Introduction
Handwashing practices in the patient care setting began in the early 19th century. The practice evolved over the years with evidential proof of its vast importance and coupled with other hand-hygienic practices, decreased pathogens responsible for nosocomial or hospital-acquired infections (HAI). [1][2][3]
Contaminated hands of healthcare providers are a primary source of pathogenic spread. Proper hand hygiene decreases the proliferation of microorganisms, thus reducing infection risk and overall healthcare costs, length of stays, and ultimately, reimbursement.
According to the Centers for Disease Control and Prevention (CDC), hand hygiene is the single most important practice in the reduction of the transmission of infection in the healthcare setting[4][2]. Despite this evidence, studies have repeatedly shown that the importance of hygiene has not been adequately recognized amongst healthcare professionals and compliance remains low [5].
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
According to the CDC, understanding the importance of hand hygiene and its impact on the pathogenic spread of microorganisms is best understood when one understands the anatomy of the skin. The skin serves as a protective barrier against water loss, heat loss, microorganisms, and other environmental hazards.[6]
Structurally, the skin is made up of an outer, superficial layer known as the stratum corneum, the epidermis, dermis, and the hypodermis. Healthy skin is colonized with resident flora that are microorganisms that reside below the stratum corneum and the skin's surface [7]. This flora has two main functions: microbial antagonism and competing for nutrients within the ecosystem. Generally, these bacteria are not pathogenic on intact skin but may cause infections in other areas of the body such as nonintact skin, the eyes, or sterile body cavities [7].
Transient microorganisms are often acquired by healthcare workers through direct, close contact with patients or contaminated inanimate objects or environmental surfaces. Transient flora colonizes the superficial skin layers [8]. It can be removed by routine handwashing more easily than resident flora. These organisms vary in number depending upon body location. Healthcare-associated infections are a result of these transient organisms.[9][10][11][12]
Indications
According to the CDC, hand hygiene encompasses the cleansing of your hands with soap and water, antiseptic hand washes, antiseptic hand rubs such as alcohol-based hand sanitizers, foams or gels, or surgical hand antisepsis. Indications for handwashing include when hands are visibly soiled, contaminated with blood or other bodily fluids, before eating, and after restroom use. Hands should be washed if potential there was potential exposure to Clostridium difficile, Norovirus, or Bacillus anthracis.[13][14]
In 2009, the World Health Organization (WHO) highlighted preset guidelines known as the "Five Moments for Hand Hygiene." [15]
- Before touching or coming into contact with a patient
- Before performing a clean or aseptic procedure
- After an exposure risk to bodily fluids and glove removal
- After contact with a patient and their immediate surroundings
- After touching an inanimate object in the patient's immediate surroundings even if no direct patient contact
Alcohol-based hand sanitizers are the recommended product for hand hygiene when hands are not visibly soiled. Apply alcohol-based products per manufacturer guidelines on dispensing of the product. Typically, 3 mL to 5 mL in the palm, rubbing vigorously, ensuring all surfaces on both hands get covered, about 20 seconds is required for all surfaces to dry completely [15].
Patient and facility healthcare professionals are monitored for hand-washing practices, and they are conforming to hand-hygiene practices. This practice is becoming increasingly popular as healthcare professionals strive for a safer environment.
Contraindications
Artificial nails and nail extensions contain pathogens in the subungual spaces; thus posing a threat to microorganism transmission in the healthcare arena. Therefore, it is recommended that healthcare professionals do not use them. Well-manicured nails and adherence to artificial nail policies outlined in facility-specific guidelines are vital to hand hygiene practices. The WHO guidelines recommend that nails should be kept less than 0.5cm long [15].
Hand rubbing with an alcohol-based rub should not be performed when the hands are visibly soiled. In this case, the CDC and WHO guidelines recommend that handwashing with soap and water [15].
