Introduction
The angle of Louis is the eponymous name given to the sternal angle or the manubriosternal joint (see Image. Sternum). The angle of Louis is an important anatomical landmark, serving as a crucial reference point in clinical examinations and medical procedures. For example, clinicians use the sternal angle to guide stethoscope placement when auscultating heart and lung sounds. Radiologists also use this site as a reference point for assessing the positions of various thoracic structures in imaging studies.
The joint is slightly flexible in younger individuals due to inadequate development. Complete fusion of the angle of Louis generally occurs at approximately 30 years of age. Anomalies of the manubriosternal junction pose challenges in the clinical examination, radiological diagnosis, and therapy of thoracic conditions.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Structure
The sternum consists of the manubrium, body, and xiphisternum. The manubrium is the widest and thickest of these segments, situated superiorly. The suprasternal (jugular) notch is at the manubrium's superior border, palpable between the clavicular heads. This nearly triangular bone measures 4 cm in length and lies at the level of the T3 and T4 bodies. The 1st rib's costal cartilage fuses with the lateral aspect of the manubrium inferolateral to the clavicular notch.
The sternal angle lies at the T4 to T5 intervertebral (IV) disk level. The manubrium and sternal body lie in different planes; hence, the angulation at the manubriosternal joint. The 2nd costal cartilage articulates with the lateral border of the joint. Thus, the angle of Louis is a convenient starting point for counting ribs anteriorly since the 1st rib is impalpable beneath the clavicle.[1] The manubriosternal junction or the angle of Louis is palpable as a transverse ridge in most individuals.
Clinicians recognize the manubriosternal joint as a synchondrosis, with soft hyaline cartilage connecting the 2 sternal segments. However, anatomists often classify this junction as a symphysis, joined by tough fibrocartilage and allowing only slight movements.[2]
Function
During inspiration, the vertical diameter of the central thoracic region increases as the diaphragm contracts and descends. During expiration, the lungs' elastic recoil reduces pleural cavity pressure and returns the thorax to its resting size.
Sternal movement during inspiration provides a "pump-handle" mechanism for anterosuperior thoracic expansion. The manubrium limits sternal mobility during this phase, but flexibility at the angle of Louis enables anterosuperior expansion of the chest and abdomen.[3][4]
Embryology
Sternum Development
The mesosternum begins to develop around the 6th gestational week, marked by the formation of craniocaudally oriented mesenchymal bars in the ventrolateral body wall of the developing embryo. From the 6th to 9th gestational weeks, the sternal primordia move medially, elongate, and interact with the growing primordial ribs, forming sternal bars. This process culminates in the midline fusion of these bars, starting from the manubrium and progressing craniocaudally.
By the 10th week, chondrification occurs, forming a single solid cartilaginous rod in the mid-anterior thorax. The caudal extension of these sternal bars beyond the last rib attachment gives rise to the xiphoid process.[5]
Manubrium Development
The development of the manubrium involves 3 distinct mesenchymal primordia: the presternal and paired suprasternal masses. During the 6th gestational week, the presternal mass emerges in the region mediocranial to the sternal bars and later merges with these bars. Simultaneously, the suprasternal masses form between the medial ends of the primordial clavicles and the presternum. The suprasternal masses later fuse with the presternum. This fusion creates the superior manubrial margin and the sternoclavicular joints.[6]
Blood Supply and Lymphatics
Cadaveric studies reveal internal mammary artery branches perforating the sternum at each intercostal level. Associated veins have been identified following a similar course.[7][8] Importantly, in patients undergoing internal mammary harvesting, these perforating arteries anastomose with the intercostal arteries and indirectly with the posterior intercostal arteries. These connections enable collateral blood flow in the area. Despite this arrangement, studies have shown that a period of sternal ischemia ensues immediately after harvesting the internal mammary artery.[9]
Nerves
The intercostal nerves are somatic nerves supplying the sternum and manubrium. The main thoracic nerves supplying the sternum arise from the anterior rami of spinal nerve segments T2 to T6. These nerves stimulate intercostal muscle contraction and provide sensation to the skin. Unlike the lateral thorax, the manubrium and sternum have fewer nerves.
