Introduction
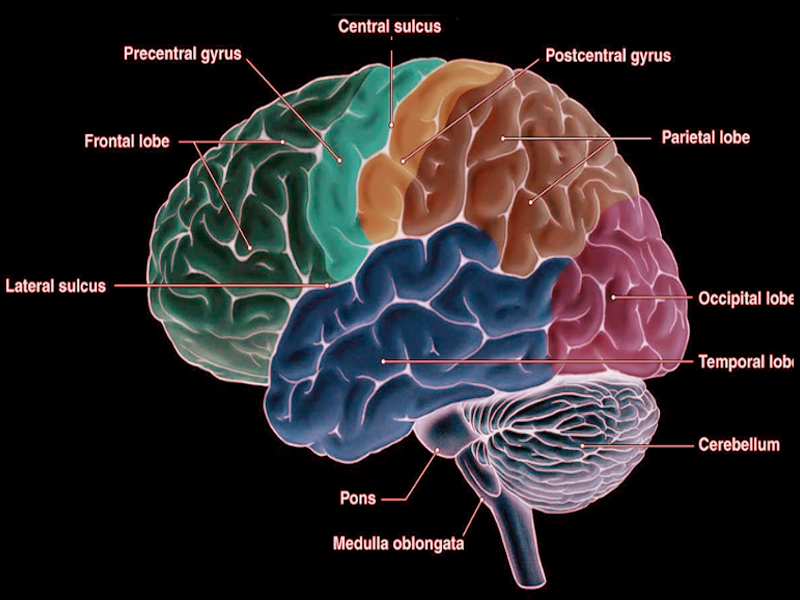
The precentral gyrus is on the lateral surface of each frontal lobe, anterior to the central sulcus. It runs parallel to the central sulcus and extends to the precentral sulcus.[1] The primary motor cortex is located within the precentral gyrus and is responsible for the control of voluntary motor movement. Since the precentral gyrus is the location of the primary motor cortex, several motor pathways originate within it. The corticospinal tract, corticobulbar tract, and cortico-rubrospinal tract all begin within the precentral gyrus.[2]
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The precentral gyrus is the anatomical location of the primary motor cortex, which is responsible for controlling voluntary motor movement on the body's contralateral side. The primary motor cortex is topographically organized and creates a somatotropic map. Texts often refer to this map as the motor homunculus, or “little man.” The organization of the homunculus is in such a way that that the medial part of the paracentral lobule contains the motor control of the foot, leg, and thigh, and the precentral gyrus contains the motor control for the gluteal area, trunk, upper extremity, hand, digits, and head. The motor homunculus within the precentral gyrus is organized in such a way that trunk is more medial, the upper limb and hand are more laterally, and the far lateral regions, just superior to the lateral fissure, contain the motor control for the face and head. Regions of the motor homunculus that require more fine-tuned motor control are larger than the others. Specifically, the areas for the hand and face are disproportionally larger than others. In addition to the primary motor cortex, the precentral gyrus also contains a portion of the supplementary motor cortex, which is involved in the planning of voluntary limb movement.[3]
The precentral gyrus is a part of the cerebral cortex and contains the neocortex. Neocortex contains six different cell layers (I-VI), which are numbered starting from the cortical surface and move inward. Layer I mainly consists of the dendrites from neurons and axons of the deeper layers. Layers II and III contain neurons that extend to other layers of the cortex, layer IV receives inputs from the thalamus, layer V consists of projections to other subcortical areas, such as the basal ganglia, brainstem, and spinal cord, and layer VI contains projections to the thalamus. Different areas of the cerebral cortex consist of varying layer thickness depending on the function of that region. The primary motor cortex consists of larger layers III and IV due to the numerous projections to the brainstem, spinal cord, and other cortical areas to control voluntary movement. The primary motor cortex does not receive a lot of sensory information from the thalamus, so there is a thinner layer IV. Giant pyramidal cells of Betz are also found within the primary motor cortex and project down to the lumbosacral segments of the spinal cord. The primary motor cortex receives afferent inputs from the premotor cortex, sensory cortex, thalamus, basal ganglia, and cerebellum. The neurons within the primary motor cortex contribute to the establishment of the corticobulbar, corticospinal, and cortico-rubrospinal tracts.[2][4][2]
Embryology
The precentral gyrus is part of the cerebral cortex, which forms from the telencephalon. By day 32 of development, the cerebral hemispheres emerge as two bubble-like structures on the telencephalon. The cerebral cortices eventually form from the thinner roof and lateral aspects of the cerebral hemispheres. Initially, the cerebral hemispheres are smooth, but from six to nine months of development, the cerebral cortex forms its gyri and sulci.[1]
Blood Supply and Lymphatics
The precentral gyrus is supplied by the anterior cerebral artery and the middle cerebral artery, which are both branches off of the internal carotid artery. The superior division of the middle cerebral artery supplies the more lateral surface of the precentral gyrus, while the anterior cerebral artery supplies the medial aspect of the precentral gyrus. The precentral gyrus, along with the majority of the cortical surface, is drained by the superficial cerebral veins, which then empty into the superior sagittal sinus.[5][6][5]
Nerves
Motor Pathways
The primary motor cortex is located within the precentral gyrus and is responsible for the regulation of voluntary motor movements. Due to its significant role in motor movements, the precentral gyrus is the initiating point for several motor pathways, including, the corticospinal tract, the corticobulbar tract, and the cortico-rubrospinal tract.[2]
