Introduction
The premalignant oral disorder is a blanket term for a variety of pathologies that can arise in the oral cavity. Early recognition and prompt management are key to optimal outcomes. However, there remains a significant knowledge gap in this area among medical practitioners.[1] A recent systematic review revealed that less than half of medical practitioners were aware of common risk factors of premalignant oral lesions or oral carcinoma; further, a low level of awareness was noted among most medical practitioners of common premalignant oral cavity lesions. Thus, there remains a significant need to understand and recognize the presentation, pathophysiology, and management of these conditions.
The oral cavity is an anatomical site defined by an area that includes the lips, gums, buccal mucosa, gingiva/alveolar ridge, hard palate, the floor of the mouth, and oral tongue (anterior 2/3). The vestibule is comprised of the buccal and labial aspects of dentition, as well as the mucosa of the alveolus and wet border of the lip.[2] Stratified squamous epithelium lines the majority of the oral cavity, and aberrancy in this epithelium is often what gives rise to premalignant oral lesions.
The most commonly described premalignant oral lesions are leukoplakia, erythroplakia, lichen planus, and submucous fibrosis.[3][4][5][6] This review will describe the etiology, pathophysiology, pertinent history, and exam findings, as well as management options for these oral cavity malignant precursors.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The most commonly described etiologies of premalignant oral lesions are cigarette smoking, tobacco, and alcohol exposure.[7][8] Betel nut chewing has also been associated with the development of oral leukoplakia.[9] Human papillomavirus (HPV) has emerged as a risk factor: a recent meta-analysis of 52 studies revealed a pooled HPV DNA prevalence of 22.5% in oral premalignant disorders.[10] The authors also noted that HPV16 was the predominant genotype, which is also the most common serotype found in oropharyngeal cancer.[11]
Epidemiology
Oral premalignant lesions occur in roughly between 1.5% and 4.5% of the world's population and disproportionately affect men compared to women.[12][13] The highest rates were found in Asian, South American, and Caribbean populations, as geographical variance exists due to differing rates of tobacco and alcohol consumption. Oral premalignant lesions account for 17% to 35% of all new cases of oral cavity cancer and undergo malignant transformation between 0.7% and 2.9% annually.[14][15]
Pathophysiology
The oral cavity is lined with stratified squamous epithelium, which is exquisitely sensitive to carcinogenic insult. Exposure to tobacco, alcohol, betel nut, or human papillomavirus can result in a cellular microenvironment that results in the formation of dysplastic or hyperkeratotic epithelium. This manifests clinically as oral leukoplakia, erythroplakia, or lichen planus. These entities have varying rates of progression to carcinoma, though dysplastic epithelium can be present in any of these pathologies, highlighting the need for histopathological evaluation.[16] The pre-malignant nature of oral lichen planus remains controversial versus oral lichenoid lesions showing more established pre-malignant potential.[17]
Oral submucous fibrosis is a separate entity that is caused specifically by betel nut use. Chronic betel quid use results in submucosal fibrosis, leading to progressive oral cavity scarring leading to trismus, dysphagia, or odynophagia. Oral submucous fibrosis may present in isolation but can also be found concurrently with leukoplakia or erythroplakia.[18]
Histopathology
Histopathology of oral leukoplakia often reveals hyperkeratosis or parakeratosis with varying degrees of inflammation. Hyperplastic epithelium may be present, in addition to mild, moderate, or severe dysplasia. Carcinoma in situ or frank carcinoma also may be present.[19]
Erythroplakia often has similar features on histological evaluation, including varying degrees of dysplasia; erythroplakia lesions harbor carcinoma more frequently than leukoplakic lesions.[20] Lichen planus can similarly display hyperkeratosis, in addition to lymphocytic infiltration and Civatte bodies.[21] Finally, oral submucous fibrosis exhibits characteristic collagen hyalinization and deposition of fibrotic material in the submucosa and muscularis.[18]
History and Physical
Evaluation of oral lesions requires thoughtful evaluation and close attention to physical exam findings. In assessing a patient with a possible premalignant oral lesion, the clinician must elicit the length of time the lesion has been present, the evolution of the lesion (change in character or size), presence or absence of pain or recent dental trauma, bleeding, associated dysphagia, odynophagia, trismus, or weight loss, as well as the history of smoking or alcohol exposure. Special attention to medical history, including autoimmune disorders or history of solid organ transplant, is vital, as these patients are at higher risk of developing oral cavity carcinoma.[22][23]
Certain viral illnesses can predispose patients to premalignant oral lesions, including human immunodeficiency virus or Hepatitis C. Hepatitis C is often comorbid with oral lichen planus.[24] On physical exam, it is important to characterize size, shape, description, color, firmness, and location of the lesion, along with the presence of cervical or parotid lymphadenopathy if it is present. Leukoplakia will present as a white patch or plaque in the oral cavity, which cannot be wiped off, whereas erythroplakia may present as a firm red patch or plaque; both are usually non-tender lesions. The lesion can be diffuse or well-circumscribed and may involve the wet border of the lip, floor of the mouth, oral tongue, or buccal mucosa.