Equipment
Handwashing is the act of washing hands with soap, either antimicrobial or nonantimicrobial, and water for at least 15 to 20 seconds with a vigorous motion to cause friction making sure to include all surfaces of the hands and fingers.
It requires a specific skill set to ensure proper technique.
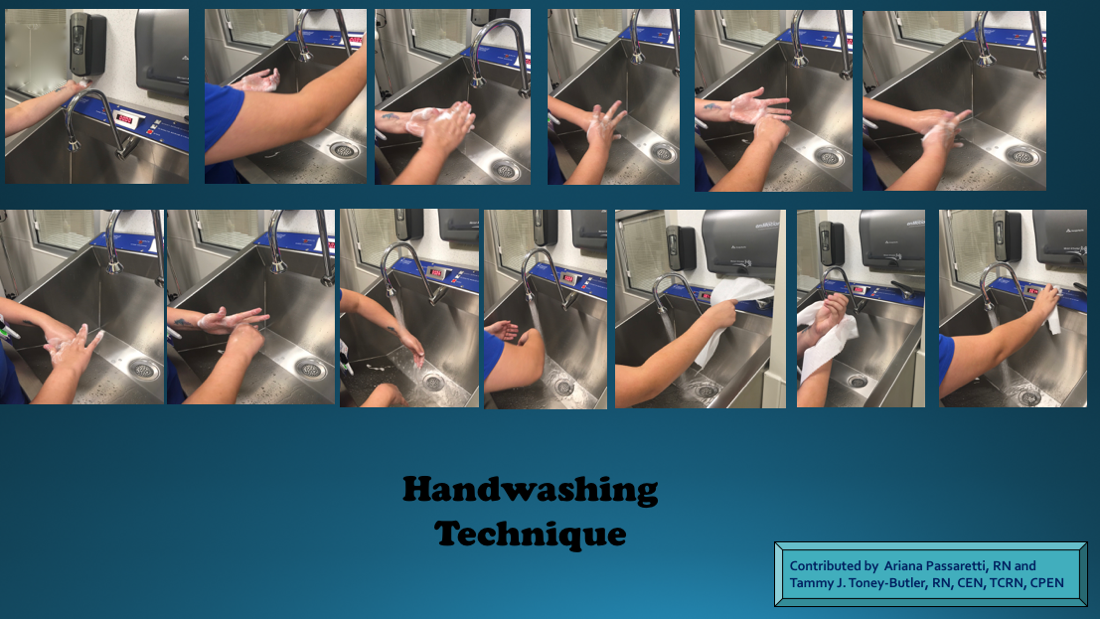
Handwashing Technique: [15]
- Begin by standing in front of the sink and taking care not to touch sink surfaces with hands or uniform/lab coat.
- If hands touch sinks at any time during this process, they are considered contaminated, and you must start the process over.
- Turn on the warm water. Allow water to wet hands and wrists thoroughly.
- Remember to keep hands and forearms lower than your elbows, so cross-contamination from water running back does not occur.
- Water should flow in a manner from least to most contaminated areas such as the hands. Microorganisms get washed down the sink.
- Apply approximately 3 mL to 5 mL of an antiseptic soapy solution. Soap requires even distribution with a nice lather making sure all areas of hands receive covering in soap.
- Next, use friction or rubbing of hands and wrists for no less than 15-20 seconds to ensure the removal of germs.
- Use a timer or timed sink if available.
- This vigorous rubbing of hands and wrists will include anterior and posterior surfaces, cuticle area, underneath nails, and in between each finger.
- Leave no part of the hand or wrist untouched.
- Interlace fingers, rub palms and backs of hands at least five times each to ensure all areas have coverage.
- The World Health Organization (WHO) recommends 6 steps in hand hygiene. This includes palm to palm, right palm over the left dorsum and vice versa, palm to palm with fingers interlaced, backs of fingers to opposing palms, rubbing of thumbs and fingertips.
