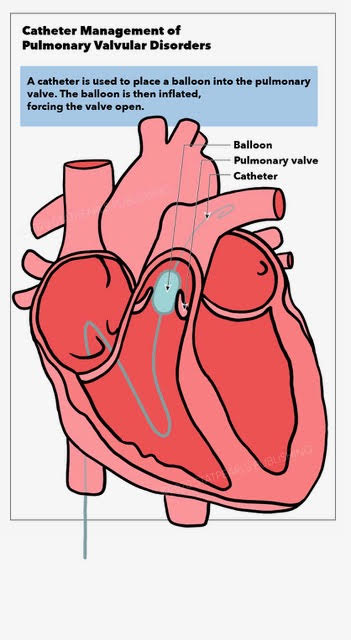
Catheter Management Pulmonary Valvular Disorders
Catheter Management Pulmonary Valvular Disorders
Introduction
Due to advances in several medical subspecialties such as pediatric cardiology and pediatric cardiac surgery, the prevalence of congenital heart disease has increased to 1 in 150 in adulthood, in which about half have undergone surgery in childhood. A significant proportion of patients will need re-intervention in adulthood.[1][2] The right ventricular outflow tract (RVOT) is affected in about 20% of newborns with congenital heart disease, including defects such as tetralogy of Fallot (ToF), truncus arteriosus (TA), pulmonary atresia, etc. Palliation of these defects necessitates various reconstruction techniques with bio-prosthetic valves, trans-annular patches, and conduits between right ventricle (RV) and pulmonary artery (PA).[3] These conduits are usually required when there is an associated anomalous left anterior descending artery (LAD) from the right coronary artery (RCA) crossing the RVOT, thereby precluding a transannular patch repair. While these conduits can restore normal pulmonary valve function, there are subsequent morbidities that can develop, such as conduit calcifications, intimal proliferation, and somatic growth, which therefore make the durability of these conduits limited, and ultimately requiring re-intervention.[4]
The etiology of conduit dysfunction over time is multifactorial and can depend on the patient's age, the defect, tissue type, intervention type, and the material employed. Furthermore, homograft valve deterioration can cause significant RVOT dysfunction, pulmonary regurgitation (PR), and pulmonary stenosis (PS), with about half of the patients requiring re-intervention.[5][6] Additionally, surgical reoperation can have significant morbidity and even mortality due to chest adhesions, cardiac ischemia, heart failure, and multi-organ dysfunction.[7][8][9][10][11][12] Earlier surgical interventions for TOF included the transannular patch procedure with consequences such as pulmonary insufficiency, dilation of tricuspid annulus resulting in tricuspid regurgitation (TR), right ventricular dilation, and atrial and ventricular arrhythmias as a potential etiology of sudden cardiac death (SCD). Transcatheter intervention with balloon angioplasty and stent implantation was a remarkable advancement but still resulted in significant pulmonary regurgitation.[13][14] Transcatheter pulmonary valve implantation (TPVI), which is a common intervention in adult patients with congenital heart disease patients today, has been introduced as a much less invasive approach, allowing earlier restoration of pulmonary valve function before the onset of irreversible remodeling and dysfunction, and potentially fewer lifetime surgical interventions.[15][16]
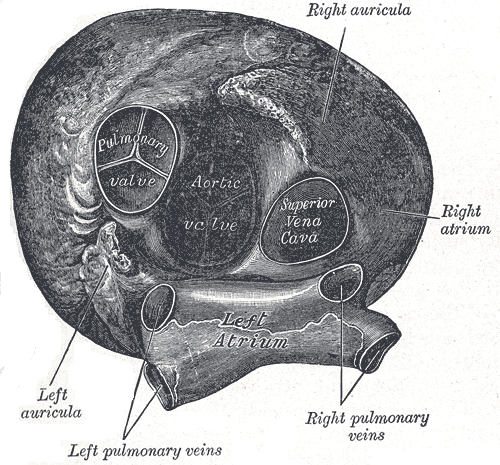
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The optimal anatomy for TPVI is a uniform diameter from the RVOT to the bifurcation of PA with adequate length of main PA to avoid stenting into the bifurcation. TPVI recommendations are currently limited to the dysfunctional RVOT conduits 16 mm in diameter or greater. Occasionally, off-label use of these valves is applied in patients with native or post-TAP repair, or those with less than 16 mm conduits.[17]
Indications
Optimizing the timing for RVOT intervention remains challenging. Standard TPVI criteria are currently similar to those used for surgical pulmonary valve replacement (PVR). The criteria focus on RV volumetric data, RV systolic function, significant TR, significant RVOT obstruction, arrhythmias, QRS interval, and potentially other residual intracardiac defects. TPVI is generally indicated with one of the following criteria in asymptomatic patients with moderate to severe PR:
(1) Significant RV dilation: right ventricular end-diastolic volume index (RVEDVI) > 150 ml/m2, or right ventricular end-systolic volume index (RVESVI) > 80 ml/m2
(2) RV systolic dysfunction: RV ejection fraction (RVEF) < 45%
(3) Persistent atrial or ventricular arrhythmias
(4) RVOT obstruction: RV systolic pressure (RVSP) > 2/3 systemic or > 80 mm Hg
(5) Progressive TR
(6) Symptomatic patients with moderate to severe PR and significant pulmonary stenosis with RVSP > 60 mm Hg.[18]
Class IIa recommendation (Level of evidence: B) for TPVI was assigned by the American Heart Association, American Academy of Pediatrics and Society of Cardiovascular Angiography and Interventions for patients with moderate to severe PR or PS with an RV to PA conduit with or without symptoms.[19]
The presence of symptomatic severe PR and/or PS constitutes a class I indication.
The guidelines recommended by various societies depend on the following risk factors to recommend the intervention of pulmonary valve: (1) age at initial repair, (2) electrophysiological markers, and (3) hemodynamic consequences related to severe PR.[18][20][21][22] QRS interval duration with the predictive value for long-term arrhythmias and risk of SCD is another factor to be considered in the assessment of the need for intervention. A detailed evaluation of RVOT morphology must be carried out to assess TPVI feasibility when the clinical criteria are met.
