Introduction
Intralenticular or lens abscess is an uncommon ocular entity resulting from post-trauma, surgery, or metastatic spread.[1] It can also be sterile. Lens abscesses can result secondary to trauma from iron rod, thorn injury, vegetative matter trauma, intralenticular cilia or ophthalmia nodosa, mud injury, dust fall, and stone injury and can also result from blunt trauma to the eye. The lens can be damaged in approximately 30% of perforating eye injuries and 10% of intralenticular foreign bodies lodged in the lens.[2] In cases with blunt trauma, the patient with a lens abscess can have mild symptoms such as pain, blurred vision, and watering. The patients with penetrating trauma present with pain, redness, and sudden onset defective vision.[3]
Slit lamp examination usually reveals a heterogenous lens opacity or pus-filled lenticular cavity. Fundus examination is extremely vital to rule out vitritis and endophthalmitis. Documentation of visual acuity, intraocular pressure, and seidel's test is also essential to assess the treatment response in each case. The other critical investigation of interest which can delineate a lens abscess well are ultrasound B scan, anterior segment optical coherence tomography (ASOCT), and ultrasound biomicroscopy (UBM).[4]
It is also essential to assess the integrity of the posterior capsule as the risk of endophthalmitis is increased manifold when the posterior capsule is ruptured. It is vital to differentiate lens abscesses from traumatic cataracts, as IOL implantation in primary sitting is contraindicated. Diagnosing lens abscess requires clinician expertise, experience, and a high index of suspicion.
Prompt diagnosis, targeted intervention, elimination of microbial load, and regular and meticulous follow-up are the key elements for treatment success. It is also important to take a culture from the lens aspirate to pinpoint the microorganism. In cases with fungal lens abscesses, intravitreal steroids should be avoided. A detailed examination and high clinical suspicion are required to look for complications like secondary glaucoma, cystoid macular edema, and endophthalmitis.[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Bacterial
Staphylococcus Aureus
Staphylococcus is the most common bacteria on the ocular surface and is an aerobic gram-positive organism with low virulence. It can also enter the after penetrating through an exogenous source. The organism is also commonly seen in the aspirate cultured from lens abscess.[6]
Staphylococcus Epidermidis
Staphylococcus epidermidis is also an aerobic, gram-positive bacteria with low virulence. It is commonly seen as a commensal in the eyes or can be associated with postoperative endophthalmitis. The organism has also been cultured from lens aspirate of lens abscess. There can also be a delayed manifestation of postoperative infection because steroids and antibiotics usually mask the initial response. As per previous reports, the microorganism can adhere to the plastic surface of the intraocular lens by producing a glycocalyx polysaccharide which acts as a glue.[7]
Propionibacterium Acne
Propionibacterium acne is commonly seen on the skin and conjunctiva and generally can be considered a contaminant of the ocular surface. The microorganism is an anaerobic, Gram-positive rod, which can also result in a mixed eye infection. The organism is sensitive to penicillin, less sensitive to cephalosporins, and resistant to gentamicin and vancomycin. The microorganism has also been reported commonly from lens abscess, postoperative endophthalmitis after trabeculectomy, and keratoplasty. It also invites the development of phacoantigenic uveitis.[5]
Stenotrophomonas Maltophilia
This microorganism has also been reported in cases with lens abscesses.[8]
Paecilomyces Lilacinus
This is one of the rare species reported in lens abscesses.[9]
Streptococcus Pneumoniae (Pneumococcus)
Pneumococcus causes ulcus serpans and has also been cultured in cases with lens abscesses.[10]
Pseudomonas Aeruginosa
This is another species reported from lens abscess.[11]
Fungal
- Aspergillus niger
- Candida
- Bipolaris
- Cladosporium
- Unidentified hyaline fungi[12]
Epidemiology