On the other hand, oral submucous fibrosis usually involves the oral tongue and may include portions of the oropharynx. There is often a pale discoloration of the mucosa with a mottled appearance and may result in trismus in advanced cases. Finally, oral lichen planus may present as an ulcerative, tender lesion with a fine reticular appearance, often of the oral tongue or buccal mucosa.[22]
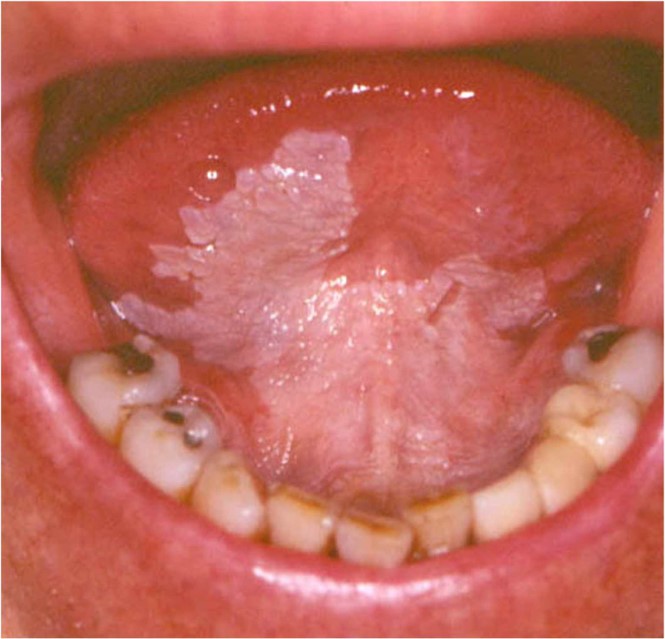
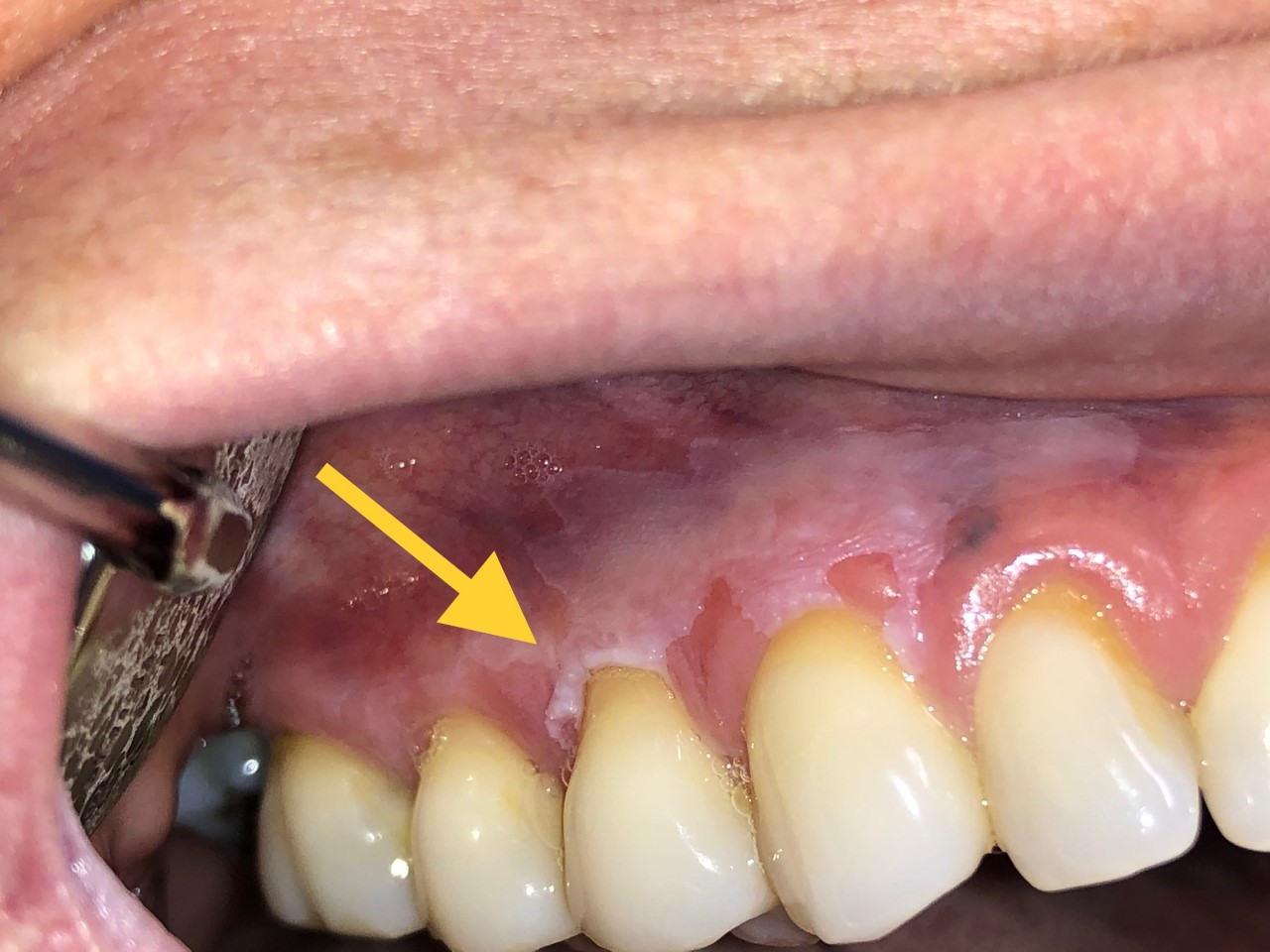
Figures 1-3 display a variety of leukoplakic lesions of the oral cavity.
Evaluation
Evaluation of premalignant oral lesions consists of both physical exam and biopsy. As noted above, a careful bimanual exam with appropriate illumination is paramount. Tissue sampling is warranted to rule out frank malignancy in most cases. If the lesion is diffuse or involving multiple subsites, several samples from different sites should be obtained. If moderate or severe dysplasia is present on histopathology, excisional biopsy with appropriate margins should be strongly considered to formally exclude malignancy.[25]
Contrasted computed tomography from the skull base to the clavicle is recommended if malignancy is suspected or if cervical adenopathy is present. Imaging allows for further characterization of the lesion as well as in staging in the case of malignancy.
Treatment / Management
Management of premalignant oral lesions is focused mainly on the prevention of oral cavity carcinoma. Based upon the histopathology of the lesion and patient preference, cessation of risk factors including alcohol, tobacco, and betel nut, along with close observation, are a reasonable option in patients with low-risk lesions. However, in patients with high-risk lesions (with moderate or severe dysplasia on histopathology or high-risk sites such as the lateral border of tongue or floor of mouth), excisional biopsy is the management of choice. Several methods are available, including laser ablation or formal excision.