Contraindications
Active infection and patients with occluded central veins are considered absolute contraindications for TPVI. It is also important to evaluate all potential patients for unfavorable coronary anatomy that could result in coronary compression with valve placement, as coronary compression with valve dilation is an absolute contraindication. At this time, an RVOT diameter larger than the largest valve is considered a contraindication, as this would not allow secure valve placement. Recurrent infective endocarditis (IE) and active intravenous drug abuse are also considered higher long term risk for infection and are often considered contraindications.[18][22]
Equipment
A balloon-expandable valve is the first transcatheter valve approved for use in humans. Bonhoeffer et al. published the first TPVI experience in humans after prior testing in animal models.[13][23] TPVI was subsequently shown to be less invasive, with a lower risk of bleeding and infection compared to surgery, and avoided the risk associated with cardiopulmonary bypass.[24] There are currently three commercially available transcatheter valve systems to treat RVOT dysfunction, although there are only two that are approved for use in the United States. The first-generation balloon-expandable stented prosthesis is offered in two versions, 20 mm and 22 mm, ideal for 16 mm to 24 mm RVOT dimensions.[25] With a closed-cell design, a pulmonary valve conduit made from a valved segment of the bovine jugular vein is sutured within a bare metal platinum iridium stent.[26] The unexpanded stent measures 34 mm in length and shortens to 28 mm and 24 mm when expanded to 18 mm and 22 mm, respectively.[27] The balloon-expandable valve accounts for the majority of transcatheter pulmonary valves implanted, as it was the first commercially available transcatheter valve type. In patients with a large RVOT diameter, but with suitable branch PAs diameters, bilateral valve implantation in-branch PAs has been developed as an innovative approach, though much less commonly used.[28]
More recently, a second-generation balloon-expandable valve commonly used for aortic valve intervention was approved for use in the pulmonary position in 2016. The larger range of sizes (20 mm, 23 mm, 26 mm, and 29 mm) makes this valve potentially suitable for placement in conduits or large RVOTs (> 22 mm). This device consists of a tri-leaflet valve constructed from bovine pericardial tissue and hand-sutured onto a rigid chromium-cobalt. These valves enable the placement of large-diameter transcatheter valves in large conduits and native RVOTs. The length of the stent frame ranges from 14.3 mm and 19.1 mm for 23 and 29 mm valves, respectively, after implantation to suit RVOT dimensions from 20 to 29 mm.[26] The valve may provide some potential advantages over the first-generation valve. The unique valve alignment system allows its use with smaller sheaths. Furthermore, as mentioned above, the valve is available in a larger diameter, thus expanding the potential candidates to include conduits and RVOTs as large as 29 mm. Finally, the rigid stent frame has a potentially lower risk for stent fracture, though this is speculative. With a proximal sealing cuff, the third generation newer balloon-expandable valve is designed to prevent paravalvular leak, although this is not yet approved for pulmonary use with clinical trials in the United States pending. However, the second-generation valve has been approved by the FDA for the treatment of RV-PA conduit dysfunction and valve-in-valve indications in the pulmonic position.
Other Equipment
Stiff wires are used for extra support to deliver the valve to the RVOT, especially in patients with complex anatomies and concomitant pulmonary valve stenosis. A standard pigtail catheter is used to perform angiograms of PAs for good visualization. Medium pressure or high-pressure balloons are used to estimate the RVOT size, assess for coronary artery compression, pre-dilation of RVOT/conduit, and post-dilation of the valve prosthesis. Large sheaths are used for vascular access and for introducing delivery systems to the RVOT. Covered stents are occasionally used to provide a landing zone for the deployment of the prosthetic valve. They reduce the risk of conduit disruption if significant dilation is required due to severe stenosis. In select cases, non-covered stents are used to provide an adequate landing zone. Suture mediated vascular closure devices are routinely deployed before insertion of large sheaths to help optimize hemostasis post-procedure.[26]
Personnel
A cardiac team with interventional cardiologists, cardiac surgeons, non-invasive cardiologists, and cardiac anesthesiologists are crucial to ensure the best potential outcome of this complex procedure. This team should be experienced in treating RVOT interventions. In addition, extracorporeal membrane oxygenation (ECMO) facilities should be considered in the event of significant instability or deterioration, although the need for ECMO support with this procedure is quite rare. Pediatric or interventional cardiologists with expertise in cardiac magnetic resonance imaging (CMR) and echocardiography are extremely helpful for pre-procedure assessment and planning. Nurses need to be available for patient care pre- and post-procedure, including assessing vitals, baseline laboratory tests, confirming the patient’s ABO-Rh blood group, determining baseline renal function, and maintaining hydration. Cardiac catheterization nurses need to ensure the availability of blood in case of conduit tear and/or PA bleeding or perforation. Post-procedure, frequent monitoring of the site of the catheterization, and assessing patients for complications is required.
Preparation
A detailed review of the patient’s history, with a thorough understanding of the cardiac anatomy, as well as specific attention to the details of previous surgical interventions (i.e., type of RVOT reconstruction, size of conduit, type of conduit, intra-operative concerns or challenges, etc.), are crucial. Review of other available diagnostic studies such as previous hemodynamic evaluation, echocardiography, EKGs, stress tests, cross-sectional imaging with either cardiac magnetic resonance imaging (CMR), or computed tomography (CT).[29][30] Specific attention to details such as biventricular function, RVOT morphology, degree of RVOT stenosis and/or regurgitation (spectral Doppler evaluation), and TR need to be evaluated with echocardiography.[31][32][33] It also helps to consider the potential routes vascular access that may be necessary (i.e., femoral vein, internal jugular vein, hybrid approach) and ensure patency of these vessels.
