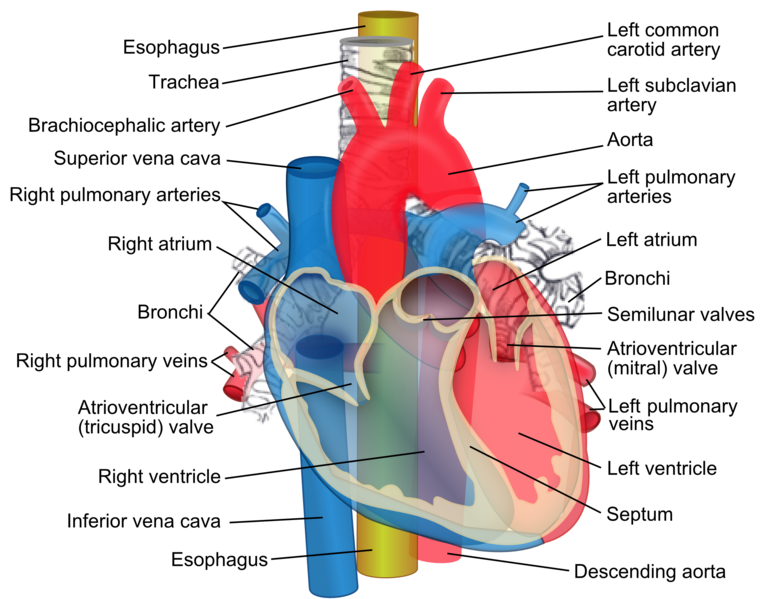
The mediastinum is a large compartment in the thoracic chest that contains vital structures such as the heart and its major blood vessels, as well as the esophagus, trachea, and additional important structures. The superior mediastinum is a triangle-shaped structure that sits at the upper, anterior portion of the chest. The superior mediastinum is most noteworthy for containing the take-off point of the three great branches of the aortic arch: the brachiocephalic trunk (also known as the innominate artery), the left common carotid artery, and the left subclavian artery. The superior mediastinum also contains the origin of the superior vena cava, the thymus, and portions of the esophagus and trachea. The lower mediastinum also contains the pulmonary arteries, which are the final set of great vessels. This article will focus primarily on the great vessels found in the mediastinum.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The first branch of the aortic arch is the brachiocephalic artery. The brachiocephalic artery branches into the right subclavian artery, which supplies the right upper extremity, and then the right common carotid, which brings blood supply to the right side of the head and neck. The arch of the aorta then gives off the left common carotid artery, which goes on to supply the left side of the head and neck. The final major vessel to leave the aortic arch is the left subclavian artery, which supplies the left upper extremity.
There has been significant variation reported in the origin of the brachiocephalic (innominate) artery. High-riding innominate artery is perhaps the most commonly identified anomaly; this can include late take-off from the aorta and, more commonly, a late bifurcation into the right subclavian and right common carotid. This results in a brachiocephalic artery located in the neck, which can present major issues during carotid, thyroid, and parathyroid surgeries. There are also reports of a left brachiocephalic artery in rare cases of transposition of the great vessels.[1][2][3]
The pulmonary trunk arises directly from the right ventricle of the heart and divides almost immediately into the left and right pulmonary arteries. These carry de-oxygenated blood from the right side of the heart to the pulmonary circulation. They then branch into successively smaller arteries. Oxygenated blood eventually returns to the left atrium via the pulmonary veins.
The superior vena cava also resides within the superior mediastinum. Its major tributaries include the two brachiocephalic veins, the left superior intercostal vein, and the azygos vein. The brachiocephalic veins receive blood from the upper extremities via the subclavian veins and from the head and neck via the internal jugular veins. The left superior intercostal veins receive blood from the first three ribs and intercostal spaces. The 4th through 8th left intercostal veins empty into the accessory hemiazygos vein, and the 9th through 11th left intercostal veins empty into the hemiazygos vein. Both the accessory hemiazygos and the hemiazygos vein empty into the azygos vein, as do all the right intercostal veins. The azygos then drains directly into the superior vena cava.
The thymus is the most obvious structure of the superior mediastinum and sits atop the innominate artery. The gland may extend anteriorly against the posterior surface of the sternum.
Blood Supply and Lymphatics
A description of the primary vasculature appeared in the “Structure and Function” section of this article.
The primary lymphatic structure of the mediastinum is the thoracic duct, which runs to the left of the cervical esophagus and enters the junction of the left internal jugular and subclavian veins.