The obvious limitation of laser ablation is that formal histopathological evaluation of the entire lesion is not feasible due to the destructive nature of laser ablation. A recent study found that when compared to simple biopsies, whole lesion excision revealed a 7% rate of occult carcinoma and a 79% variation in the degree of dysplasia present in the initial biopsy.[26] (B2)
Therefore, excisional biopsy is the gold standard of treatment if clinical suspicion remains. The only randomized trial evaluating surgical excision vs. smoking cessation and close observation in a total of 260 patients with nondysplastic oral leukoplakia revealed a nonsignificant difference in the development of carcinoma between the two arms, suggesting that watchful waiting may be feasible in otherwise low-risk patients.[27] (A1)
Several nonsurgical treatments, including non-steroidal inflammatory drugs and retinoids, may be effective, yet high-level data supporting these treatments is lacking.[28] Lichen planus, in particular, may be managed with topical corticosteroids with varying degrees of success.[24](A1)
Differential Diagnosis
Several other entities may mimic oral premalignant lesions, including squamous cell carcinoma, oral candidiasis, oral hairy leukoplakia, oral mucositis or graft versus host disease, autoimmune lesions (i.e., discoid lupus), or Kawasaki disease. Histological evaluation remains the gold standard for differentiating these pathologies.
Prognosis
Prognosis of oral premalignant disorders centers mainly upon the clinical presentation of the lesion and the degree of dysplasia present on histopathology. Close follow-up is recommended in these patients, especially in those with risk factors such as tobacco use, immunosuppression, or severe dysplasia, as a recent study showed that up to half of treated patients develop recurrence or new lesions and up to a fifth can develop invasive carcinoma.[29] In some practices, quarterly follow-up is performed in high-risk patients, and at least biannual follow-up is recommended in low-risk patients.
Complications
The most feared complication of oral premalignant disorders is progression to carcinoma. A recent meta-analysis revealed that the rate of malignant transformation of all oral premalignant disorders combined was around 7.9%. In contrast, lichen planus alone is around 1.4%, leukoplakia 9.5%, oral submucous fibrosis 5.2%, and erythroplakia 33.1%.[30] Close follow-up and possible surgical intervention are thus essential for the prevention and early detection of oral carcinoma.
Deterrence and Patient Education
Patient education and deterrence of tobacco, alcohol, and betel nut exposure are essential to preventing further epithelial toxicity and oral premalignant disorders.
Pearls and Other Issues
To avoid the development of oral cavity carcinoma, histological evaluation is essential. Surgical excision is recommended for high-risk lesions. Low-risk lesions managed with observation must be closely followed and physical exam findings documented appropriately to assess interval changes.[25] Photo documentation can aid in this endeavor as well.
Enhancing Healthcare Team Outcomes
Due to the risk of malignant transformation of oral premalignant disorders, prompt diagnosis is critical. Management of oral premalignant disorders is complex and requires an interprofessional team approach, including the expertise of pathologists, surgical oncologists, and radiologists, in addition to the auxiliary staff. Nurses and pharmacists may also play a role in some cases. In patients treated non surgically, pharmacists play a vital role in managing medications and ensuring no adverse effects occur. An interprofessional team-based approach is paramount to patient outcomes and the prevention of oral cavity carcinoma. [Levle 5]
