Introduction
The deep tendon reflexes (DTR), particularly the tricep, patellar, and Achilles reflexes, were initially described by Wilhelm Heinrich Erb and Carl Friedrich Otto Westphal in adjacent articles simultaneously published in 1875 in the German Archives for Psychiatry and Nervous Diseases.[1] Since then, the Achilles reflex test, also called the ankle jerk test, has remained an essential component of the lower extremity neurologic exam. It is a myotatic (deep tendon) reflex that can be elicited easily with a reflex hammer to assess the S1 nerve root of the lumbosacral plexus. As for all deep tendon reflexes, the Achilles reflex is then interpreted by grading the response using a 0 to 4 scale and comparing it to the contralateral limb and nearby reflexes.[2][3]
Examining the DTRs such as the Achilles reflex provides insight into the function of the reflex arc and its' symmetry or lack thereof when compared to the contralateral side. Deep tendon reflexes remain an essential component of the neurologic exam that can guide further clinical decisions and differentiate between upper motor neuron and lower motor neuron pathology.[2][4][5]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
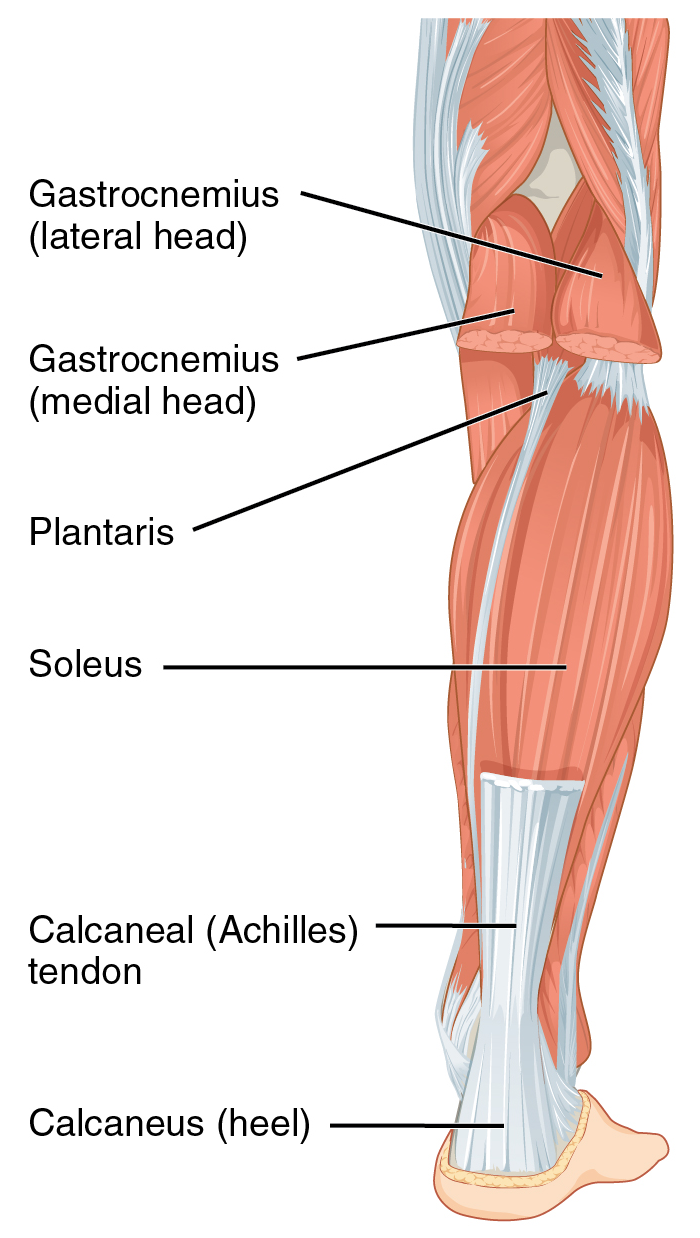
The Achilles tendon can be palpated just superior to the posterior aspect of the calcaneus. The strongest and largest tendon in the human body attaches the triceps surae (soleus and gastrocnemius) muscle to the calcaneal tuberosity.[6][7] The tendon is covered by a paratenon and not a tendon sheath. A paratenon is a thin fascial covering that decreases friction while serving as a conduit for blood vessels.[6][7]
Innervation and Reflex Arc
The Achilles tendon is innervated primarily by the S1 and S2 nerve roots of the tibial nerve.[7] The Achilles tendon reflex is a stretch reflex, which refers to the involuntary contraction of a muscle in response to passive stretching—tapping the tendon with a reflex hammer, a subsequent lengthening (stretch) in the triceps surae muscle, causing the muscle spindle's stretch receptors to be activated and propagate an excitatory stimulus. The stimulus is then carried by the Ia afferent neurons to the spinal cord, specifically to the cell bodies of the afferent neurons in the dorsal root ganglion.[4]
The afferent neurons then synapse on and activate an alpha motor neuron in the ventral horn of the spinal cord. The activated alpha motor neuron then transmits an efferent stimulus back to the neuromuscular junction of the agonist (triceps surae) muscle leading to a muscular contraction (reflex).[4] To ensure that the agonist muscle (triceps surae) of the reflex has an unopposed contraction, the Ia afferent neurons simultaneously stimulate an inhibitory neuron in the spinal cord that prevents the contraction of the antagonist (tibialis anterior) muscle.[8]