The preferred approach may depend on several factors such as RVOT morphology, compliance and distensibility of the RVOT, and the coronary artery anatomy. CT or MRI cross-sectional imaging with 3D reconstruction can be very helpful to carefully assess the RVOT morphology, conduit type, and degree of calcification.[25][34] The most challenging morphology for transcatheter intervention is a pyramidal shape that is narrow distally and wide proximally, whereas patients with homograft or conduit in place are more suitable conventionally.[35][36][37][38] Another significant determinant for the suitability is the compliance and distensibility of the RVOT. CMR can identify pulsatility, which normally cannot be determined by a CT scan, while balloon testing can more optimally assess RVOT distensibility. In the current era, TPVI’s applicability has been extended to include the native RVOT after publications about the safety and efficacy of TPVI in the same subset of patients.[35][37][38]
Technique or Treatment
General anesthesia or deep sedation is usually employed for the procedure with on-site surgical support.[39] Various vascular access sites can be used, including femoral, jugular, and subclavian veins. Femoral access is the most common, although the jugular approach may allow a more desirable anatomical curvature for delivery of the valve with certain anatomic arrangements, and may provide a larger vessel in smaller patients in whom femoral access may be prohibitive. Prior to the valve implantation, heparin is administered to keep the activated coagulation time (ACT) greater than 250 seconds, and prophylactic antibiotics are typically given prior to placement of any stents or hardware. A right heart catheterization is performed in standard fashion with pressure measurements throughout the entire right heart. When performing the right heart assessment, it is essential to use a balloon-tipped catheter as the catheter crosses the largest effective orifice of the tricuspid valve (TV) with the help of an inflated balloon. This will help prevent the catheter from traversing small spaces within the tricuspid valve chordae or RV trabeculations that could subsequently result in difficulty in passing larger sheaths and/or damage to the tricuspid.
Angiograms are typically performed in the main pulmonary artery and RV in two projections, although in patients with severe pulmonary regurgitation, a single PA angiogram may be sufficient. Very often, the AP projection is optimized with cranial angulation (20 to 30 degrees) to best profile the RVOT/conduit to most accurately determine the conduit’s length, diameter, and morphology. Typically a straight lateral projection with the lateral camera nicely defines the conduit and the proximity to the sternum, which may help predict how and where the conduit will dilate during balloon testing. Aortic root injection, and often selective coronary angiography, is also performed to assess the proximity of the coronary arteries to the conduit, as will be addressed below. It is helpful when performing the angiograms to leave a catheter and/or wire out the RVOT to identify the exact location of the conduit to the coronaries.
After determining whether reasonable clinical and/or hemodynamic criteria are present for intervention, it is important to consider how to best prepare the conduit for valve placement. For patients with significant conduit stenosis, this will almost certainly require dilation of the conduit and potentially “pre-stenting” of the conduit. The most common contemporary practice is to fully dilate the RVOT conduit as much as possible prior to placing a valve to reduce the risk of the stent and/or valve fracture, particularly in patients with severe stenosis and/or calcification. In patients without significant stenosis, or in patients with a rigid bioprosthetic valve that are unlikely to dilate, this may not be necessary. Nonetheless, the presence of a bare-metal stent may provide a nice and easily identifiable landing zone for subsequent valve placement and should always be considered.
Before proceeding with stent implantation for pre-stenting, there are several very important steps that are necessary to reduce the likelihood of significant complications. Firstly, in patients were severe stenosis and/or severe calcification, it is important to perform serial dilations of the conduit with multiple balloons rather than immediate and rapid restoration of the conduit to its original diameter. This is typically done in 2 mm increments up to the original diameter, and in some cases, just slightly larger than the original conduit diameter. This is felt to reduce the risk of conduit rupture and will allow for assessment of and intervention on any conduit tears that may result. As is certainly important during valve implantation, balloon dilation requires a secure and stable wire position as distal as possible to allow for the most stable balloon position. Given the more posterior orientation of the left pulmonary artery (LPA) as compared to the right, the LPA often provides a smooth wire course. However, many anatomic variations can exist in patients post repair, and the RPA can be considered if this orients the wire and/or balloon more ideally. The use of “super-stiff” wires is extremely helpful and should be available for this part of the procedure, with the tip placed as far distally in the branch PAs as possible.
Secondly, it is important to assess the coronary artery anatomy once the conduit is dilated to its intended maximal diameter. The incidence of coronary artery compression with conduit dilation has been shown to be about 5% of patients with complex CHD.[40] Furthermore, it is not uncommon to have anatomic variations of coronary artery origin in patients with CHD.[41] Hence, aortography/selective coronary angiography with simultaneous balloon inflation in RVOT is essential to identify coronary artery compression, which would be a contraindication to the procedure.[40][42] Coronary assessment is typically done with either an aortic root injection or selective coronary artery injection of the left coronary artery while the conduit in the RVOT is fully balloon dilated. This will simulate the effect on anatomy and/or flow in the coronary artery post stent placement. Assessment of the coronary arteries pre-and post-dilation is extremely important to ensure that stent placement will not result in coronary compression. If there are concerns about coronary distortion or compression, stent/valve placement may be contraindicated. It is also important to assess for aortic root compression with or without coronary compression during balloon sizing, as this may cause significant aortic valve insufficiency in patients with native RVOT or transannular patch.[43]
Despite these technical concerns, the procedure has been performed successfully in greater than 96% of patients with RVOT dysfunction.[40][42][44] Provided that the conduit can safely be dilated to a reasonable diameter without coronary compression, it is very often practical to proceed with pre-stenting to the intended diameter. Bare metal stents with a strong radial strength are ideal for this purpose. For patients in whom there are significant concerns for severe calcification and/or stenosis and the potential risk of coronary disruption, it is important to have an array of large covered stents available for either rapid deployment or perhaps even elective use prior to dilation. Given the large diameter of the stent, the use of BIB (balloon-in-balloon) balloon is very helpful to allow for uniform expansion of the stent with the ability to optimize the position after inflating the inner balloon, if needed. It is also important to assess the stent during deflation of the balloon, as significant “recoil” of the stent may result in heavily calcified conduits. Consideration additional stents should be given if significant recoil results to help relieve the radial tension on the subsequent valve itself.