Lens abscess is more common in males because most are outdoor workers, especially farmers and factory workers. The lens can be damaged in approximately 30% of perforating eye injuries and 10% of intralenticular foreign bodies lodged in the lens.[13]
Pathophysiology
Once the anterior lens capsule is breached secondary to penetrating or blunt trauma, there is a cortical disturbance. The displaced cortex acts as an excellent nidus for microorganisms' growth and infection eruptions.[14] This results in the lenticular cavity or lens abscess. Since the lens is avascular, topical antibiotics also don't reach the lens cavity directly. It has also been observed that if the anterior capsular tear or rupture is less than 2 mm, it can heal without the proliferation of lens epithelial cells. Intraocular foreign bodies in the lens can also act as a nidus for microorganisms.[1]
Sometimes the foreign body is inert and remains lodged in the lens substance without reaction. If there is a breach of the posterior capsule, the microorganism, retained lens cortex, lens abscess, and chemical toxins released by the microorganism can reach the vitreous cavity and result in an inflammatory cascade.[15]
This results in vitritis and endophthalmitis. Whenever there is delayed endophthalmitis by low-grade pathogens such as P.acne, this is called localized endophthalmitis. In cases with immunosuppression or immunosuppressed patients, the mechanism of ocular immune privilege is also compromised in the anterior chamber, with a disrupted blood-retinal barrier, immunosuppressive factors in the eye, and systemic immune compromise such as anterior chamber-associated immune deviation (ACAID).[16]
History and Physical
History
A detailed history is extremely vital in each case. There can be blunt or penetrating trauma. There can be a history of vegetative matter trauma, needle, fishhook, iron rod, caterpillar hair, stone, mud, clay, metal, and chestnut injury.[17]
Symptoms
The patient can present with blepharospasm, swelling, pain, redness, defective vision, watering, photophobia, floaters, and flashes.[18]
Signs
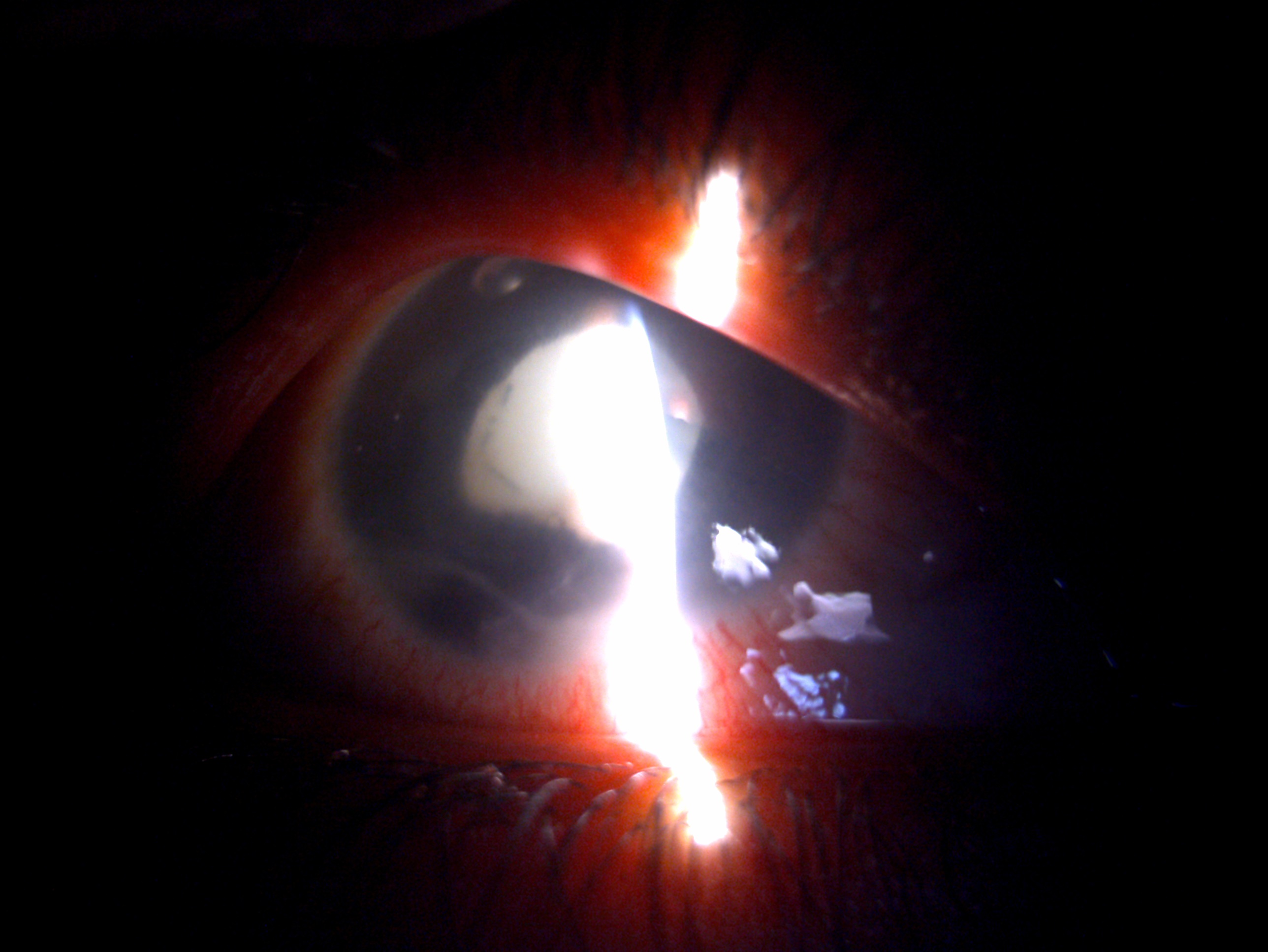
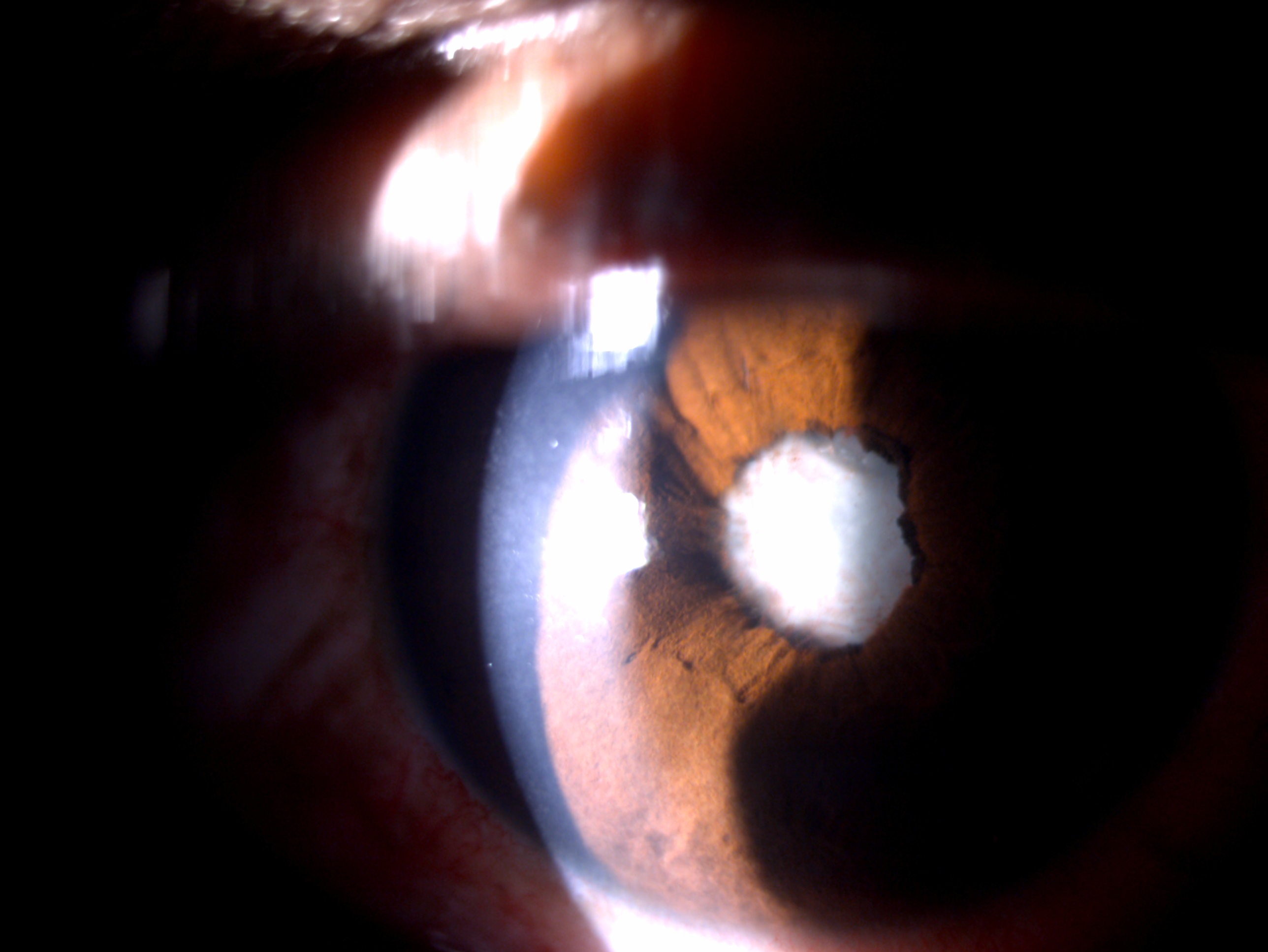
Anterior segment examination may reveal any of the signs such as conjunctival congestion, chemosis, subconjunctival hemorrhage, conjunctival tear, corneal lamellar tear, full thickness cornea tear, self-sealed corneal tear, corneal edema, anterior chamber hypopyon, cells and flare in the anterior chamber, exudates over the iris, iridodialysis, iris bombe, posterior synechiae, relative afferent pupillary defect, sluggish reacting pupil, lens neovascularization, pus-filled lens, or lens abscess. Sometimes the lenticular opacity can take the appearance of yellow-white exudate.[3]
The classic description of a lens abscess is whitish-yellow, dense, homogenous lenticular opacity which is well demarcated from the remaining lens. There can be an injury to the posterior capsule resulting posterior capsular tear. There can be associated vitritis, vitreous membranes, retinal injury, retinal tear, choroidal detachment, and exudates. There can be the associated presence of the foreign body in the anterior or posterior segment.[19]
Intralenticular abscess after fungal infection is less common. In cases with lens abscess due to fungal etiology, the typical findings are uveitis, fungal balls, and fibrinous membrane over the pupil. Fungal lens abscess can also manifest as fungal endophthalmitis, a latency of weeks to months. The timing of symptoms can vary from 24 hours to 6 months post-trauma, with an average of 1.8 months after open globe injury. In fungal endophthalmitis, the symptoms are subacute, and they worsen gradually.[20]
P.acne can also cause acute endophthalmitis, which can present as a full-blown acute infection or chronic low-grade smoldering infection. Chronic endophthalmitis has to be differentiated from phacoantigenic uveitis. In each case of lens abscess, it is essential to document the nature of trauma, presentation duration, onset and severity of symptoms, clinical findings, and visual acuity.[21]
Evaluation
Seidel's Test
In cases with blunt or penetrating trauma, it is always necessary to perform the Seidel and forced Seidel tests to determine the aqueous leak. In case of an aqueous leak, it is mandatory to suture the tear.[22]