Although spinal reflex arcs bypass the brain to provide a quick response, the descending corticospinal tracts dampen and refine the amplitude of the reflex arc.[4] The S1 nerve root serves as the conduit for both the afferent and efferent impulses of the Achilles tendon reflex arc.
The deep tendon reflex arc is divided into the upper motor neuron (UMN) component and the lower motor neuron (LMN) component. The UMN component consists of the descending structures that transmit the dampening stimulus to the LMN at the ventral horn, such as the corticospinal tracts, brainstem, internal capsule, and cerebral cortex.[4] The LMN structures are the ventral (anterior) horn of the spinal cord and the peripheral nerve that innervates the muscle. The LMN of the Achilles reflex consists of the ventral horn of the S1 nerve root and the tibial nerve.
Indications
The Achilles reflex test is performed as part of any complete physical exam, particularly when assessing the neurologic functions of the lower extremities. When the pathology of the S1 nerve root is in question, the Achilles reflex test is the initial assessment of choice. It can aid in differentiating UMN pathology from LMN pathology as well as help in localizing the lesion.[4] Additionally, it can provide information on peripheral nerve function, which can be of utmost importance in certain patient populations, such as those with diabetes mellitus and hypothyroidism.[9][10][11]
Contraindications
Generally, there are no contraindications to performing the Achilles reflex test; however, one may have to defer the test in cases of injury. These injuries could be secondary to trauma or any underlying disorders that make the procedure difficult for the examiner to perform and the patient to sustain. Other possible contraindications are skin disorders. For instance, if a patient has advanced psoriasis of the overlying skin, it could be uncomfortable for the patient to undergo this procedure.
Equipment
The Achilles reflex can be elicited using reflex hammers. Modern-day reflex hammers are available in four styles: Taylor hammer, Queen Square hammer, Babinski hammer, and the Troemner hammer. However, no study has shown any hammer to be superior to the next; selection is based purely on preference and tradition of the institution. A practitioner holds a standard reflex hammer by the handle in a firm manner, typically with their dominant thumb and forefinger holding most of the weight with the flat part of the top toward the patient’s Achilles tendon area. Other, larger, and more advanced reflex hammers, like a pendulum hammer, can also be used to assess the Achilles reflex.[12]
Personnel
Any healthcare professional who has had training may perform the procedure, including nurse practitioners, physician associates, and doctors.