Following conduit preparation with pre-stenting, if necessary, it is important to select the type and size of the pulmonary valve for implantation. As described above, the first-generation transcatheter valve system allows for the placement of valves 16 mm to 22 mm in diameter with a valve and delivery system designed for the pulmonary position. The associated delivery system for this valve allows for the preparation of the valve onto an appropriate BIB balloon, which is then housed by an integrated sheath that eliminates the need for additional sheathing or manipulation. The tapered nature of the sheath with a long tapered dilator at the tip allows for relatively easy delivery of the entire delivery system over the wire into the RVOT that protects the valve within the sheath. The second-generation valve is an alternative that allows for larger diameter valves (up to 29 mm) and thus may be ideal for larger conduits and/or outflow tracts. The delivery system is unique in that it allows for valve alignment onto the balloon within the IVC and thus allows for a smaller access sheath. The valve itself is therefore not covered by the sheath, and this may create some challenges in passing this delivery system through the RVOT with the potential for the valve/balloon apparatus to the course along RV trabeculations and/or conduit calcifications or irregularities. More recently, the use of larger introducer sheaths into the MPA has helped alleviate this problem. The second-generation valve is loaded onto a single large diameter balloon, and thus slow, controlled inflation to the intended balloon volume allows for accurate valve positioning.
Following valve placement, right heart hemodynamics are reassessed, as is a pulmonary artery angiogram to evaluate the valve position, valve competence and to assess branch PA flow. Occasionally, post-implantation dilation to further expand the valve or eliminate any residual gradient or perivalvular leak is indicated. Hemostasis can be achieved with several maneuvers (i.e., the figure of eight suture, closure device, or manual pressure), and post-procedure bleeding from the venous access site is rarely problematic, despite the large sheaths. Patients are observed in CCU or telemetry wards overnight, and a 24 hr course intravenous antibiotics is standard. ECG, posteroanterior (PA)/lateral X-ray chest, and transthoracic echocardiogram (TTE) should be performed the following day, with most patients suitable for discharge in 24 hrs. The patient should be discharged home on daily aspirin, and this should be continued indefinitely while the valve remains in place.
Complications
Although uncommon, it is important to be aware of several potential procedural complications in patients with severe RV dysfunction, the combination of pulmonary regurgitation and a stiff wire traversing the tricuspid valve potentially causing tricuspid regurgitation, hypotension, and hemodynamic instability may occur. More significantly, severe hemodynamic compromise may result from valve dislodgment into the PA, causing obstruction of the pulmonary blood flow, coronary compression causing coronary ischemia, and conduit rupture causing major hemorrhage. However, these are fortunately rare. Heavy calcification and the presence of homograft conduits have been identified as risk factors for rupture.[45] In homografts and conduits, pre and post-deployment dilations of the balloon have the potential to cause rupture or a tear. Most cases can be managed successfully with a covered stent, but surgical conduit replacement may be required following rupture.[17][46] Valve migration/embolization remains a potential serious procedural complication, which may require surgical explanation. Fortunately, with adequate conduit assessment and RVOT preparation, this remains rare. Nonetheless, should this occur, valve deployment into a branch pulmonary artery has been proposed as a potential remedy should the valve embolize distally. Furthermore, retrieval with the deployment of the embolized valve into the inferior vena cava (IVC) with subsequent stenting to open the valve leaflets has been also proposed as a potential solution, but this carries a significant risk of injury to TV, RV, and IVC.
Longer-term complications include the risk of stent fracture, which remains the most common reason for re-intervention with the first-generation valve, even despite pre-stenting (5% to 16%). Younger age, higher pre-and procedural RVOT gradient, smaller angiographic conduit diameter, valve position directly under the sternum, stent recoil, or compression after deployment is the risk factors.[46][47] Type I fracture constitutes of one strut disruption without loss of stent integrity. Type II includes stent integrity loss, and type III includes fractures with fragment separation. Type I can be seen in up to 40% of patients; however, it is not usually associated with any adverse effects. Type II and III stent fractures are associated with early conduit restenosis and valve failure and may require surgical replacement or repeat TPVI. Clinically significant stent fracture with the second-generation valve in the pulmonary position has not yet been reported.
More recently, the development of infective endocarditis has emerged as a significant risk, with an incidence of approximately 2.4% per patient-year. Male gender, multiple stents, unprotected dental treatment, previous history of endocarditis, and non-compliance of aspirin constitute the risk factors.[48][49][50][51] Percutaneous pulmonary valve (PPV) endocarditis is characterized by vegetation visualized on the implant or as the new evidence of PPV dysfunction associated with bloodstream infection.[52] A wide spectrum of organisms ranging from coagulase-negative staphylococcus to HACEK organisms can cause TPVI-related endocarditis. Streptococcus viridans and Staphylococcus aureus are the most common causes. Occasionally this can be treated and cleared medically. However, due to the significant dysfunction of the valve post-infection, many patients require surgical replacement of the valve even if the bloodstream is able to be cleared of infection.
Clinical Significance
A decade after its approval in the United States, TPVI has emerged as a safe and effective non-surgical therapeutic modality for RVOT dysfunction that often results in a peak cath gradient less than 35 mm Hg and no more than mild insufficiency, with a complication rate is between 6% and 13%.[44][53][54] Several studies have now demonstrated the clinical efficacy of the procedure, highlighting its potential to reduce the RV pressure, RVOT gradient, and eliminate PR.[33][46][55][56] Percutaneous restoration of pulmonary valve function has also been shown to result in a significant decrease in RV dimensions, improvement in stroke volumes, and improvement NYHA functional classes.[44][57][58][59] Furthermore, patients experience an improvement in exercise capacity and improvement in peak oxygen consumption.[57][60][61][62] Patients were free of valve dysfunction or need for re-intervention in 93.5 ± 2.4% at 1 year.[46] The post-approval study showed freedom from PPV dysfunction to be 96.9%. Thus, multiple studies have demonstrated excellent success rates, hemodynamic results, and low rate of complications rates.