Anterior chamber Tap
An anterior chamber should be performed to pinpoint the microorganism from the aqueous aspirate. An aqueous tap can be performed from the paracentesis with a 25 G needle, and 0.1 ml of aqueous can be aspirated for analysis.[23]
Smear Analysis
The lens material can also be taken on KOH smear, Gram stain, and Giemsa stain to determine whether it's a bacterial cause or a fungal cause.[24]
Culture of Lens Aspirate
In cases with the anterior capsular breach and cortical disturbance, the lens material can be removed by either lens aspiration by bimanual irrigation and aspiration or extracapsular cataract extraction approach or by manual small incision cataract surgical approach. Some of the lens material should be sent for culture, which can reveal colonies of a microorganism after 72 hours of growth. The most common culture media used are blood agar, chocolate agar, MacConkey agar, and Sabround Dextrose agar incubated in bacteriological indicator for 16 hours overnight at 37 degrees Celsius.[25]
B Scan Ultrasonography
This is a valuable investigation to rule out vitritis, vitreous membrane, exudates, endophthalmitis, and vitreous hemorrhage. When there is a defect in the posterior capsule, the lenticular matter can be seen extruding through the posterior capsule in the vitreous cavity as a dumbbell. This is called a "dumbbell sign" of lens abscess.[26]
Anterior Segment Optical Coherence Tomography
ASOCT is a vital tool for looking for lens abscesses. It appears as heterogenous lenticular opacity on ASOCT.[1]
Ultrasound Biomicroscopy
UBM has also been listed as a vital tool for delineating lens abscesses.[27]
Computed Tomography
CT scan is vital to localizing any occult foreign body and bony defects.[28]
Treatment / Management
Medical Management
Antibiotics
Antibiotics are the mainstay in managing lens abscesses and safeguarding the eye from endophthalmitis. They can be given as topical, oral, intravenous, subconjunctival, and through the intravitreal route. They help in controlling infection and prevent the spread of abscesses.[29](B2)
Topical
The drugs implicated are
- Moxifloxacin 5 mg/ml
- Fortified tobramycin 14 mg/ml
- Cefazolin 50 mg/ml
- Gentamicin 13.6 mg/ml
- Cefuroxime 50 mg/ml[30]
Subconjunctival
- Cefazolin 100 mg
- Gentamicin 20 mg
- Cefuroxime 125 mg
- Amphotericin B injections 0.01 mg/0.1 cc[31] (A1)
Intravenous
- Cefazolin sodium
- Gentamicin
- Sulphamethoxazole 240 mg
- Trimethoprim 1.2 g[32]
Intravitreal
- Ceftazidime 2 mg
- Vancomycin[33]
Oral
- Flucloxacillin 250 mg
- Pivampicillin 500 mg
- Metronidazole 400 mg
- Ofloxacin 200 mg
- Imipenem 200 mg[26] (B3)
Antifungals
Lens abscesses can also result from fungal species; hence topical, oral, and intracameral antifungals are needed. Topical antifungals have a slower penetration. Accordingly, hourly administration is warranted to get adequate anterior chamber penetration.[34](B3)
Topical
Oral
- Fluconazole 150 mg
- Voriconazole 200mg[36]
Intracameral
Intrastromal
Corticosteroids
Corticosteroids are the mainstay in controlling inflammation. They should be used only when the infection has been controlled. The treating surgeon should be cautious while starting the steroids as it may flare up the abscess and vitritis and lead to the rapid multiplication of microorganisms leading to endophthalmitis. The postoperative steroid regimen is continued after cataract extraction, lens aspiration, and IOL implantation. They can be given through topical and oral routes. In rare cases, if there is persistent posterior segment inflammation, steroids are needed through intravenous and intravitreal routes. Topical steroids help treat conjunctival and scleral inflammation. Steroids can suppress the host's immune system, leading to deeper penetration and proliferation of the fungus. This can result in rebound anterior segment inflammation.[39]
Topical
- Prednisolone acetate 1% 10 mg/ml
- Dexamethasone 0.1%
- Betamethasone 0.05%[40]
Adjuvant Drugs
Cycloplegics
Cycloplegics help to control anterior chamber inflammation, relieve ciliary spasms, relieve pain, break posterior synechiae, prevent the formation of synechiae and prevent the breakdown of the blood-aqueous barrier. They are vital in controlling inflammation.[41]