Preparation
There is minimal preparation needed to complete the Achilles reflex test. The patient should be relaxed, lying on an examination table, and their Achilles tendon area well exposed from the superior calf to the plantar aspect of the foot. The practitioner should have washed hands, reflex hammer in hand, and should be in the position to perform the exam.[12]
Technique or Treatment
There are various ways to perform an Achilles reflex test.[12] The traditional approach elicits the reflex with a "tendon tap," where the examiner strikes the Achilles tendon.[13] The conventional "tendon tap" can be performed with the patient in a supine position, knee flexed, and hip externally rotated on the examination table. One hand is slightly dorsiflexing the foot from the plantar aspect, as the other hand strikes the Achilles tendon with the reflex hammer. This approach can also be performed with the leg dangling off the examination table or with the leg elevated and held up by the examiner.[12]
The plantar strike is an alternative method of assessing the Achilles tendon reflex that may be of use, particularly for hospitalized patients with limited mobility. A plantar strike allows the examiner to assess the reflex while the patient remains supine with extended legs. The plantar strike method is performed by tapping the examiner's fingers on the patient's forefoot with slight tension causing dorsiflexion. A plantarflexion reflex should then be observed. The "plantar tap" has been shown to have 89% concordance with the traditional Achilles "tendon tap," regardless of the examiner's experience level.[13] Furthermore, it has been shown that the plantar strike or the Achilles tendon strike with an elevated leg provides the most reliable results when examining elderly patients, as it is commonly difficult to elicit in this patient population.[12]
A pendulum hammer can also elicit the Achilles reflex in a standing patient.[14] Examing a standing patient allows for the assessment of the reflex arc during postural control, as it is known that reflex excitability varies during functional motor commands.[15] Reflex arc assessment during the muscular engagement, such as when standing, allows for assessing the entire spinal reflex arc.[14] However, it is more commonly used in the research setting.
Reinforcement
Occasionally, reinforcement of deep tendon reflexes can be performed to elicit a reflex that might not be observed otherwise in that patient. The Jendrassik maneuver is a commonly employed reinforcement technique in which the patient is asked to hook their hands together with flexed fingers while trying to pull apart as firmly as possible.[2][16] The use of the Jendrassik maneuver was shown to make the Achilles reflex appear in 70% of normal elderly patients with an absent reflex prior to reinforcement.[17]
Clinical Significance
Reflex Grade
As previously mentioned, the Achilles reflex test is interpreted and graded based on reflex amplitude using a scale such as the NINDS Myotatic Reflex Scale.[18] The NINDS scale uses a 0 to 4 grading system:
- 0 = reflex is absent
- 1 = Reflex is small, less than normal; includes a trace response or a response brought out only with reinforcement
- 2 = Reflex is in the lower half of the normal range
- 3 = Reflex is in the upper half of the normal range
- 4 = Reflex enhanced, more than normal; includes clonus if present, which optionally can be noted in an added verbal description of the reflex
Additionally, a plus (+) or a minus (-) can be added to the number grade to identify an in-between grade response. A grading of 5 can also be used to denote a sustained clonus of >10 rhythmic oscillations after briskly stretching a hyperreflexic muscle, usually performed in the Achilles tendon.
Interpretation of Observed Reflex
When examining deep tendon reflexes, it is of utmost importance to compare each reflex response to the corresponding contralateral side. A numeric grading scale remains a subjective quantifier that depends on the examiner's preconceived idea of what a specific grade should be. However, the observation of an asymmetric reflex should be observed across all examiners regardless of their individual grade assignment. Hyporeflexia, hyperreflexia, and asymmetric responses are abnormal and should prompt further examination.[2]
Hyporeflexia is usually indicative of LMN disease, that is, of the peripheral nerve or the anterior (ventral) horn of the spinal cord for that particular level.[5] Disease or disruption of the LMN causes a diminished or absent reflex as the stimulus is not transmitted to the effector muscle. Additional features of LMN disease are the presence of flaccidity or diminished muscle tone, weakness, fasciculations, and muscular atrophy.[4]
The causes of LMN disease include acquired peripheral neuropathies, hereditary causes, or structural damage to the LMN.[19] Peripheral neuropathies are the most common cause of absent or diminished reflexes.[2] Physiologic derangements caused by diabetes mellitus, hypothyroidism, uremia, vitamin or electrolyte deficiencies, and toxins such as lead or arsenic can commonly present with hyporeflexia. Diminished or absent Achilles tendon reflex is commonly seen in patients with hypothyroidism or diabetes mellitus.[20][21] Furthermore, the absence of the Achilles tendon reflex has been shown to have 72.1% sensitivity and 90.6% specificity in identifying peripheral neuropathy in elderly patients.[21]
Medications such as isoniazid, vincristine, and diphenylhydantoin are also known to cause hyporeflexia. There are multiple hereditary and immune-related causes of hyporeflexia, including but not limited to spinobulbar muscular atrophy, spinal muscular atrophy, distal hereditary motor neuropathies, and Guillian-Barre syndrome.[19] Structural damage to the LMN components of the tibial nerve can occur with neural foraminal stenosis or a herniated intervertebral disc at the L5-S1 level that compresses the S1 nerve root.