The Corticospinal Tract
Voluntary motor movements are largely under the control of the corticospinal tract.[7] This tract can also be referred to as the pyramidal tract due to its triangular shape in the medulla. The corticospinal tract is formed from neurons in the precentral gyrus, premotor area, and postcentral gyrus, with 80% of its fibers supplied by the primary motor cortex. The path continues from the cortex and moves through the posterior limb of the internal capsule. From there, it travels to the middle area of the cerebral peduncle and forms multiple axon fascicles in the basis pontis. After the pons, the corticospinal tract enters the ipsilateral medullary pyramid. It is at this point where most fibers cross to the contralateral side at the pyramidal decussation, located at the medullary-spinal cord junction. These crossed fibers continue down the spinal cord in the lateral funiculus. The lateral funiculus is also somatotopically organized with the fibers supplying the sacral region is the most lateral, followed by the thoracic and lumbar fibers, and then the cervical fibers traveling more towards the midline. These fibers synapse directly and indirectly, through interneurons, on alpha and gamma lower motor neurons, especially those associated with more distal muscles.[2]
Fibers that do not cross contralaterally in the pyramidal decussation, travel down the spinal cord in the anterior funiculus, creating the anterior corticospinal tract. These fibers decussate in the anterior white commissure and also synapse directly and indirectly, through interneurons, on alpha and gamma lower motor neurons. Axons in the anterior corticospinal tract usually synapse on lower motor neurons supplying more medial muscles.[2]
The Corticobulbar Tract
The corticobulbar tract is a similar pathway to the corticospinal tract, except instead of supplying the muscles of the body, it supplies the muscles of the face and head. This tract primarily starts in the lateral aspect of the primary motor cortex, located within the precentral gyrus. From there it travels through the genu of the internal capsule, cerebral peduncle, basis pontis, and on to the medullary pyramids on the ipsilateral side. Fibers then go on to synapse on the motor nuclei of cranial nerves, both directly and indirectly through interneurons. The corticobulbar tract sends direct bilateral fibers to the hypoglossal nerve, facial nerve, and trigeminal nerve motor nuclei. The motor nucleus of the facial nerve is a special case in this tract. The part that supplies the muscles around the mouth and lower face receives only contralateral fibers from the corticobulbar tract. While the part that supplies the forehead and muscles of the upper face receives bilateral fibers originating from both sides.[2]
Cortico-Rubro-Spinal Tract
The cortico-rubrospinal tract is a motor pathway that aids in the regulation of flexor muscle movements of the extremities. This corticospinal system controls spinal cord lower motor neurons indirectly. It begins as the corticorubral tract in the primary motor cortex within the precentral gyrus and sends fibers down to the ipsilateral red nucleus of the midbrain. From there, it continues as the rubrospinal tract, as the fibers cross over in the ventral tegmental decussation and continue down the lateral brainstem. The fibers then intermix with fibers from the lateral corticospinal tract and travel down the spinal cord in the lateral funiculus. The axons from the rubrospinal tract then synapse on alpha and gamma motor neurons of the muscles associated with the flexion of the extremities.[2]
Physiologic Variants
The pattern of gyri within the cerebral hemispheres varies between individuals, but the primary sulci that form in fetal life, the central and precentral sulci, are relatively constant.[8]
Surgical Considerations
Several conditions exist that necessitate the need for surgery within or very close to the precentral gyrus. Glioma resection and resection to decrease the number of seizures in refractory epilepsy are two discussed here. In both cases, the potential for postoperative motor deficits needs to be kept in mind, when determining the risk-benefit ratio for patients.[9][10]