- Rinse hands and wrists making sure all soap has been successfully washed off.
- When rinsing off water remember to keep hands down and elbows up, then dry hands and wrists entirely with clean or disposable towels.
- Throw towels away if disposable or place in the appropriate place/hamper/bin without coming into contact with these objects.
- The end of handwashing will involve making sure you do not recontaminate your hands by touching the sink or faucet handles to turn the water off. Once hands are washed and dried, use a towel to turn off the water and then dispose of it in the appropriate container.
- Surgical sinks/handwashing stations have timers such as in trauma bays that automatically shut off at specific time intervals. These guard against recontamination of hands/wrists by ensuring there is no need to turn the water off manually.
Personnel
Healthcare professionals caring for high-risk patients that are immunocompromised must take great care in performing proper hand hygiene as this patient population is at high risk for opportunistic infections [16]. Handwashing with soap and water will remove nearly all transient gram-negative bacilli in 10 seconds while chlorhexidine may be more appropriate than soap and water for the removal of transient gram-positive bacteria [16].
Handwashing is a requirement if potential there was potential exposure to Clostridium difficile, Norovirus, or Bacillus anthracis. Clostridium difficile and Bacillus anthracis contain spores, and none of the agents used in antiseptic handwash or hand-rub preparations are reliably sporicidal. In these cases, vigorous handwashing with soap will assist in the removal of the spores from the skin.
According to the CDC, established guidelines recommend that agents used for surgical hand scrubs should reduce microorganisms on intact skin in a substantial manner, contain a nonirritating antimicrobial preparation, have broad-spectrum activity, and be fast-acting and persistent. Studies have demonstrated that formulations containing 60% to 95% alcohol alone or 50% to 95% in combination with other products lower bacterial counts on the skin immediately post-scrub more effectively than other agents [15].
Technique or Treatment
Surgical hand antiseptic practices began in the late 1800s and remain vital to the prevention of infection today. Surgical hand antisepsis or hand hygiene for surgery requires a different set of skills than regular handwashing techniques [17]. The inadvertent transfer of microorganisms to a patient's surgical site can result in a surgical site infection, these are one of the most common forms of hospital-associated infections for surgical patients [18]. Carrying out the correct hand hygiene steps prior to surgery can help reduce the risk of surgical site infections.
According to the CDC, "Hand Hygiene in the Healthcare Settings," hand hygiene for surgery follows specific vital steps using either an antimicrobial soap or an alcohol-based hand sanitizer before donning sterile gloves for surgical procedures. In contrast to hygienic handwashing, surgical hand preparation must remove the transient flora and reduce the presence of resident flora [17].
Surgical Hand Antisepsis Steps [17] [18]
- Remove all jewelry such as rings, watches, and bracelets before beginning the surgical hand scrub.
- Inspect hands for cuts, cuticle damage, open lesions or abrasions.
- Apply surgical shoe covers, hats, caps, masks, and eye protection next.
- Turn on water using foot/knee controls to the desired warm temperature.
- Perform a pre-rinse ensuring soap gets to about two inches above the elbows remembering the hands must be kept above the elbows at all times during this process as well as during the rinse.
- Begin debris removal from underneath fingernails using a nail pick while the water is running.
- When performing surgical hand antisepsis using an antimicrobial agent, scrub hands, fingers, and forearms for 2 to 6 minutes typically, but follow manufacturer guidelines and facility-specific policies and procedures. Some institutions suggest a certain number of strokes when cleansing the nails, palms, hands, and forearms.
- Brush methods may be used and are facility-specific. Long scrub times (e.g., 10 minutes) are not a recommendation due to the potential to irritate hands and nonsupporting evidence of its benefit versus risk.
- Shorter scrub times with a two-stage surgical scrub technique may be standard in some institutions.
- Remember, when rinsing soap/agent off, allow water to run off at the elbows, ensuring the hands remain clean and free of microbes.