Hyperreflexia is indicative of UMN disease. Damage to any UMN components (corticospinal tracts, brainstem, internal capsule, and cerebral cortex) leads to a hyperactive deep tendon reflex due to the disinhibition of the spinal reflex arc.[22] As previously described, the upper motor neurons are essential in dampening the reflex response. In addition to hyperreflexia, UMN lesions present with spasticity or increased muscle tone and weakness, as well as various pathological reflexes such as the Babinski sign, clonus, Hoffman sign, and radiation of reflexes to other muscle groups. Causes of UMN damage can be due to anoxic brain injury, brain trauma or spinal cord trauma, cerebrovascular accidents, neurodegenerative disorders (amyotrophic lateral sclerosis, primary lateral sclerosis, multiple sclerosis), spinal cord compression, or malignancy, to name a few.[5]
Enhancing Healthcare Team Outcomes
The Achilles tendon reflex is a simple maneuver that is part of any lower extremity neurologic exam. It can be performed relatively easily both in the clinic and inpatient environment. However, differences in technique and experience can lead to varying intra-patient results. Various case-control studies have been published that compare the traditional Achilles tendon tap to the plantar tap and the reproducibility across different experience levels (Level 3).[12][23][13]
When comparing the two Achilles reflex methods, it was shown that the traditional Achilles tendon tap had less inter-observer and intra-observer reliability.[12][23][13] The plantar tap method had greater reproducibility. When comparing senior-level physicians to junior level, the plantar tap had significant inter-observer reliability (p < 0.001).[23] The intra-observer reliability was not significant in the senior level practitioners but did show a significant difference for the junior level physicians (p < 0.05).[23] Additionally, 84% of ankle jerks would have initially been called absent if final-year medical students would not perform a plantar tap method for confirmation.[12]
The ubiquitous nature of the Achilles reflex test and its use by senior physicians, junior physicians, medical students, nurses, and physician assistants, necessitate a reliable confirmatory alternative. Considering the interdisciplinary structure of patient care teams with varying levels of experience, it is prudent to consider using the plantar tap method. Particularly for patient populations that you may suspect a diminished or altered reflex response, such as the elderly, diabetic, and hypothyroid patients.
Media
(Click Video to Play)
Ankle Deep Tendon Reflex Clinical Examination. This video shows how to conduct the ankle deep tendon reflex test. Landmarks include the Achilles tendon and calf and plantar muscles.
Contributed by RS Menon, MD (https://www.youtube.com/watch?v=62jADalpDaI)
(Click Video to Play)
Clinical Examination of Ankle Clonus. Clinical examination of ankle clonus is typically demonstrated in upper motor neuron lesions or serotonin syndrome.
Contributed by RS Menon, MD
(Click Video to Play)
(Click Image to Enlarge)
References
Tyler KL, McHenry LC Jr. Fragments of neurological history. The knee jerk and other tendon reflexes. Neurology. 1983 May:33(5):609-10 [PubMed PMID: 6341874]
Walker HK, Hall WD, Hurst JW, Walker HK. Deep Tendon Reflexes. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:(): [PubMed PMID: 21250237]
Litvan I, Mangone CA, Werden W, Bueri JA, Estol CJ, Garcea DO, Rey RC, Sica RE, Hallett M, Bartko JJ. Reliability of the NINDS Myotatic Reflex Scale. Neurology. 1996 Oct:47(4):969-72 [PubMed PMID: 8857728]
Zimmerman B, Hubbard JB. Deep Tendon Reflexes. StatPearls. 2023 Jan:(): [PubMed PMID: 30285397]