The long-term rate of re-intervention with the first-generation valve remains relatively low, with freedom of re-intervention at 1 year and 5 years are greater than 90% and 76%, respectively, excluding patients with stent fracture.[54] Several risk factors for needing reintervention have been identified: lack of pre-stenting, presence of a homograft, moderate-to-severe tricuspid valve insufficiency pre-procedurally, and post-intervention RVOT gradient greater than 25 mm Hg.[54][63][49] Long term survival for patients receiving a valve is excellent at 98% and 97% at 5 and 7 years, respectively.[54][49] Likewise, the second-generation valve decreases the RVOT gradient, the degree of PR, improves NYHA functional class, decreases RV systolic pressure, RV-PA gradient, and PA systolic pressure.[64][65] Technical success rates for the second-generation valve implantation are equivalent to the first-generation valve about 96%, with similar potential complications (stent migration, ventricular arrhythmia, and conduit rupture) with the technical advantage being its ability to be implanted in larger conduits.[26][66] Freedom from re-intervention at 6 months is about 97%. Thus, both the valve systems have promising results, particularly when care is taken to adequately prepare the existing conduit with pre-stenting for severe conduit stenosis.
Enhancing Healthcare Team Outcomes
Transcatheter pulmonary valve replacement is a safe and effective alternative to surgical valve replacement in patients with native RVOT/surgical RVOT conduit dysfunction with excellent procedural success and low incidence of post-procedural pulmonary valvular regurgitation. Fracture of stent frame is the most common etiology for valve degeneration requiring re-intervention. Current recommendations from professional societies recommend TPVI in symptomatic patients with severe PR/PS (Class 1, CEBM level of evidence 3) and asymptomatic patients with severe PS/PR and evidence of RV dysfunction/RV dilation/recurrent arrhythmias (Class 2a, CEBM level of evidence 3). Future development of valve systems improving valve durability, lowering catheter/valve profile, reducing thrombogenicity, and inflammatory response to valves may further improve outcomes, reduce complications, and expand the patients eligible for TPVI.
The interprofessional team approach in the management of patients with RVOT dysfunction plays a critical role in ensuring optimal outcomes for patients. The interprofessional team should include interventional cardiologists, cardiothoracic surgeons, cardiac imaging experts, cardiac anesthesiologists, nurses, and catheterization laboratory technologists who work together to provide an integrated & holistic approach to pre-procedural planning, intra-procedural support, and post-procedural care to ensure optimal outcomes for patients. Communication shared decision making, and collaboration between health care providers is key for excellent outcomes. Interprofessional care also helps identify early and late complications of TPVI, therefore improve the prognosis of the patients. Advancements in imaging techniques and protocols will provide further insight into the pathophysiology of the RVOT dysfunction to help identify appropriate timing for TPVI for the best clinical outcome and long term prognosis.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Marelli AJ,Mackie AS,Ionescu-Ittu R,Rahme E,Pilote L, Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007 Jan 16; [PubMed PMID: 17210844]
Level 2 (mid-level) evidenceWarnes CA,Liberthson R,Danielson GK,Dore A,Harris L,Hoffman JI,Somerville J,Williams RG,Webb GD, Task force 1: the changing profile of congenital heart disease in adult life. Journal of the American College of Cardiology. 2001 Apr; [PubMed PMID: 11300418]
Level 2 (mid-level) evidenceVerheugt CL,Uiterwaal CS,van der Velde ET,Meijboom FJ,Pieper PG,van Dijk AP,Vliegen HW,Grobbee DE,Mulder BJ, Mortality in adult congenital heart disease. European heart journal. 2010 May; [PubMed PMID: 20207625]
Level 2 (mid-level) evidenceYuan SM,Mishaly D,Shinfeld A,Raanani E, Right ventricular outflow tract reconstruction: valved conduit of choice and clinical outcomes. Journal of cardiovascular medicine (Hagerstown, Md.). 2008 Apr; [PubMed PMID: 18334887]
Level 3 (low-level) evidenceOng K,Boone R,Gao M,Carere R,Webb J,Kiess M,Grewal J, Right ventricle to pulmonary artery conduit reoperations in patients with tetralogy of fallot or pulmonary atresia associated with ventricular septal defect. The American journal of cardiology. 2013 Jun 1; [PubMed PMID: 23481618]
Level 2 (mid-level) evidenceBoethig D,Thies WR,Hecker H,Breymann T, Mid term course after pediatric right ventricular outflow tract reconstruction: a comparison of homografts, porcine xenografts and Contegras. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2005 Jan; [PubMed PMID: 15621472]
Level 3 (low-level) evidenceElahi M,Dhannapuneni R,Firmin R,Hickey M, Direct complications of repeat median sternotomy in adults. Asian cardiovascular [PubMed PMID: 15905341]
Temeck BK,Katz NM,Wallace RB, An approach to reoperative median sternotomy. Journal of cardiac surgery. 1990 Mar; [PubMed PMID: 2133819]
van der Bom T,Zomer AC,Zwinderman AH,Meijboom FJ,Bouma BJ,Mulder BJ, The changing epidemiology of congenital heart disease. Nature reviews. Cardiology. 2011 Jan; [PubMed PMID: 21045784]