Muscles
The neck and thoracic muscles are directly attached to the manubrium and sternal body. The manubrium is an insertion point of the sternocleidomastoid, sternohyoid, and sternothyroid. The sternal body is an insertion point of the pectoralis major. Occasionally, the sternalis muscle lies superficial to the sternal body (see physiologic variants).
Three layers of intercostal muscles move the manubriosternal joint indirectly by their rib attachments. The external intercostals in the outermost layer have fibers running anteriorly and inferolaterally, elevating the ribs during inspiration. The internal intercostals lie deep to the external intercostals, oriented perpendicularly to the external intercostals. The innermost set of intercostals lies deep to the internal intercostals. These muscles are thin and oriented in the same direction as the internal intercostals.
Physiologic Variants
Sternal angle physiologic variants arise from differences in joint location, joint fusion, and joint angulation. An accessory muscle, the sternalis, is also found in some individuals. The clinical significance of these variations is explained below.
Joint Location
The manubriosternal joint is usually located at the insertion of the 2nd costal cartilage. However, the joint has been shown to extend to the 3rd costal cartilage insertion occasionally, which may affect physical examination and radiologic accuracy.[12]
Joint Fusion
Studies have shown that manubriosternal joint fusion can occur at any age. However, the 5-year age gap between nearly fused and fully fused joints implies a higher likelihood of fusion with advancing age. Notably, joint fusion was abnormal in 66% of cases, indicating that the joint's ability to pivot and increase the chest's front-to-back diameter might not significantly impact respiration in adult life.[10]
Joint Angulation
The reference interval for the sternal angle is 155-175 degrees. Exaggeration of this angle can be seen in some people and can affect thoracic movement.[11]
Sternalis Muscle
Some individuals may have a muscle lying superficially and parallel to the sternum known as the sternalis muscle. This muscle has no clear function but may be confused as a pathological structure or make sternal surgery challenging. The sternalis inserts proximally at the manubrium or superior aspect of the sternal body, but its distal insertion is variable.[12]
Healthcare providers must know these anatomical variants to prevent clinical examination and imaging errors.
Surgical Considerations
Surface Landmark For Thoracic Surgeries
Sternal angle surface landmarks are crucial to thoracic procedures. The 1st rib's impalpability makes the 2nd sternocostal joint at the angle of Louis a convenient starting point for rib counting.
The sternal angle is at the same level as the T4-to-T5 IV level, helping to locate deeper thoracic structures during surgery. The imaginary plane joining these 2 structures demarcates the inferior border of the superior mediastinum. The major structures in the superior mediastinum include the thymus, brachiocephalic veins, superior vena cava (SVC), aortic arch, vagus and phrenic nerves, trachea, and esophagus.
The trachea forms the carina at the level of the sternal angle, bifurcating into the right and left main bronchi. The angle of Louis also marks the level of the ligamentum arteriosum and the point where the left recurrent laryngeal nerve loops below the aortic arch. At this level, the azygos vein also arches anteriorly over the right hilum to enter the SVC, while the thoracic duct crosses over to the left side of the chest from the abdomen.
Sternocostal articulations vary in length in the first 7 ribs. The inferior 5 ribs do not articulate with the sternum. The costochondral junctions align from a point 5 cm from the midline at the sternal angle to 2.5 cm posteroinferior to the 10th costal cartilage.
Sternotomy
Sternotomy is widely regarded as the optimal incision technique in cardiac surgery, with low failure rates and consistently favorable long-term outcomes. Sternotomy's applicability extends to thoracic surgery for procedures involving the mediastinum and pulmonary regions. Proper execution of this procedure minimizes short- and long-term morbidity and mortality after thoracic surgery.