Drugs Implicated
- Atropine 1%
- Cyclopentolate 1%
- Homatropine 2.5%[42]
Antiglaucoma Drugs
They are needed to control intraocular pressure from uncontrolled inflammation, trabecular meshwork blockage, and trabeculitis. Miotics and prostaglandins are contraindicated in ocular inflammation.
Drugs
Surgical Management
Evacuation of Lens Abscess
Whenever there is a breach in the anterior capsule and cortical matter disturbance, the lenticular material should be removed immediately to prevent endophthalmitis and panophthalmitis.[1]
Lens Aspiration
Young patients have no nucleus with lens matter, and the lenticular matter is mostly cortical. Hence the lens material can be easily aspirated from the paracentesis using bimanual irrigation and aspiration.[44]
Extra Capsular Cataract Extraction (ECCE)
In today's era, ECCE is not practiced much but is a viable option for abscess removal through the superior limbal incision.[45]
Manual Small Incision Cataract Surgery (MSICS)
Another nuclear management option is MSICS, by performing a sclerocorneal tunnel for cataract and abscess removal.[46]
Phacoemulsification
Those surgeons who don't practice ECCE and MSICS can use phacoemulsification as the primary process for lens removal.[47]
Anterior Vitrectomy
In some cases where there is zonular dialysis and posterior capsular breach, vitreous prolapse occurs in the anterior chamber. These cases require automated anterior vitrectomy along with the primary procedure.[48]
Pars Plana Vitrectomy
In cases where there is a nucleus drop, cortical matter drop in the vitreous cavity, non-resolving vitritis, vitreous hemorrhage, and endophthalmitis will require a para plana vitrectomy along with pars plana lensectomy or vitreous lavage.[49]
Aphakia Management
Earlier aphakia management was a matter of debate in cases of lens abscess. Primary IOL implantation reduces the visual rehabilitation time and defers additional surgical procedures. However, it is always advisable to defer primary IOL implantation in these cases. Primary IOL implantation can cause severe uveitis and manifest as cells, flare in the anterior chamber, keratic precipitates at the back of the cornea, posterior synechiae at the back of the cornea, pigments on the IOL, and vitritis. Secondary IOL implantation as a staged procedure has good outcomes in these cases and prevents developing infection and inflammation. A 3-piece hydrophobic IOL is stable for these cases.[50](B2)
Nd YAG Laser Capsulotomy
Nd YAG laser capsulotomy will be needed once posterior capsular opacification is developed. This should be attempted only after three months of quiescence.[8](B3)
100% Oxygen
The administration of 100 percent oxygen has also been tried as a treatment for lens abscess.[46]
Differential Diagnosis
Prognosis
Prognosis in lens abscess cases depends on multiple factors such as type of trauma, the onset of infection, anterior or posterior segment involvement, immune status, timing and nature of the treatment, follow-up, and patient compliance.[1] The prognosis is good if the lens abscess is evacuated immediately and the posterior capsule is intact. The intact posterior capsule prevents the spread of infection to the vitreous cavity and acts as a barrier to the development of vitritis, pan uveitis, and endophthalmitis.[54]
The prognosis is poor if the posterior capsule is breached, the posterior segment is involved, and the immune system is compromised. Delay in surgical intervention is another reason for the poor prognosis of these cases.[54]
Complications
- Amblyopia
- Corneal scar
- Corneal decompensation
- Secondary glaucoma
- Festooned pupil
- Posterior synechiae
- Occlusio pupillae
- Seclusio pupillae
- Intermediate uveitis
- Panuveitis
- Vitritis
- Vitreous membranes
- Cystoid macular edema
- Endophthalmitis
- Panophthalmitis
- Retinal detachment
- Choroidal detachment
Postoperative and Rehabilitation Care
Once the patient has undergone evacuation of lens abscess and culture reports are available targeted antimicrobial therapy should be given. Antibacterials and antifungals are the mainstays depending on the microorganism involved. Culture-negative cases can be treated with combination therapy. A detailed fundus evaluation by a retina specialist is a must in each case to rule out signs of posterior segment infection and inflammation.[55]