Vida VL,Berggren H,Brawn WJ,Daenen W,Di Carlo D,Di Donato R,Lindberg HL,Corno AF,Fragata J,Elliott MJ,Hraska V,Kiraly L,Lacour-Gayet F,Maruszewski B,Rubay J,Sairanen H,Sarris G,Urban A,Van Doorn C,Ziemer G,Stellin G, Risk of surgery for congenital heart disease in the adult: a multicentered European study. The Annals of thoracic surgery. 2007 Jan; [PubMed PMID: 17184653]
Verheugt CL,Uiterwaal CS,Grobbee DE,Mulder BJ, Long-term prognosis of congenital heart defects: a systematic review. International journal of cardiology. 2008 Dec 17; [PubMed PMID: 18687485]
Level 1 (high-level) evidenceKhairy P, Aboulhosn J, Gurvitz MZ, Opotowsky AR, Mongeon FP, Kay J, Valente AM, Earing MG, Lui G, Gersony DR, Cook S, Ting JG, Nickolaus MJ, Webb G, Landzberg MJ, Broberg CS, Alliance for Adult Research in Congenital Cardiology (AARCC). Arrhythmia burden in adults with surgically repaired tetralogy of Fallot: a multi-institutional study. Circulation. 2010 Aug 31:122(9):868-75. doi: 10.1161/CIRCULATIONAHA.109.928481. Epub 2010 Aug 16 [PubMed PMID: 20713900]
Level 2 (mid-level) evidenceBonhoeffer P,Boudjemline Y,Saliba Z,Merckx J,Aggoun Y,Bonnet D,Acar P,Le Bidois J,Sidi D,Kachaner J, Percutaneous replacement of pulmonary valve in a right-ventricle to pulmonary-artery prosthetic conduit with valve dysfunction. Lancet (London, England). 2000 Oct 21; [PubMed PMID: 11052583]
Level 3 (low-level) evidencePeng LF,McElhinney DB,Nugent AW,Powell AJ,Marshall AC,Bacha EA,Lock JE, Endovascular stenting of obstructed right ventricle-to-pulmonary artery conduits: a 15-year experience. Circulation. 2006 Jun 6; [PubMed PMID: 16735676]
Level 2 (mid-level) evidencePutman LM,van Gameren M,Meijboom FJ,de Jong PL,Roos-Hesselink JW,Witsenburg M,Takkenberg JJ,Bogers AJ, Seventeen years of adult congenital heart surgery: a single centre experience. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2009 Jul; [PubMed PMID: 19303791]
Level 2 (mid-level) evidenceCoats L,Tsang V,Khambadkone S,van Doorn C,Cullen S,Deanfield J,de Leval MR,Bonhoeffer P, The potential impact of percutaneous pulmonary valve stent implantation on right ventricular outflow tract re-intervention. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2005 Apr; [PubMed PMID: 15784347]
Level 2 (mid-level) evidenceBerman DP,McElhinney DB,Vincent JA,Hellenbrand WE,Zahn EM, Feasibility and short-term outcomes of percutaneous transcatheter pulmonary valve replacement in small (<30 kg) children with dysfunctional right ventricular outflow tract conduits. Circulation. Cardiovascular interventions. 2014 Apr; [PubMed PMID: 24569596]
Level 2 (mid-level) evidenceBaumgartner H, Bonhoeffer P, De Groot NM, de Haan F, Deanfield JE, Galie N, Gatzoulis MA, Gohlke-Baerwolf C, Kaemmerer H, Kilner P, Meijboom F, Mulder BJ, Oechslin E, Oliver JM, Serraf A, Szatmari A, Thaulow E, Vouhe PR, Walma E, Task Force on the Management of Grown-up Congenital Heart Disease of the European Society of Cardiology (ESC), Association for European Paediatric Cardiology (AEPC), ESC Committee for Practice Guidelines (CPG). ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). European heart journal. 2010 Dec:31(23):2915-57. doi: 10.1093/eurheartj/ehq249. Epub 2010 Aug 27 [PubMed PMID: 20801927]
Level 1 (high-level) evidenceFeltes TF,Bacha E,Beekman RH 3rd,Cheatham JP,Feinstein JA,Gomes AS,Hijazi ZM,Ing FF,de Moor M,Morrow WR,Mullins CE,Taubert KA,Zahn EM, Indications for cardiac catheterization and intervention in pediatric cardiac disease: a scientific statement from the American Heart Association. Circulation. 2011 Jun 7; [PubMed PMID: 21536996]
Geva T. Repaired tetralogy of Fallot: the roles of cardiovascular magnetic resonance in evaluating pathophysiology and for pulmonary valve replacement decision support. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance. 2011 Jan 20:13(1):9. doi: 10.1186/1532-429X-13-9. Epub 2011 Jan 20 [PubMed PMID: 21251297]
Silversides CK,Marelli A,Beauchesne L,Dore A,Kiess M,Salehian O,Bradley T,Colman J,Connelly M,Harris L,Khairy P,Mital S,Niwa K,Oechslin E,Poirier N,Schwerzmann M,Taylor D,Vonder Muhll I,Baumgartner H,Benson L,Celermajer D,Greutmann M,Horlick E,Landzberg M,Meijboom F,Mulder B,Warnes C,Webb G,Therrien J, Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: executive summary. The Canadian journal of cardiology. 2010 Mar; [PubMed PMID: 20352134]
Level 3 (low-level) evidenceWarnes CA,Williams RG,Bashore TM,Child JS,Connolly HM,Dearani JA,Del Nido P,Fasules JW,Graham TP Jr,Hijazi ZM,Hunt SA,King ME,Landzberg MJ,Miner PD,Radford MJ,Walsh EP,Webb GD, ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Journal of the American College of Cardiology. 2008 Dec 2; [PubMed PMID: 19038677]
Level 1 (high-level) evidenceAndersen HR,Knudsen LL,Hasenkam JM, Transluminal implantation of artificial heart valves. Description of a new expandable aortic valve and initial results with implantation by catheter technique in closed chest pigs. European heart journal. 1992 May; [PubMed PMID: 1618213]
Level 3 (low-level) evidenceMulder BJ,de Winter RJ,Wilde AA, Percutaneous pulmonary valve replacement: a new development in the lifetime strategy for patients with congenital heart disease. Netherlands heart journal : monthly journal of the Netherlands Society of Cardiology and the Netherlands Heart Foundation. 2007 Jan; [PubMed PMID: 17612700]
Schievano S,Coats L,Migliavacca F,Norman W,Frigiola A,Deanfield J,Bonhoeffer P,Taylor AM, Variations in right ventricular outflow tract morphology following repair of congenital heart disease: implications for percutaneous pulmonary valve implantation. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance. 2007; [PubMed PMID: 17578725]