Tumors located within the primary motor cortex of the precentral gyrus are frequently considered unresectable due to the likelihood of creating new neurological deficits. However, the primary goal of glioma surgery is to achieve the maximal safe resection because the extent of this resection has been shown to increase survival for both low- and high-grade gliomas. New neurosurgical techniques have been introduced to achieve the maximal safe resection while decreasing the consequences seen postoperatively. One technique showing promise is the use of intraoperative stimulation mapping, which has been shown to decrease the incidence of severe neurological deficits by 60%. Even with new techniques, the risks of resecting gliomas in the precentral gyrus are still present. Up to 20% of patients who have undergone a resection involving the primary motor cortex or precentral gyrus have reported postoperative permanent motor deficits. The risk of a patient developing a motor deficit can still be up to 30% even with experienced hands, direct cortical stimulation, and intraoperative neuromonitoring. Given the potential for risks during precentral gyrus resections, patients should be counseled prior to surgery on the high probability of having a new or worsened motor dysfunction. However, these deficits usually partially or completely resolve with time. Several techniques have been found to help neurosurgeons perform safer resections. Surgical planning assistance is available with the use of preoperative transcranial magnetic stimulation (TMS), which is also useful to aid with functional MRI and diffusion tensor imaging (DTI)-based tractography and is beneficial when ruling out if there is functional involvement of the primary motor cortex. Using TMS may lead to greater gross-total glioma resection. Continuous motor mapping with direct cortical stimulation is being tried as a new technique to help make precentral gyrus resections safer.[10][11][12][13][12][11][10]
Surgical resection can be a treatment for frontal lobe epilepsy that is refractory to antiepileptic drugs. A subset of these patients have seizures that begin in the primary motor cortex, making the precentral gyrus an important target for resection. However, finding the precentral gyrus during surgery can be challenging due to a layer of arachnoid mater and being occupied by large veins. Sulcal anatomy should be verified preoperatively through imaging and then confirmed by gyral anatomy and stereotactic navigation intraoperatively. At greater depths, the sulci become more visible. The best way to identify the precentral gyrus during surgery is through the precentral “knob,” as it is the most common aspect of the precentral gyrus between individuals. This portion of the precentral gyrus functions as the hand area of the primary motor cortex and appears as looking like an omega sign. When this aspect is not visible, the central sulcus can also be utilized to locate the precentral gyrus.[9][14][9]
Resections in the motor cortex have demonstrated effectiveness as a treatment option for patients with refractory epilepsy that begins within the precentral gyrus. Out of 280 patients, 85% showed some seizure improvement. These improvements did not come without deficits, as 58% of patients had an immediate postoperative motor deficit, and 23% had a long-term motor deficit. These motor deficits display a certain pattern of recovery. Immediately after surgery, there is paresis of the affected area for about two weeks. Following those two weeks, recovery begins in the proximal aspect of the limb and travels distally over the next couple of months. For the upper extremity, shoulder movement is seen first, followed by elbow flexion, elbow extension, wrist flexion, and finally return of hand function. The lower extremity strength tends to recover better than upper extremity strength, with the most common functional outcome being the return of ambulation without assistance. For resections involving the facial area of the primary motor cortex, the functional outcomes are facial symmetry and language function. In 37 patients, 20% noted a facial weakness, and 40% reported immediate postoperative dysphagia. Most patients had a resolution of postoperative dysphagia, with only 8% reporting long term dysphagia.[9]
Clinical Significance
The precentral gyrus is the anatomical location of the primary motor cortex and is responsible for the control of voluntary movement. Lesions occurring within the precentral gyrus affect upper motor neurons, and therefore present with upper motor neuron signs. Since the precentral gyrus is above the pyramidal decussation, upper motor signs will present on the contralateral side of the body. Symptoms of upper motor neuron dysfunction include muscle weakness, distal muscles are usually affected more than proximal, increased muscle tone with spasticity, increased muscle stretch reflexes, and the presence of pathologic reflexes, for example, the Babinski sign. Upper motor neuron signs will also present with little to no muscle atrophy.[15]