Based on the clinical picture, the antibiotics and antifungals can be started at a dose of 6 to 8 times. If, on postoperative day 1, there is an infected corneal tear or hypopyon, and the focus of infection is there, the drugs should be given hourly. The medications should be tapered as the clinical condition of the patient improves. Steroids should be started under close supervision after 1 to 2 weeks of antimicrobial treatment. The patient should be explained and counseled regarding the prognosis of the cases and the need for suture removal and secondary IOL implantation. The patient should be followed up closely and counseled regarding the timely use of medications.[56]
Consultations
Any case of blunt or penetrating trauma presenting to the routine outpatient should be evaluated meticulously to rule out lenticular trauma and the development of an abscess. All patients should be dilated for lenticular examination, and the clinician should be able to differentiate between traumatic cataracts and lens abscesses. These cases should be referred to the cornea clinic or the available cornea consultant for expert inputs and targeted management. A retina specialist should also evaluate all lens abscess cases to rule out posterior segment involvement and prevent the development of any complications.[50]
Deterrence and Patient Education
All patients with a lens abscess should be counseled in detail regarding the nature of ocular pathology and its complications if not managed on time. The patient should be explained the need for lens abscess evacuation and aphakia management. The patient should also be explained that the primary aim is to get rid of the infection, and the secondary aim is visual rehabilitation. Each patient should be clearly explained the prognosis, need for regular follow-up, timely treatment, and staged interventions.[50]
Pearls and Other Issues
Lens abscess is a rarely reported entity in literature. For an astute clinician, it is essential to differentiate traumatic cataracts from lens abscesses as the treatment is poles apart. The prognosis in each case is governed by immune status and posterior segment involvement. If the posterior capsule is breached, there is a high chance of endophthalmitis. Topical antimicrobial therapy and steroids should be used based on the patient's clinical status. Surgical removal of the infective foci is the treatment of choice for lens abscesses.[50]
Enhancing Healthcare Team Outcomes
Lens abscess is a rare clinical entity usually diagnosed only by an experienced cornea or a cataract surgeon. Surgeons play a crucial role in diagnosing and managing these cases. The nurses help recruit the patient to the clinic, assist in slit lamp evaluation, visual acuity evaluation, intraocular pressure management, staining the eye, and counseling the patient.[57] They also help explain the medications to the patient and provide regular follow-ups of these patients. The pharmacist help in arranging the drugs for the patients. The operating room assistants help prepare patients during surgery and meticulously manage these cases. Hence, a good outcome in these cases depends on the interprofessional team's coordinated efforts and open communication between all team members.[58]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Balamurugan S, Gurnani B, Kaur K, Gireesh P, Narayana S. Traumatic intralenticular abscess-What is so different? The Indian journal of radiology & imaging. 2020 Jan-Mar:30(1):92-94. doi: 10.4103/ijri.IJRI_369_19. Epub 2020 Mar 30 [PubMed PMID: 32476758]
Liesegang TJ. Traumatic lens abscess: report of a case. Annals of ophthalmology. 1983 Dec:15(12):1151-4 [PubMed PMID: 6660695]
Level 3 (low-level) evidenceMohseni M, Blair K, Gurnani B, Bragg BN. Blunt Eye Trauma. StatPearls. 2024 Jan:(): [PubMed PMID: 29261988]
Sayadi J,Mekni M,Kallel Z,Choura R,Gouider D,Malek I,Nacef L, Surgical management of a traumatic intralenticular abscess: a case report. The Pan African medical journal. 2022; [PubMed PMID: 35432703]