Level 2 (mid-level) evidenceKheiwa A,Divanji P,Mahadevan VS, Transcatheter pulmonary valve implantation: will it replace surgical pulmonary valve replacement? Expert review of cardiovascular therapy. 2018 Mar; [PubMed PMID: 29433351]
Khambadkone S, Percutaneous pulmonary valve implantation. Annals of pediatric cardiology. 2012 Jan; [PubMed PMID: 22529604]
Gillespie MJ,Dori Y,Harris MA,Sathanandam S,Glatz AC,Rome JJ, Bilateral branch pulmonary artery melody valve implantation for treatment of complex right ventricular outflow tract dysfunction in a high-risk patient. Circulation. Cardiovascular interventions. 2011 Aug; [PubMed PMID: 21846891]
Level 3 (low-level) evidenceChung R,Taylor AM, Imaging for preintervention planning: transcatheter pulmonary valve therapy. Circulation. Cardiovascular imaging. 2014 Jan; [PubMed PMID: 24449547]
Hascoët S,Acar P,Boudjemline Y, Transcatheter pulmonary valvulation: current indications and available devices. Archives of cardiovascular diseases. 2014 Nov; [PubMed PMID: 25444020]
Boudjemline Y,Sarquella-Brugada G,Kamache I,Patel M,Ladouceur M,Bonnet D,Boughenou FM,Fraisse A,Iserin L, Impact of right ventricular outflow tract size and substrate on outcomes of percutaneous pulmonary valve implantation. Archives of cardiovascular diseases. 2013 Jan; [PubMed PMID: 23374968]
Alsulami G,Patel M,Malekzadeh-Milani S,Bonnet D,Boudjemline Y, Hyperacute flash pulmonary oedema after transcatheter pulmonary valve implantation: The melody of an overwhelmed left ventricle. Archives of cardiovascular diseases. 2014 Apr; [PubMed PMID: 24793996]
Level 3 (low-level) evidenceKhambadkone S,Coats L,Taylor A,Boudjemline Y,Derrick G,Tsang V,Cooper J,Muthurangu V,Hegde SR,Razavi RS,Pellerin D,Deanfield J,Bonhoeffer P, Percutaneous pulmonary valve implantation in humans: results in 59 consecutive patients. Circulation. 2005 Aug 23; [PubMed PMID: 16103239]
Schievano S,Petrini L,Migliavacca F,Coats L,Nordmeyer J,Lurz P,Khambadkone S,Taylor AM,Dubini G,Bonhoeffer P, Finite element analysis of stent deployment: understanding stent fracture in percutaneous pulmonary valve implantation. Journal of interventional cardiology. 2007 Dec; [PubMed PMID: 18042059]
Level 3 (low-level) evidenceGillespie MJ,Rome JJ,Levi DS,Williams RJ,Rhodes JF,Cheatham JP,Hellenbrand WE,Jones TK,Vincent JA,Zahn EM,McElhinney DB, Melody valve implant within failed bioprosthetic valves in the pulmonary position: a multicenter experience. Circulation. Cardiovascular interventions. 2012 Dec; [PubMed PMID: 23212395]
Level 2 (mid-level) evidenceBoshoff DE,Cools BL,Heying R,Troost E,Kefer J,Budts W,Gewillig M, Off-label use of percutaneous pulmonary valved stents in the right ventricular outflow tract: time to rewrite the label? Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 22887796]
Level 2 (mid-level) evidenceMeadows JJ,Moore PM,Berman DP,Cheatham JP,Cheatham SL,Porras D,Gillespie MJ,Rome JJ,Zahn EM,McElhinney DB, Use and performance of the Melody Transcatheter Pulmonary Valve in native and postsurgical, nonconduit right ventricular outflow tracts. Circulation. Cardiovascular interventions. 2014 Jun; [PubMed PMID: 24867892]
Level 2 (mid-level) evidenceCao QL,Kenny D,Zhou D,Pan W,Guan L,Ge J,Hijazi ZM, Early clinical experience with a novel self-expanding percutaneous stent-valve in the native right ventricular outflow tract. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 24824357]
Level 3 (low-level) evidenceAlkashkari W,Alsubei A,Hijazi ZM, Transcatheter Pulmonary Valve Replacement: Current State of Art. Current cardiology reports. 2018 Mar 15; [PubMed PMID: 29546472]
Morray BH,McElhinney DB,Cheatham JP,Zahn EM,Berman DP,Sullivan PM,Lock JE,Jones TK, Risk of coronary artery compression among patients referred for transcatheter pulmonary valve implantation: a multicenter experience. Circulation. Cardiovascular interventions. 2013 Oct 1; [PubMed PMID: 24065444]
Level 2 (mid-level) evidenceShah N,Cheng VE,Cox N,Soon K, Percutaneous Coronary Intervention of an Anomalous Left Main Coronary Artery Arising from the Right Sinus of Valsalva. Heart, lung [PubMed PMID: 25911146]
Sridharan S,Coats L,Khambadkone S,Taylor AM,Bonhoeffer P, Images in cardiovascular medicine. Transcatheter right ventricular outflow tract intervention: the risk to the coronary circulation. Circulation. 2006 Jun 27; [PubMed PMID: 16801469]
Level 3 (low-level) evidenceLindsay I,Aboulhosn J,Salem M,Levi D, Aortic root compression during transcatheter pulmonary valve replacement. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 27121036]
Biernacka EK,Rużyłło W,Demkow M,Kowalski M,Śpiewak M,Piotrowski W,Kuśmierczyk M,Banaś S,Różanski J,Hoffman P, Transcatheter pulmonary valve implantation in patients with right ventricular outflow tract dysfunction: early and mid-term results. The Journal of invasive cardiology. 2015 Jun; [PubMed PMID: 26028663]
Boudjemline Y,Malekzadeh-Milani S,Patel M,Thambo JB,Bonnet D,Iserin L,Fraisse A, Predictors and outcomes of right ventricular outflow tract conduit rupture during percutaneous pulmonary valve implantation: a multicentre study. EuroIntervention : journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2016 Jan 22; [PubMed PMID: 25244126]
Level 2 (mid-level) evidenceMcElhinney DB,Cheatham JP,Jones TK,Lock JE,Vincent JA,Zahn EM,Hellenbrand WE, Stent fracture, valve dysfunction, and right ventricular outflow tract reintervention after transcatheter pulmonary valve implantation: patient-related and procedural risk factors in the US Melody Valve Trial. Circulation. Cardiovascular interventions. 2011 Dec 1; [PubMed PMID: 22075927]