Nerves
Both the vagus and phrenic nerves descend into the mediastinum. Both the proximal trachea and esophagus descend into the superior mediastinum. They may be exposed via a left cervical neck incision.
The left recurrent laryngeal nerve originates from the left vagus and traverses the aortic arch in between the left common carotid artery and the left subclavian artery. The nerve then passes underneath the aortic arch, just adjacent to the ligamentum arteriosum. From here, the nerve descends into the tracheoesophageal groove.
The sympathetic trunk crosses bilaterally next to the vertebral bodies.
Surgical Considerations
Aortitis syndrome refers to inflammation and/or narrowing of the aorta secondary to an autoimmune process, infection, or other systemic inflammation. This syndrome can present at any portion of the aorta: ascending, aortic arch, thoracic or abdominal. Infectious aortitis is typically secondary to septicemia, syphilis, or mycobacterial infection. In particular, syphilis is a common cause of aortitis of the aortic arch, which can lead to the narrowing of the take-off point of the great vessels of the superior mediastinum. Non-infectious causes of aortitis include Takayasu arteritis, giant cell arteritis, and Bechet’s disease. Surgery is often necessary for the event of a severe narrowing of the aorta or one of the great vessels. The inflammatory process should be controlled prior to any operative intervention. Both endovascular and open procedures have been studied. Endovascular techniques have been shown to decrease perioperative complications, but long-term efficacy appears comparable.[4][2][5]
The thymus is a small triangular gland containing lymphoid tissue. In the infant, the thymus is quite large and can occupy most of the space behind the manubrium. It is a primary lymphatic organ responsible for the development of cellular immunity. The thymus reaches its maximum just after puberty and then gradually atrophies. In the adult, only fat cells and small fibrous strands remain. In about a quarter of individuals who develop myasthenia gravis, the thymus may be enlarged (thymoma). The thymus gland is accessed via the median sternotomy and removed in toto. Great care should be taken during the excision of the thymoma as the phrenic nerve runs laterally and can easily be damaged. The only way to determine if the thymoma is benign or malignant is by visual inspection of its location and invasion of adjacent structures. Many tumors receive treatment with surgery and radiation therapy. Malignant lesions tend to be invasive and adherent to nearby structures. Adherent lesions treated with surgery increase the risk of vascular compromise during the procedure. Care is necessary to carefully dissect any vessels to which the mass is adherent, particularly the brachiocephalic trunk, but also including the remaining great vessels. Thirty percent of tumors are too advanced for surgery and will require chemotherapy.[6]
Clinical Significance
Since the superior vena cava traverses the superior mediastinum, any number of causes can result in obstruction. While lung cancer is the most common cause, other causes include aortic aneurysms, mediastinal fibrosis, pericarditis, thrombosis secondary to venous catheter placement, and infections like histoplasmosis. Superior vena cava syndrome most commonly presents in middle-aged individuals with edema and plethora of the head, distended neck veins, and headache. Once diagnosed, the condition requires treatment as it could progress to the brain and/or upper airway edema. Radiotherapy is often used as the initial treatment when the diagnosis is uncertain. In the past, surgery was the approach to reconstruct the superior vena cava, but today percutaneous angioplasty and stenting offer symptomatic relief within 24 to 48 hours.[7][8][9]
Stenosis of the brachiocephalic artery is a rare but well-reported syndrome that presents due to a narrowing of the brachiocephalic trunk, leading to decreased supply to the right subclavian and right common carotid arteries. This condition has been reported secondary to aortitis syndrome, atherosclerosis, or congenital narrowing. The most commonly recommended treatment is percutaneous transluminal angioplasty with stent placement. The preferred access point for this procedure is the femoral artery.[10][11][12]
Aneurysms of the great vessels are not uncommon in the superior mediastinum. Surgeons usually need to perform a median sternotomy incision to get access to these aneurysms. Access to the proximal left subclavian artery usually requires a very high left thoracotomy.
Other Issues
Massive emboli can lodge in the bifurcation of the pulmonary arteries, leading to a condition known as a saddle embolus, which results in significantly decreased blood flow through the pulmonary circuit. This condition creates rapid and severe hypoxia, as well as significant right heart strain that can lead to cardiovascular collapse. This represents a potential medical emergency, requiring immediate intra-arterial tPA and possible embolectomy.[13][14]
The presence of a rapid bleed into the trachea found during a tracheostomy might represent a trachea-innominate fistula. This condition results from a connection between the brachiocephalic vein and the trachea and is an absolute surgical emergency associated with a high mortality rate.