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Papadiochou S, Papadiochos I, Perisanidis C, Papadogeorgakis N. Medical practitioners' educational competence about oral and oropharyngeal carcinoma: a systematic review and meta-analysis. The British journal of oral & maxillofacial surgery. 2020 Jan:58(1):3-24. doi: 10.1016/j.bjoms.2019.08.007. Epub 2019 Nov 27 [PubMed PMID: 31785865]
Level 1 (high-level) evidenceTonge CH. Oral anatomy--progress of a discipline. British dental journal. 1981 Jul 7:151(1):3-5 [PubMed PMID: 7018532]
Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. Journal of oral pathology & medicine : official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology. 2007 Nov:36(10):575-80 [PubMed PMID: 17944749]
Maymone MBC, Greer RO, Kesecker J, Sahitya PC, Burdine LK, Cheng AD, Maymone AC, Vashi NA. Premalignant and malignant oral mucosal lesions: Clinical and pathological findings. Journal of the American Academy of Dermatology. 2019 Jul:81(1):59-71. doi: 10.1016/j.jaad.2018.09.060. Epub 2018 Nov 14 [PubMed PMID: 30447325]
Mccormick NJ, Thomson PJ, Carrozzo M. The Clinical Presentation of Oral Potentially Malignant Disorders. Primary dental journal. 2016 Feb 1:5(1):52-63 [PubMed PMID: 29029654]
Wetzel SL, Wollenberg J. Oral Potentially Malignant Disorders. Dental clinics of North America. 2020 Jan:64(1):25-37. doi: 10.1016/j.cden.2019.08.004. Epub [PubMed PMID: 31735231]
Kusiak A, Maj A, Cichońska D, Kochańska B, Cydejko A, Świetlik D. The Analysis of the Frequency of Leukoplakia in Reference of Tobacco Smoking among Northern Polish Population. International journal of environmental research and public health. 2020 Sep 22:17(18):. doi: 10.3390/ijerph17186919. Epub 2020 Sep 22 [PubMed PMID: 32971842]
Grady D, Greene J, Daniels TE, Ernster VL, Robertson PB, Hauck W, Greenspan D, Greenspan J, Silverman S Jr. Oral mucosal lesions found in smokeless tobacco users. Journal of the American Dental Association (1939). 1990 Jul:121(1):117-23 [PubMed PMID: 2370378]
Thomas SJ, Harris R, Ness AR, Taulo J, Maclennan R, Howes N, Bain CJ. Betel quid not containing tobacco and oral leukoplakia: a report on a cross-sectional study in Papua New Guinea and a meta-analysis of current evidence. International journal of cancer. 2008 Oct 15:123(8):1871-6. doi: 10.1002/ijc.23739. Epub [PubMed PMID: 18688850]
Level 2 (mid-level) evidencede la Cour CD, Sperling CD, Belmonte F, Syrjänen S, Kjaer SK. Human papillomavirus prevalence in oral potentially malignant disorders: Systematic review and meta-analysis. Oral diseases. 2021 Apr:27(3):431-438. doi: 10.1111/odi.13322. Epub 2020 Mar 30 [PubMed PMID: 32144837]
Level 1 (high-level) evidenceKreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2005 Feb:14(2):467-75 [PubMed PMID: 15734974]
Level 1 (high-level) evidenceMello FW, Miguel AFP, Dutra KL, Porporatti AL, Warnakulasuriya S, Guerra ENS, Rivero ERC. Prevalence of oral potentially malignant disorders: A systematic review and meta-analysis. Journal of oral pathology & medicine : official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology. 2018 Aug:47(7):633-640. doi: 10.1111/jop.12726. Epub 2018 Jun 6 [PubMed PMID: 29738071]
Level 1 (high-level) evidencePetti S. Pooled estimate of world leukoplakia prevalence: a systematic review. Oral oncology. 2003 Dec:39(8):770-80 [PubMed PMID: 13679200]
Level 1 (high-level) evidenceSilverman S Jr, Gorsky M, Lozada F. Oral leukoplakia and malignant transformation. A follow-up study of 257 patients. Cancer. 1984 Feb 1:53(3):563-8 [PubMed PMID: 6537892]
van der Waal I, Schepman KP, van der Meij EH, Smeele LE. Oral leukoplakia: a clinicopathological review. Oral oncology. 1997 Sep:33(5):291-301 [PubMed PMID: 9415326]
van der Waal I. Oral leukoplakia, the ongoing discussion on definition and terminology. Medicina oral, patologia oral y cirugia bucal. 2015 Nov 1:20(6):e685-92 [PubMed PMID: 26449439]
van der Meij EH, Mast H, van der Waal I. The possible premalignant character of oral lichen planus and oral lichenoid lesions: a prospective five-year follow-up study of 192 patients. Oral oncology. 2007 Sep:43(8):742-8 [PubMed PMID: 17112770]