Key steps in the procedure include accurate landmark identification, meticulous midline tissue preparation, careful osteotomy, and targeted bleeding control.[14]
Clinical Significance
Chest Physical Examination
Palpating the sternal angle helps locate the 2nd rib and intercostal spaces when auscultating the chest. Typically, the optimal site for listening to the aortic valve is the right 2nd intercostal space. For the pulmonic valve, it is usually the left 2nd intercostal space. The tricuspid valve is commonly heard between the 4th and 5th intercostal spaces, while mitral valve sounds are best heard in the 5th intercostal space. Accurately locating the intercostal spaces likewise helps diagnose respiratory diseases.[15]
Sternal Variations and Thoracic Injury Tolerance
Age- and sex-related sternal changes have been found to correlate with the risk of thoracic injury. Sternal and manubrial shape, size, and ossification vary with age. The sternum and manubrium are narrower and less ossified in children than adults. Thus, thoracic organ injuries are more prevalent in children than thoracic fractures. Ossification without substantial sternal size and shape changes increases the risk of sternal fractures in adults.[13]
Other Issues
The eponymous name "angle of Louis” is believed to have originated from either Antoine Louis, a French clinician, or Wilhelm Friedrich von Ludwig, a German physician. However, there is no definitive evidence of either origin, and some even speculate that the name originates from another doctor, Pierre Charles Alexandre Louis.
Media
(Click Image to Enlarge)
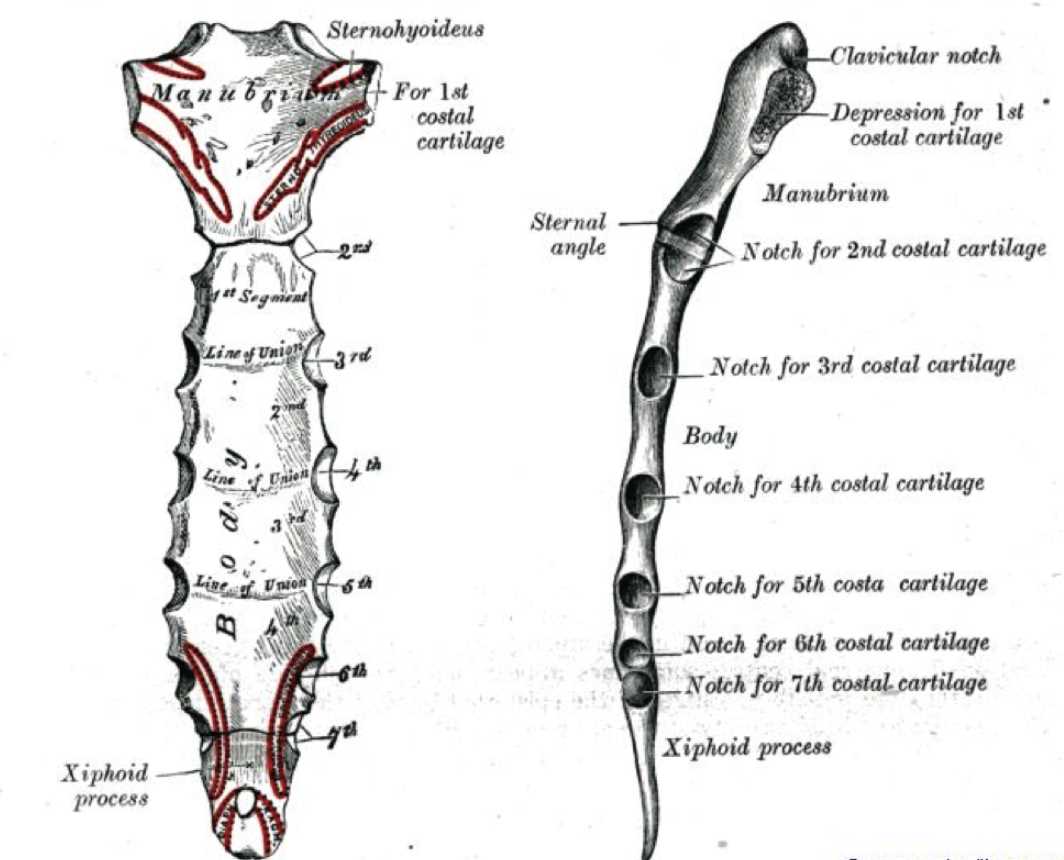
Sternum. This illustration shows anterior and lateral views of the sternum. Anterior view: manubrium, body, and xiphoid process; sternohyoid, sternothyroid, pectoralis major, and diaphragmatic attachments; 1st to 7th sternocostal attachments; articulation of the 2nd rib at the angle of Louis. Lateral view: clavicular notch, depression for the 1st costal cartilage, manubrium, sternal angle, sternal body, xiphoid process, and notches for the 1st to 7th costal cartilages.