Lymphomas are also known to occur in the superior mediastinum. These tumors present in young adults between the second and the fourth decade of life. While most mediastinal lymphomas are B-cell lymphomas, which typically have an indolent course, about 5% will be very aggressive lesions. Most patients with lymphoma of the superior mediastinum present with vague chest pain, dysphagia, dyspnea, night sweats, hoarseness, or weight loss. The symptoms typically depend on the size of the lesion. Imaging procedures are essential in determining the size and location of these lesions. A mediastinal lymph node biopsy is usually necessary to confirm the diagnosis. Most patients with mediastinal lymphomas will have their condition managed with chemotherapy and/or radiation. Lymphomas may spread via the lymphatic system, which includes the mediastinal and peri-aortic nodes. If this occurs, any attempt at surgical resection will necessitate extreme caution for the great vessels. While surgical resection is often not indicated, awareness of surrounding vessels is of the utmost importance.[15][16]
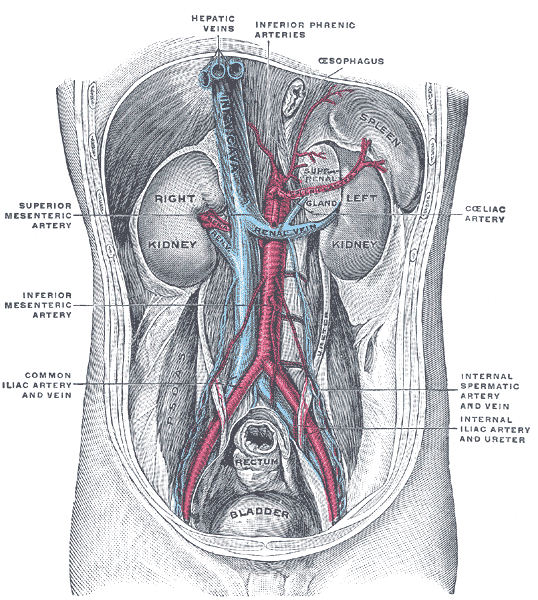
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Dalati HA, Jabbr MS, Kassouma J. High-riding brachiocephalic (innominate) artery during surgical tracheostomy. BMJ case reports. 2018 Apr 18:2018():. pii: bcr-2017-221802. doi: 10.1136/bcr-2017-221802. Epub 2018 Apr 18 [PubMed PMID: 29669763]
Level 3 (low-level) evidenceSubasi ID, Yoruk O, Sipal S, Karakaya AD, Şengöz F. Brachiocephalic artery anomaly at the neck: importance during minimally invasive video-assisted parathyroidectomy. The Journal of craniofacial surgery. 2013 Nov:24(6):e750-73. doi: 10.1097/SCS.0b013e31829ad242. Epub [PubMed PMID: 24220490]
Penslar J, Menard C, Lee S. Isolated Left Brachiocephalic Artery in Transposition of the Great Arteries. The Canadian journal of cardiology. 2018 Oct:34(10):1369.e13-1369.e15. doi: 10.1016/j.cjca.2018.07.420. Epub 2018 Jul 27 [PubMed PMID: 30269835]
Keser G, Aksu K. Diagnosis and differential diagnosis of large-vessel vasculitides. Rheumatology international. 2019 Feb:39(2):169-185. doi: 10.1007/s00296-018-4157-3. Epub 2018 Sep 17 [PubMed PMID: 30221327]
Gaudric J, Dennery M, Jouhannet C, Kagan N, Saadoun D, Chiche L, Koskas F. [Aortitis and surgery]. La Revue de medecine interne. 2016 Apr:37(4):284-91. doi: 10.1016/j.revmed.2015.12.017. Epub 2016 Jan 18 [PubMed PMID: 26797187]
Berghmans T, Durieux V, Holbrechts S, Jungels C, Lafitte JJ, Meert AP, Moretti L, Ocak S, Roelandts M, Girard N. Systemic treatments for thymoma and thymic carcinoma: A systematic review. Lung cancer (Amsterdam, Netherlands). 2018 Dec:126():25-31. doi: 10.1016/j.lungcan.2018.10.018. Epub 2018 Oct 18 [PubMed PMID: 30527189]
Level 1 (high-level) evidenceSalavitabar A, Flyer JN, Torres AJ, Richmond ME, Crystal MA, Turner ME, Chai P, Zuckerman WA. Transcatheter stenting of superior vena cava obstruction after pediatric heart transplantation: A single-center experience assessing risk factors and outcomes. Pediatric transplantation. 2018 Nov:22(7):e13267. doi: 10.1111/petr.13267. Epub 2018 Jul 11 [PubMed PMID: 29992703]