Level 2 (mid-level) evidencePassi D, Bhanot P, Kacker D, Chahal D, Atri M, Panwar Y. Oral submucous fibrosis: Newer proposed classification with critical updates in pathogenesis and management strategies. National journal of maxillofacial surgery. 2017 Jul-Dec:8(2):89-94. doi: 10.4103/njms.NJMS_32_17. Epub [PubMed PMID: 29386809]
Farah CS, Woo SB, Zain RB, Sklavounou A, McCullough MJ, Lingen M. Oral cancer and oral potentially malignant disorders. International journal of dentistry. 2014:2014():853479. doi: 10.1155/2014/853479. Epub 2014 May 7 [PubMed PMID: 24891850]
Chuang SL, Wang CP, Chen MK, Su WW, Su CW, Chen SL, Chiu SY, Fann JC, Yen AM. Malignant transformation to oral cancer by subtype of oral potentially malignant disorder: A prospective cohort study of Taiwanese nationwide oral cancer screening program. Oral oncology. 2018 Dec:87():58-63. doi: 10.1016/j.oraloncology.2018.10.021. Epub 2018 Oct 24 [PubMed PMID: 30527244]
Cheng YS, Gould A, Kurago Z, Fantasia J, Muller S. Diagnosis of oral lichen planus: a position paper of the American Academy of Oral and Maxillofacial Pathology. Oral surgery, oral medicine, oral pathology and oral radiology. 2016 Sep:122(3):332-54. doi: 10.1016/j.oooo.2016.05.004. Epub 2016 Jul 9 [PubMed PMID: 27401683]
Katsanos KH, Roda G, Brygo A, Delaporte E, Colombel JF. Oral Cancer and Oral Precancerous Lesions in Inflammatory Bowel Diseases: A Systematic Review. Journal of Crohn's & colitis. 2015 Nov:9(11):1043-52. doi: 10.1093/ecco-jcc/jjv122. Epub 2015 Jul 10 [PubMed PMID: 26163301]
Level 1 (high-level) evidenceKoff JL, Waller EK. Improving cancer-specific outcomes in solid organ transplant recipients: Where to begin? Cancer. 2019 Mar 15:125(6):838-842. doi: 10.1002/cncr.31963. Epub 2019 Jan 9 [PubMed PMID: 30624770]
Lavanya N, Jayanthi P, Rao UK, Ranganathan K. Oral lichen planus: An update on pathogenesis and treatment. Journal of oral and maxillofacial pathology : JOMFP. 2011 May:15(2):127-32. doi: 10.4103/0973-029X.84474. Epub [PubMed PMID: 22529568]
Villa A, Woo SB. Leukoplakia-A Diagnostic and Management Algorithm. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2017 Apr:75(4):723-734. doi: 10.1016/j.joms.2016.10.012. Epub 2016 Oct 26 [PubMed PMID: 27865803]
Holmstrup P, Vedtofte P, Reibel J, Stoltze K. Oral premalignant lesions: is a biopsy reliable? Journal of oral pathology & medicine : official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology. 2007 May:36(5):262-6 [PubMed PMID: 17448135]
Level 2 (mid-level) evidenceArduino PG, Lodi G, Cabras M, Macciotta A, Gambino A, Conrotto D, Karimi D, Haddad GE, Carbone M, Broccoletti R. A Randomized Controlled Trial on Efficacy of Surgical Excision of Nondysplastic Leukoplakia to Prevent Oral Cancer. Cancer prevention research (Philadelphia, Pa.). 2021 Feb:14(2):275-284. doi: 10.1158/1940-6207.CAPR-20-0234. Epub 2020 Sep 21 [PubMed PMID: 32958584]
Level 1 (high-level) evidenceLodi G, Franchini R, Warnakulasuriya S, Varoni EM, Sardella A, Kerr AR, Carrassi A, MacDonald LC, Worthington HV. Interventions for treating oral leukoplakia to prevent oral cancer. The Cochrane database of systematic reviews. 2016 Jul 29:7(7):CD001829. doi: 10.1002/14651858.CD001829.pub4. Epub 2016 Jul 29 [PubMed PMID: 27471845]
Level 1 (high-level) evidenceLodi G, Porter S. Management of potentially malignant disorders: evidence and critique. Journal of oral pathology & medicine : official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology. 2008 Feb:37(2):63-9. doi: 10.1111/j.1600-0714.2007.00575.x. Epub [PubMed PMID: 18197849]
Iocca O, Sollecito TP, Alawi F, Weinstein GS, Newman JG, De Virgilio A, Di Maio P, Spriano G, Pardiñas López S, Shanti RM. Potentially malignant disorders of the oral cavity and oral dysplasia: A systematic review and meta-analysis of malignant transformation rate by subtype. Head & neck. 2020 Mar:42(3):539-555. doi: 10.1002/hed.26006. Epub 2019 Dec 5 [PubMed PMID: 31803979]
Level 1 (high-level) evidence