Contributed by William Gossman Collection
References
Sayeed RA, Darling GE. Surface anatomy and surface landmarks for thoracic surgery. Thoracic surgery clinics. 2007 Nov:17(4):449-61, v. doi: 10.1016/j.thorsurg.2006.12.002. Epub [PubMed PMID: 18271160]
Sarcinelli JM, Eustáquio-Silva R, da Silva Baptista J. Manubriosternal joint: synchondrosis or symphysis? Analysis of morphology and aging in humans. Surgical and radiologic anatomy : SRA. 2019 Mar:41(3):275-279. doi: 10.1007/s00276-018-2154-6. Epub 2018 Dec 11 [PubMed PMID: 30539209]
Graeber GM, Nazim M. The anatomy of the ribs and the sternum and their relationship to chest wall structure and function. Thoracic surgery clinics. 2007 Nov:17(4):473-89, vi. doi: 10.1016/j.thorsurg.2006.12.010. Epub [PubMed PMID: 18271162]
Cameron HU, Fornasier VL. The manubriosternal joint--ananatomicoradiological survey. Thorax. 1974 Jul:29(4):472-4 [PubMed PMID: 4854943]
Level 3 (low-level) evidenceSadler TW. Embryology of the sternum. Chest surgery clinics of North America. 2000 May:10(2):237-44, v [PubMed PMID: 10803330]
van der Merwe AE, Weston DA, Oostra RJ, Maat GJ. A review of the embryological development and associated developmental abnormalities of the sternum in the light of a rare palaeopathological case of sternal clefting. Homo : internationale Zeitschrift fur die vergleichende Forschung am Menschen. 2013 Apr:64(2):129-41. doi: 10.1016/j.jchb.2013.01.003. Epub 2013 Mar 7 [PubMed PMID: 23473075]
Level 3 (low-level) evidenceHuang AP, Sakata RK. Pain after sternotomy - review. Brazilian journal of anesthesiology (Elsevier). 2016 Jul-Aug:66(4):395-401. doi: 10.1016/j.bjane.2014.09.013. Epub 2016 Apr 23 [PubMed PMID: 27343790]
Berdajs D, Zünd G, Turina MI, Genoni M. Blood supply of the sternum and its importance in internal thoracic artery harvesting. The Annals of thoracic surgery. 2006 Jun:81(6):2155-9 [PubMed PMID: 16731146]
Seyfer AE, Shriver CD, Miller TR, Graeber GM. Sternal blood flow after median sternotomy and mobilization of the internal mammary arteries. Surgery. 1988 Nov:104(5):899-904 [PubMed PMID: 3187903]
Level 3 (low-level) evidenceKirum GG, Munabi IG, Kukiriza J, Tumusiime G, Kange M, Ibingira C, Buwembo W. Anatomical variations of the sternal angle and anomalies of adult human sterna from the Galloway osteological collection at Makerere University Anatomy Department. Folia morphologica. 2017:76(4):689-694. doi: 10.5603/FM.a2017.0026. Epub 2017 Mar 29 [PubMed PMID: 28353306]
Weaver AA, Schoell SL, Nguyen CM, Lynch SK, Stitzel JD. Morphometric analysis of variation in the sternum with sex and age. Journal of morphology. 2014 Nov:275(11):1284-99. doi: 10.1002/jmor.20302. Epub 2014 Jun 17 [PubMed PMID: 24935890]
Saeed M, Murshid KR, Rufai AA, Elsayed SE, Sadiq MS. Sternalis. An anatomic variant of chest wall musculature. Saudi medical journal. 2002 Oct:23(10):1214-21 [PubMed PMID: 12436146]
Ehara S. Manubriosternal joint: imaging features of normal anatomy and arthritis. Japanese journal of radiology. 2010 Jun:28(5):329-34. doi: 10.1007/s11604-010-0438-9. Epub 2010 Jun 30 [PubMed PMID: 20585919]