Level 2 (mid-level) evidenceMcElhinney DB,Bergersen L,Marshall AC, In situ fracture of stents implanted for relief of pulmonary arterial stenosis in patients with congenitally malformed hearts. Cardiology in the young. 2008 Aug; [PubMed PMID: 18559137]
Level 2 (mid-level) evidenceCheung G,Vejlstrup N,Ihlemann N,Arnous S,Franzen O,Bundgaard H,Søndergaard L, Infective endocarditis following percutaneous pulmonary valve replacement: diagnostic challenges and application of intra-cardiac echocardiography. International journal of cardiology. 2013 Nov 30; [PubMed PMID: 24182680]
Level 3 (low-level) evidenceLurz P,Coats L,Khambadkone S,Nordmeyer J,Boudjemline Y,Schievano S,Muthurangu V,Lee TY,Parenzan G,Derrick G,Cullen S,Walker F,Tsang V,Deanfield J,Taylor AM,Bonhoeffer P, Percutaneous pulmonary valve implantation: impact of evolving technology and learning curve on clinical outcome. Circulation. 2008 Apr 15; [PubMed PMID: 18391109]
Level 2 (mid-level) evidenceChen XJ,Smith PB,Jaggers J,Lodge AJ, Bioprosthetic pulmonary valve replacement: contemporary analysis of a large, single-center series of 170 cases. The Journal of thoracic and cardiovascular surgery. 2013 Dec; [PubMed PMID: 23122698]
Level 2 (mid-level) evidenceBuber J,Bergersen L,Lock JE,Gauvreau K,Esch JJ,Landzberg MJ,Valente AM,Sandora TJ,Marshall AC, Bloodstream infections occurring in patients with percutaneously implanted bioprosthetic pulmonary valve: a single-center experience. Circulation. Cardiovascular interventions. 2013 Jun; [PubMed PMID: 23756696]
Level 2 (mid-level) evidencePatel M,Malekzadeh-Milani S,Ladouceur M,Iserin L,Boudjemline Y, Percutaneous pulmonary valve endocarditis: incidence, prevention and management. Archives of cardiovascular diseases. 2014 Nov; [PubMed PMID: 25445753]
Cheatham JP,Hellenbrand WE,Zahn EM,Jones TK,Berman DP,Vincent JA,McElhinney DB, Clinical and hemodynamic outcomes up to 7 years after transcatheter pulmonary valve replacement in the US melody valve investigational device exemption trial. Circulation. 2015 Jun 2; [PubMed PMID: 25944758]
Vezmar M,Chaturvedi R,Lee KJ,Almeida C,Manlhiot C,McCrindle BW,Horlick EM,Benson LN, Percutaneous pulmonary valve implantation in the young 2-year follow-up. JACC. Cardiovascular interventions. 2010 Apr; [PubMed PMID: 20398873]
Asoh K,Walsh M,Hickey E,Nagiub M,Chaturvedi R,Lee KJ,Benson LN, Percutaneous pulmonary valve implantation within bioprosthetic valves. European heart journal. 2010 Jun; [PubMed PMID: 20231157]
Level 2 (mid-level) evidenceDemkow M,Biernacka EK,Spiewak M,Kowalski M,Siudalska H,Wolski P,Sondergaard L,Miśko J,Hoffman P,Rużyłło W, Percutaneous pulmonary valve implantation preceded by routine prestenting with a bare metal stent. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 20602475]
Coats L,Khambadkone S,Derrick G,Hughes M,Jones R,Mist B,Pellerin D,Marek J,Deanfield JE,Bonhoeffer P,Taylor AM, Physiological consequences of percutaneous pulmonary valve implantation: the different behaviour of volume- and pressure-overloaded ventricles. European heart journal. 2007 Aug; [PubMed PMID: 17595193]
Zahn EM,Hellenbrand WE,Lock JE,McElhinney DB, Implantation of the melody transcatheter pulmonary valve in patients with a dysfunctional right ventricular outflow tract conduit early results from the u.s. Clinical trial. Journal of the American College of Cardiology. 2009 Oct 27; [PubMed PMID: 19850214]
Martins JD,Ewert P,Sousa L,Freitas I,Trigo C,Jalles N,Matos P,Agapito A,Ferreira R,Pinto FF, Percutaneous pulmonary valve implantation: initial experience. Revista portuguesa de cardiologia : orgao oficial da Sociedade Portuguesa de Cardiologia = Portuguese journal of cardiology : an official journal of the Portuguese Society of Cardiology. 2010 Dec; [PubMed PMID: 21428139]
Batra AS,McElhinney DB,Wang W,Zakheim R,Garofano RP,Daniels C,Yung D,Cooper DM,Rhodes J, Cardiopulmonary exercise function among patients undergoing transcatheter pulmonary valve implantation in the US Melody valve investigational trial. American heart journal. 2012 Feb; [PubMed PMID: 22305848]
Borik S,Crean A,Horlick E,Osten M,Lee KJ,Chaturvedi R,Friedberg MK,McCrindle BW,Manlhiot C,Benson L, Percutaneous pulmonary valve implantation: 5 years of follow-up: does age influence outcomes? Circulation. Cardiovascular interventions. 2015 Feb; [PubMed PMID: 25652317]
Level 2 (mid-level) evidenceHolzer RJ,Hijazi ZM, Transcatheter pulmonary valve replacement: State of the art. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 26423185]
Armstrong AK,Balzer DT,Cabalka AK,Gray RG,Javois AJ,Moore JW,Rome JJ,Turner DR,Zellers TM,Kreutzer J, One-year follow-up of the Melody transcatheter pulmonary valve multicenter post-approval study. JACC. Cardiovascular interventions. 2014 Nov; [PubMed PMID: 25459038]
Kenny D,Hijazi ZM,Kar S,Rhodes J,Mullen M,Makkar R,Shirali G,Fogel M,Fahey J,Heitschmidt MG,Cain C, Percutaneous implantation of the Edwards SAPIEN transcatheter heart valve for conduit failure in the pulmonary position: early phase 1 results from an international multicenter clinical trial. Journal of the American College of Cardiology. 2011 Nov 15; [PubMed PMID: 22078433]
Level 1 (high-level) evidenceFaza N,Kenny D,Kavinsky C,Amin Z,Heitschmidt M,Hijazi ZM, Single-center comparative outcomes of the Edwards SAPIEN and Medtronic Melody transcatheter heart valves in the pulmonary position. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography [PubMed PMID: 23008193]
Level 2 (mid-level) evidenceSuradi HS,Hijazi ZM, Percutaneous pulmonary valve implantation. Global cardiology science [PubMed PMID: 26535223]