Level 3 (low-level) evidenceFish LA, Ragen MT, Smith RE, Lean J. Propionibacterium acnes lens abscess after traumatic implantation of intralenticular cilia. American journal of ophthalmology. 1988 Apr 15:105(4):423-4 [PubMed PMID: 3358438]
Level 3 (low-level) evidenceTong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG Jr. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clinical microbiology reviews. 2015 Jul:28(3):603-61. doi: 10.1128/CMR.00134-14. Epub [PubMed PMID: 26016486]
Namvar AE, Bastarahang S, Abbasi N, Ghehi GS, Farhadbakhtiarian S, Arezi P, Hosseini M, Baravati SZ, Jokar Z, Chermahin SG. Clinical characteristics of Staphylococcus epidermidis: a systematic review. GMS hygiene and infection control. 2014:9(3):Doc23. doi: 10.3205/dgkh000243. Epub 2014 Sep 30 [PubMed PMID: 25285267]
Level 1 (high-level) evidenceHutchinson K,Kempster R,Conrad D, Intralenticular abscess caused by Stenotrophomonas maltophilia. Eye (London, England). 2001 Jun; [PubMed PMID: 11450743]
Level 3 (low-level) evidenceTara A, Kobayashi T, Kohmoto R, Fukumoto M, Sato T, Kida T, Ooi Y, Ikeda T. A Case of Fungal Endophthalmitis Caused by Paecilomyces lilacinus that Might Have Spread from the Sclera into the Intraocular Space. Case reports in ophthalmology. 2020 May-Aug:11(2):256-262. doi: 10.1159/000508389. Epub 2020 Jul 1 [PubMed PMID: 32774289]
Level 3 (low-level) evidenceWeiser JN, Ferreira DM, Paton JC. Streptococcus pneumoniae: transmission, colonization and invasion. Nature reviews. Microbiology. 2018 Jun:16(6):355-367. doi: 10.1038/s41579-018-0001-8. Epub [PubMed PMID: 29599457]
Moradali MF, Ghods S, Rehm BH. Pseudomonas aeruginosa Lifestyle: A Paradigm for Adaptation, Survival, and Persistence. Frontiers in cellular and infection microbiology. 2017:7():39. doi: 10.3389/fcimb.2017.00039. Epub 2017 Feb 15 [PubMed PMID: 28261568]
Brooks DE,Taylor DP,Plummer CE,Quinn R,Kallberg ME,Sheppard B,Barrie KP,Blackwood SE,Nunnery CM,Ben-Shlomo G,Clark CJ,Woodworth AA, Iris abscesses with and without intralenticular fungal invasion in the horse. Veterinary ophthalmology. 2009 Sep-Oct; [PubMed PMID: 19751491]
Level 3 (low-level) evidenceKaushik S, Ram J, Dogra MR, Narang S, Brar GS, Gupta A. Traumatic lens abscess with chornic endophthalmitis successfully treated with pars plana lensectomy and vitrectomy. Ophthalmic surgery and lasers. 2001 May-Jun:32(3):239-42 [PubMed PMID: 11371092]
Level 3 (low-level) evidenceMangan MS, Arıcı C, Tuncer İ, Yetik H. Isolated Anterior Lens Capsule Rupture Secondary to Blunt Trauma: Pathophysiology and Treatment. Turkish journal of ophthalmology. 2016 Aug:46(4):197-199. doi: 10.4274/tjo.85547. Epub 2016 Aug 15 [PubMed PMID: 28058159]
Lin YC, Kuo CL, Chen YM. Intralenticular foreign body: A case report and literature review. Taiwan journal of ophthalmology. 2019 Jan-Mar:9(1):53-59. doi: 10.4103/tjo.tjo_88_18. Epub [PubMed PMID: 30993070]
Level 3 (low-level) evidenceBuggage RR,Callanan DG,Shen DF,Chan CC, Propionibacterium acnes endophthalmitis diagnosed by microdissection and PCR. The British journal of ophthalmology. 2003 Sep; [PubMed PMID: 12928300]
Level 3 (low-level) evidenceGrewal SS, Sud RN. Ocular injuries due to caterpillar hairs. Indian journal of ophthalmology. 1976 Oct:24(3):14-7 [PubMed PMID: 1031399]
Level 3 (low-level) evidenceDigre KB, Brennan KC. Shedding light on photophobia. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2012 Mar:32(1):68-81. doi: 10.1097/WNO.0b013e3182474548. Epub [PubMed PMID: 22330853]
Elksnis Ē, Vanags J, Elksne E, Gertners O, Laganovska G. Isolated posterior capsule rupture after blunt eye injury. Clinical case reports. 2021 Apr:9(4):2105-2108. doi: 10.1002/ccr3.3956. Epub 2021 Feb 18 [PubMed PMID: 33936647]
Level 3 (low-level) evidenceHwang HJ,Lee YW,Koh KM,Hwang KY,Kwon YA,Song SW,Kim BY,Kim KY, Lenticular fungal infection caused by Aspergillus in a patient with traumatic corneal laceration: a case report. BMC ophthalmology. 2020 May 1; [PubMed PMID: 32357853]
Level 3 (low-level) evidenceRose-Nussbaumer J, Li Y, Lin P, Suhler E, Asquith M, Rosenbaum JT, Huang D. Aqueous cell differentiation in anterior uveitis using Fourier-domain optical coherence tomography. Investigative ophthalmology & visual science. 2015 Feb 3:56(3):1430-6. doi: 10.1167/iovs.14-15118. Epub 2015 Feb 3 [PubMed PMID: 25650415]