The precentral gyrus can also be affected by strokes, and symptoms can aid in localizing the site of the stroke. A stroke in the superior division of the middle cerebral artery will affect the more lateral aspects of the precentral gyrus; this would present with contralateral face and arm weakness with upper motor neuron signs. A stroke in the middle cerebral artery affects other areas besides the precentral gyrus, so it is likely to also present with contralateral hemisensory loss of the arm and face, and if in the dominant hemisphere, Broca aphasia may also be present. A stroke involving the anterior cerebral artery will affect the more medial aspects of the precentral gyrus, presenting with contralateral leg weakness with upper motor signs. A stroke involving the anterior cerebral artery will also be likely to demonstrate hemisensory loss of the contralateral leg.[16]
Media
References
Ribas GC. The cerebral sulci and gyri. Neurosurgical focus. 2010 Feb:28(2):E2. doi: 10.3171/2009.11.FOCUS09245. Epub [PubMed PMID: 20121437]
Lemon RN. Descending pathways in motor control. Annual review of neuroscience. 2008:31():195-218. doi: 10.1146/annurev.neuro.31.060407.125547. Epub [PubMed PMID: 18558853]
Level 3 (low-level) evidenceSchott GD. Penfield's homunculus: a note on cerebral cartography. Journal of neurology, neurosurgery, and psychiatry. 1993 Apr:56(4):329-33 [PubMed PMID: 8482950]
Mountcastle VB. The columnar organization of the neocortex. Brain : a journal of neurology. 1997 Apr:120 ( Pt 4)():701-22 [PubMed PMID: 9153131]
Level 3 (low-level) evidenceFrigeri T, Paglioli E, de Oliveira E, Rhoton AL Jr. Microsurgical anatomy of the central lobe. Journal of neurosurgery. 2015 Mar:122(3):483-98. doi: 10.3171/2014.11.JNS14315. Epub 2015 Jan 2 [PubMed PMID: 25555079]
Ugur HC, Kahilogullari G, Coscarella E, Unlu A, Tekdemir I, Morcos JJ, Elhan A, Baskaya MK. Arterial vascularization of primary motor cortex (precentral gyrus). Surgical neurology. 2005:64 Suppl 2():S48-52 [PubMed PMID: 16256841]
Jang SH. The role of the corticospinal tract in motor recovery in patients with a stroke: a review. NeuroRehabilitation. 2009:24(3):285-90. doi: 10.3233/NRE-2009-0480. Epub [PubMed PMID: 19458437]
Kido DK, LeMay M, Levinson AW, Benson WE. Computed tomographic localization of the precentral gyrus. Radiology. 1980 May:135(2):373-7 [PubMed PMID: 7367629]
Ostergard TA, Miller JP. Surgery for epilepsy in the primary motor cortex: A critical review. Epilepsy & behavior : E&B. 2019 Feb:91():13-19. doi: 10.1016/j.yebeh.2018.06.036. Epub 2018 Jul 23 [PubMed PMID: 30049575]
Magill ST, Han SJ, Li J, Berger MS. Resection of primary motor cortex tumors: feasibility and surgical outcomes. Journal of neurosurgery. 2018 Oct:129(4):961-972. doi: 10.3171/2017.5.JNS163045. Epub 2017 Dec 8 [PubMed PMID: 29219753]
Level 2 (mid-level) evidenceDe Witt Hamer PC, Robles SG, Zwinderman AH, Duffau H, Berger MS. Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012 Jul 10:30(20):2559-65. doi: 10.1200/JCO.2011.38.4818. Epub 2012 Apr 23 [PubMed PMID: 22529254]
Level 1 (high-level) evidenceObermueller T, Schaeffner M, Gerhardt J, Meyer B, Ringel F, Krieg SM. Risks of postoperative paresis in motor eloquently and non-eloquently located brain metastases. BMC cancer. 2014 Jan 14:14():21. doi: 10.1186/1471-2407-14-21. Epub 2014 Jan 14 [PubMed PMID: 24422871]
Level 2 (mid-level) evidenceObermueller T, Schaeffner M, Shiban E, Droese D, Negwer C, Meyer B, Ringel F, Krieg SM. Intraoperative neuromonitoring for function-guided resection differs for supratentorial motor eloquent gliomas and metastases. BMC neurology. 2015 Oct 20:15():211. doi: 10.1186/s12883-015-0476-0. Epub 2015 Oct 20 [PubMed PMID: 26487091]
Yousry TA, Schmid UD, Alkadhi H, Schmidt D, Peraud A, Buettner A, Winkler P. Localization of the motor hand area to a knob on the precentral gyrus. A new landmark. Brain : a journal of neurology. 1997 Jan:120 ( Pt 1)():141-57 [PubMed PMID: 9055804]
Level 3 (low-level) evidenceWalker HK, Hall WD, Hurst JW, Stern LZ, Bernick C. The Motor System and Gait. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:(): [PubMed PMID: 21250232]
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet (London, England). 1991 Jun 22:337(8756):1521-6 [PubMed PMID: 1675378]