Zayia LC, Tadi P. Neuroanatomy, Motor Neuron. StatPearls. 2023 Jan:(): [PubMed PMID: 32119503]
Koivunen-Niemelä T, Parkkola K. Anatomy of the Achilles tendon (tendo calcaneus) with respect to tendon thickness measurements. Surgical and radiologic anatomy : SRA. 1995:17(3):263-8 [PubMed PMID: 7502192]
O'Brien M. The anatomy of the Achilles tendon. Foot and ankle clinics. 2005 Jun:10(2):225-38 [PubMed PMID: 15922915]
Signorile JF, Applegate B, Duque M, Cole N, Zink A. Selective recruitment of the triceps surae muscles with changes in knee angle. Journal of strength and conditioning research. 2002 Aug:16(3):433-9 [PubMed PMID: 12173959]
Franco G, Malamani T. [Achilles reflexogram and hemodynamic parameters in the evaluation of thyroid function]. Minerva medica. 1976 Oct 27:67(51):3325-34 [PubMed PMID: 995289]
Pampoulov L. [Various particularities of the duration of the achilles reflex in diabetic patients]. Le Diabete. 1970 Jul-Sep:18(3):179-84 [PubMed PMID: 5472236]
Ballantyne GH, Croxson MS. The effect of exercise, thyroid status and insulin-induced hypoglycaemia on the Achilles tendon reflex time in man. European journal of applied physiology and occupational physiology. 1981:46(1):77-83 [PubMed PMID: 7014217]
Ziff M, Stark RJ. How to assess tendon reflexes of the lower limb in the elderly. Journal of the neurological sciences. 2017 Jan 15:372():196-200. doi: 10.1016/j.jns.2016.11.044. Epub 2016 Nov 22 [PubMed PMID: 28017211]
Schwartz RS, Morris JG, Crimmins D, Wilson A, Fahey P, Reid S, Joffe R. A comparison of two methods of eliciting the ankle jerk. Australian and New Zealand journal of medicine. 1990 Apr:20(2):116-9 [PubMed PMID: 2344316]
Level 1 (high-level) evidenceMildren RL, Zaback M, Adkin AL, Frank JS, Bent LR. Reliability of the Achilles tendon tap reflex evoked during stance using a pendulum hammer. Gait & posture. 2016 Jan:43():182-6. doi: 10.1016/j.gaitpost.2015.09.020. Epub 2015 Sep 30 [PubMed PMID: 26454702]
Stein RB, Capaday C. The modulation of human reflexes during functional motor tasks. Trends in neurosciences. 1988 Jul:11(7):328-32 [PubMed PMID: 2465639]
Ertuglu LA, Aydin A, Kumru H, Valls-Sole J, Opisso E, Cecen S, Türker KS. Jendrassik maneuver effect on spinal and brainstem reflexes. Experimental brain research. 2019 Dec:237(12):3265-3271. doi: 10.1007/s00221-019-05668-y. Epub 2019 Oct 24 [PubMed PMID: 31650212]
Impallomeni M, Kenny RA, Flynn MD, Kraenzlin M, Pallis CA. The elderly and their ankle jerks. Lancet (London, England). 1984 Mar 24:1(8378):670-2 [PubMed PMID: 6142359]
Hallett M. NINDS myotatic reflex scale. Neurology. 1993 Dec:43(12):2723 [PubMed PMID: 7802740]
Garg N, Park SB, Vucic S, Yiannikas C, Spies J, Howells J, Huynh W, Matamala JM, Krishnan AV, Pollard JD, Cornblath DR, Reilly MM, Kiernan MC. Differentiating lower motor neuron syndromes. Journal of neurology, neurosurgery, and psychiatry. 2017 Jun:88(6):474-483. doi: 10.1136/jnnp-2016-313526. Epub 2016 Dec 21 [PubMed PMID: 28003344]
NUTTALL FQ, DOE RP. THE ACHILLES REFLEX IN THYROID DISORDERS; A CRITICAL EVALUATION. Annals of internal medicine. 1964 Aug:61():269-88 [PubMed PMID: 14204862]
Richardson JK. The clinical identification of peripheral neuropathy among older persons. Archives of physical medicine and rehabilitation. 2002 Nov:83(11):1553-8 [PubMed PMID: 12422324]
Level 2 (mid-level) evidenceEmos MC, Rosner J. Neuroanatomy, Upper Motor Nerve Signs. StatPearls. 2023 Jan:(): [PubMed PMID: 31082126]
O'Keeffe ST, Smith T, Valacio R, Jack CI, Playfer JR, Lye M. A comparison of two techniques for ankle jerk assessment in elderly subjects. Lancet (London, England). 1994 Dec 10:344(8937):1619-20 [PubMed PMID: 7695707]
Level 1 (high-level) evidence