Campbell TD, Gnugnoli DM. Seidel Test. StatPearls. 2024 Jan:(): [PubMed PMID: 31082063]
Cheung CM, Durrani OM, Murray PI. The safety of anterior chamber paracentesis in patients with uveitis. The British journal of ophthalmology. 2004 Apr:88(4):582-3 [PubMed PMID: 15031183]
Level 3 (low-level) evidenceGarg P,Rao GN, Corneal ulcer: diagnosis and management. Community eye health. 1999; [PubMed PMID: 17491983]
Sharma B, Abell RG, Arora T, Antony T, Vajpayee RB. Techniques of anterior capsulotomy in cataract surgery. Indian journal of ophthalmology. 2019 Apr:67(4):450-460. doi: 10.4103/ijo.IJO_1728_18. Epub [PubMed PMID: 30900573]
Salman A, Parmar P, Philip VR, Thomas PA, Jesudasan CA. Traumatic intralenticular abscess: a case series. Clinical & experimental ophthalmology. 2007 Apr:35(3):252-5 [PubMed PMID: 17430512]
Level 3 (low-level) evidencePotop V, Coviltir V, Schmitzer S, Corbu CG, Ionescu CI, Burcel MG, Ciocâlteu A, Dăscălescu D. Ultrasound biomicroscopy as a vital tool in occult phacomorphic glaucoma. Romanian journal of ophthalmology. 2019 Oct-Dec:63(4):311-314 [PubMed PMID: 31915727]
Voss JO,Maier C,Wüster J,Beck-Broichsitter B,Ebker T,Vater J,Dommerich S,Raguse JD,Böning G,Thieme N, Imaging foreign bodies in head and neck trauma: a pictorial review. Insights into imaging. 2021 Feb 15; [PubMed PMID: 33587198]
Novosad BD, Callegan MC. Severe bacterial endophthalmitis: towards improving clinical outcomes. Expert review of ophthalmology. 2010 Oct:5(5):689-698 [PubMed PMID: 21572565]
Level 2 (mid-level) evidenceChatterjee S, Agrawal D. 5% cefuroxime as an alternative to 5% cefazolin in the treatment of Gram-positive bacterial keratitis. Indian journal of ophthalmology. 2018 Jul:66(7):1046-1048. doi: 10.4103/ijo.IJO_329_18. Epub [PubMed PMID: 29941771]
Jaspers CA, Kieft H, Speelberg B, Buiting A, van Marwijk Kooij M, Ruys GJ, Vincent HH, Vermeulen MC, Olink AG, Hoepelman IM. Meropenem versus cefuroxime plus gentamicin for treatment of serious infections in elderly patients. Antimicrobial agents and chemotherapy. 1998 May:42(5):1233-8 [PubMed PMID: 9593156]
Level 1 (high-level) evidenceKemnic TR,Coleman M, Trimethoprim Sulfamethoxazole. StatPearls. 2022 Jan; [PubMed PMID: 30020604]
Noh GM, Nam KY, Lee SU, Lee SJ. Precipitation of Vancomycin and Ceftazidime on Intravitreal Injection in Endophthalmitis Patients. Korean journal of ophthalmology : KJO. 2019 Jun:33(3):296-297. doi: 10.3341/kjo.2018.0080. Epub [PubMed PMID: 31179663]
Dong LK, Krebs DB. An intracameral approach for recalcitrant fungal keratitis. American journal of ophthalmology case reports. 2022 Mar:25():101369. doi: 10.1016/j.ajoc.2022.101369. Epub 2022 Jan 27 [PubMed PMID: 35146213]
Level 3 (low-level) evidenceSharma S, Das S, Virdi A, Fernandes M, Sahu SK, Kumar Koday N, Ali MH, Garg P, Motukupally SR. Re-appraisal of topical 1% voriconazole and 5% natamycin in the treatment of fungal keratitis in a randomised trial. The British journal of ophthalmology. 2015 Sep:99(9):1190-5. doi: 10.1136/bjophthalmol-2014-306485. Epub 2015 Mar 4 [PubMed PMID: 25740805]
Level 1 (high-level) evidenceGreer ND. Voriconazole: the newest triazole antifungal agent. Proceedings (Baylor University. Medical Center). 2003 Apr:16(2):241-8 [PubMed PMID: 16278744]
Alves da Costa Pertuiset PA, Logroño JF. Fusarium Endophthalmitis following Cataract Surgery: Successful Treatment with Intravitreal and Systemic Voriconazole. Case reports in ophthalmological medicine. 2016:2016():4593042. doi: 10.1155/2016/4593042. Epub 2016 Jun 22 [PubMed PMID: 27418989]
Level 3 (low-level) evidenceAlbab N, Oujidi M, Belghamaidi S, Hakam J, Hajji I, Moutaj R, Moutaouakil A. Intrastromal injection of voriconazole as a therapeutic of fungal hypopyon: a case report. The Pan African medical journal. 2020:35():52. doi: 10.11604/pamj.2020.35.52.20225. Epub 2020 Feb 21 [PubMed PMID: 32537057]
Level 3 (low-level) evidenceRamamoorthy S, Cidlowski JA. Corticosteroids: Mechanisms of Action in Health and Disease. Rheumatic diseases clinics of North America. 2016 Feb:42(1):15-31, vii. doi: 10.1016/j.rdc.2015.08.002. Epub [PubMed PMID: 26611548]