Noor Khairiah AK, Mohamad Nazrulhisham MN, Hazman MN. Malignant obstruction of superior vena cava: Endovascular stenting using Y-configuration stent in stent technique. The Medical journal of Malaysia. 2018 Dec:73(6):407-409 [PubMed PMID: 30647215]
Zimmerman S, Davis M. Rapid Fire: Superior Vena Cava Syndrome. Emergency medicine clinics of North America. 2018 Aug:36(3):577-584. doi: 10.1016/j.emc.2018.04.011. Epub 2018 Jun 12 [PubMed PMID: 30037444]
Nomura M, Kida S, Yamashima T, Yamashita J, Yoshikawa J, Matsui O. Percutaneous transluminal angioplasty and stent placement for subclavian and brachiocephalic artery stenosis in aortitis syndrome. Cardiovascular and interventional radiology. 1999 Sep-Oct:22(5):427-32 [PubMed PMID: 10501899]
Level 3 (low-level) evidenceRangel-Castilla L, Levy EI, Siddiqui AH. Direct Cervical Carotid Stenting and Angioplasty of Right Internal Carotid Artery and Brachiocephalic Artery Ostial Stenoses With Flow Reversal: 2-Dimensional Operative Video. Operative neurosurgery (Hagerstown, Md.). 2019 Feb 1:16(2):269-270. doi: 10.1093/ons/opy113. Epub [PubMed PMID: 29846684]
van Hattum ES, de Vries JP, Lalezari F, van den Berg JC, Moll FL. Angioplasty with or without stent placement in the brachiocephalic artery: feasible and durable? A retrospective cohort study. Journal of vascular and interventional radiology : JVIR. 2007 Sep:18(9):1088-93 [PubMed PMID: 17804769]
Level 2 (mid-level) evidenceTAYLOR FW. Saddle embolus of the aorta. A.M.A. archives of surgery. 1951 Jan:62(1):38-49 [PubMed PMID: 14789346]
Shum D, Gore NM. Saddle pulmonary embolus. The Journal of the American Osteopathic Association. 2015 May:115(5):345. doi: 10.7556/jaoa.2015.069. Epub [PubMed PMID: 25938533]
Messmer M, Tsai HL, Varadhan R, Swinnen LJ, Jones RJ, Ambinder RF, Shanbhag SP, Borowitz MJ, Wagner-Johnston N. R-CHOP without radiation in frontline management of primary mediastinal B-cell lymphoma. Leukemia & lymphoma. 2019 May:60(5):1261-1265. doi: 10.1080/10428194.2018.1519812. Epub 2019 Jan 18 [PubMed PMID: 30656983]
Hüttmann A, Rekowski J, Müller SP, Hertenstein B, Franzius C, Mesters R, Weckesser M, Kroschinsky F, Kotzerke J, Ganser A, Bengel FM, La Rosée P, Freesmeyer M, Höffkes HG, Hertel A, Behringer D, Prange-Krex G, Griesshammer M, Holzinger J, Wilop S, Krohn T, Raghavachar A, Maschmeyer G, Brink I, Schroers R, Gaska T, Bernhard H, Giagounidis A, Schütte J, Dienst A, Hautzel H, Naumann R, Klein A, Hahn D, Pöpperl G, Grube M, Marienhagen J, Schwarzer A, Kurch L, Höhler T, Steiniger H, Nückel H, Südhoff T, Römer W, Brinkmann M, Ose C, Alashkar F, Schmitz C, Dürig J, Hoelzer D, Jöckel KH, Klapper W, Dührsen U. Six versus eight doses of rituximab in patients with aggressive B cell lymphoma receiving six cycles of CHOP: results from the "Positron Emission Tomography-Guided Therapy of Aggressive Non-Hodgkin Lymphomas" (PETAL) trial. Annals of hematology. 2019 Apr:98(4):897-907. doi: 10.1007/s00277-018-3578-0. Epub 2019 Jan 4 [PubMed PMID: 30610279]