Babu K, Mahendradas P. Medical management of uveitis - current trends. Indian journal of ophthalmology. 2013 Jun:61(6):277-83. doi: 10.4103/0301-4738.114099. Epub [PubMed PMID: 23803479]
Agrawal RV, Murthy S, Sangwan V, Biswas J. Current approach in diagnosis and management of anterior uveitis. Indian journal of ophthalmology. 2010 Jan-Feb:58(1):11-9. doi: 10.4103/0301-4738.58468. Epub [PubMed PMID: 20029142]
Kaur K, Gurnani B. Cycloplegic and Noncycloplegic Refraction. StatPearls. 2024 Jan:(): [PubMed PMID: 35593830]
Noecker RJ. The management of glaucoma and intraocular hypertension: current approaches and recent advances. Therapeutics and clinical risk management. 2006 Jun:2(2):193-206 [PubMed PMID: 18360593]
Level 3 (low-level) evidenceWang Z, Lu Y, Xiao K, Gao Y, He J, Zhang S, Wang G, Zhang M. Bimanual irrigation-aspiration for ectopia lentis and use of a small incision for 4-point scleral-sutured foldable intraocular lens and anterior vitrectomy in patients with Marfan syndrome. Indian journal of ophthalmology. 2019 Oct:67(10):1629-1633. doi: 10.4103/ijo.IJO_250_19. Epub [PubMed PMID: 31546497]
Mohanty P, Prasan VV, Vivekanand U. Conventional extracapsular cataract extraction and its importance in the present day ophthalmic practice. Oman journal of ophthalmology. 2015 Sep-Dec:8(3):175-8. doi: 10.4103/0974-620X.169906. Epub [PubMed PMID: 26903724]
Gurnani B, Kaur K. Manual Small Incision Cataract Surgery. StatPearls. 2024 Jan:(): [PubMed PMID: 35881728]
Gurnani B,Kaur K, Phacoemulsification. StatPearls. 2022 Jan; [PubMed PMID: 35015444]
Astbury N, Wood M, Gajiwala U, Patel R, In the Sewa Rural Team, Chen Y, Benjamin L, Abuh SO. Management of capsular rupture and vitreous loss in cataract surgery. Community eye health. 2008 Mar:21(65):6-8 [PubMed PMID: 18504467]
Salehi A, Razmju H, Beni AN, Beni ZN. Visual outcome of early and late pars plana vitrectomy in patients with dropped nucleus during phacoemulsification. Journal of research in medical sciences : the official journal of Isfahan University of Medical Sciences. 2011 Nov:16(11):1422-9 [PubMed PMID: 22973342]
Rajaraman R, Lalitha P, Raghavan A, Palanisamy M, Prajna NV. Traumatic lenticular abscess: clinical description and outcome. American journal of ophthalmology. 2007 Jul:144(1):144-6 [PubMed PMID: 17601443]
Level 2 (mid-level) evidenceGurnani B,Kaur K, Pythium Keratitis. StatPearls. 2022 Jan; [PubMed PMID: 34424645]
Gurnani B, Kaur K, Agarwal S, Lalgudi VG, Shekhawat NS, Venugopal A, Tripathy K, Srinivasan B, Iyer G, Gubert J. Pythium insidiosum Keratitis: Past, Present, and Future. Ophthalmology and therapy. 2022 Oct:11(5):1629-1653. doi: 10.1007/s40123-022-00542-7. Epub 2022 Jul 5 [PubMed PMID: 35788551]
Gurnani B, Kaur K, Venugopal A, Srinivasan B, Bagga B, Iyer G, Christy J, Prajna L, Vanathi M, Garg P, Narayana S, Agarwal S, Sahu S. Pythium insidiosum keratitis - A review. Indian journal of ophthalmology. 2022 Apr:70(4):1107-1120. doi: 10.4103/ijo.IJO_1534_21. Epub [PubMed PMID: 35325996]
Beyer TL, O'Donnell FE, Goncalves V, Singh R. Role of the posterior capsule in the prevention of postoperative bacterial endophthalmitis: experimental primate studies and clinical implications. The British journal of ophthalmology. 1985 Nov:69(11):841-6 [PubMed PMID: 3877524]
Level 3 (low-level) evidenceLeekha S, Terrell CL, Edson RS. General principles of antimicrobial therapy. Mayo Clinic proceedings. 2011 Feb:86(2):156-67. doi: 10.4065/mcp.2010.0639. Epub [PubMed PMID: 21282489]
Qiu S, Zhao GQ, Lin J, Wang X, Hu LT, Du ZD, Wang Q, Zhu CC. Natamycin in the treatment of fungal keratitis: a systematic review and Meta-analysis. International journal of ophthalmology. 2015:8(3):597-602. doi: 10.3980/j.issn.2222-3959.2015.03.29. Epub 2015 Jun 18 [PubMed PMID: 26086015]
Level 2 (mid-level) evidenceSmith LF, Bainbridge J, Burns J, Stevens J, Taylor P, Murdoch I. Evaluation of telemedicine for slit lamp examination of the eye following cataract surgery. The British journal of ophthalmology. 2003 Apr:87(4):502-3 [PubMed PMID: 12642321]
Sanii Y,Torkamandi H,Gholami K,Hadavand N,Javadi M, Role of pharmacist counseling in pharmacotherapy quality improvement. Journal of research in pharmacy practice. 2016 Apr-Jun; [PubMed PMID: 27162808]
Level 2 (mid-level) evidence