- Foot or knee controls are used to turn the water off.
- Hands stay elevated and away from the body at all times.
- Approach sterile field, grasp towel, avoid dripping excess water on your sterile field, and dry one hand.
- Obtain a new sterile towel or reverse the first towel and dry the other hand.
- Drop towel into a nearby linen hamper or carefully handoff to another member of the healthcare team.
- After application of the alcohol-based product or antiseptic hand rub as recommended, allow hands and forearms to dry thoroughly before donning sterile gloves.
Clinical Significance
Hand hygiene practices are paramount in reducing cross-transmission of microorganisms, hospital-acquired infections and the risk of occupational exposure to infectious diseases.
Mortality and morbidity increase in the presence of hospital-acquired infections, thus diligent hand hygiene is essential to providing safe, cost-efficient, quality care to our patients.
Educational programs for patients and healthcare providers, ergonomics, and staffing ratios all play a role in hand hygiene compliance.
Enhancing Healthcare Team Outcomes
All healthcare workers should regularly wash hands as this is the most cost-effective way to prevent transmission of infections. While compliance with handwashing is high among healthcare workers, the same is not true of the public. Thus, the nurse, pharmacist and physician should educate the patient on the benefits of handwashing at every clinic visit. [19][20][21]
Media
(Click Image to Enlarge)
References
Hassan MZ, Chowdhury MAB, Hassan I, Chowdhury F, Schaefer N, Chisti MJ. Respiratory viral infection in early life and development of asthma in childhood: A protocol for systematic review and meta-analysis. Medicine. 2019 May:98(18):e15419. doi: 10.1097/MD.0000000000015419. Epub [PubMed PMID: 31045799]
Level 1 (high-level) evidenceGammon J, Hunt J. The neglected element of hand hygiene - significance of hand drying, efficiency of different methods and clinical implication: A review. Journal of infection prevention. 2019 Mar:20(2):66-74. doi: 10.1177/1757177418815549. Epub 2018 Dec 5 [PubMed PMID: 30944590]
McMichael C. Water, Sanitation and Hygiene (WASH) in Schools in Low-Income Countries: A Review of Evidence of Impact. International journal of environmental research and public health. 2019 Jan 28:16(3):. doi: 10.3390/ijerph16030359. Epub 2019 Jan 28 [PubMed PMID: 30696023]
Gold NA, Mirza TM, Avva U. Alcohol Sanitizer. StatPearls. 2023 Jan:(): [PubMed PMID: 30020626]
Pittet D. Improving compliance with hand hygiene in hospitals. Infection control and hospital epidemiology. 2000 Jun:21(6):381-6 [PubMed PMID: 10879568]
Hoang D, Khawar N, George M, Gad A, Sy F, Narula P. Video didactic at the point of care impacts hand hygiene compliance in the neonatal intensive care unit (NICU). Journal of healthcare risk management : the journal of the American Society for Healthcare Risk Management. 2018 Apr:37(4):9-15. doi: 10.1002/jhrm.21314. Epub 2018 Feb 6 [PubMed PMID: 29405485]
Kampf G, Kramer A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clinical microbiology reviews. 2004 Oct:17(4):863-93, table of contents [PubMed PMID: 15489352]
Kapil R, Bhavsar HK, Madan M. Hand hygiene in reducing transient flora on the hands of healthcare workers: an educational intervention. Indian journal of medical microbiology. 2015 Jan-Mar:33(1):125-8. doi: 10.4103/0255-0857.148409. Epub [PubMed PMID: 25560015]
Biezen R, Grando D, Mazza D, Brijnath B. Visibility and transmission: complexities around promoting hand hygiene in young children - a qualitative study. BMC public health. 2019 Apr 11:19(1):398. doi: 10.1186/s12889-019-6729-x. Epub 2019 Apr 11 [PubMed PMID: 30975108]
Level 2 (mid-level) evidenceKang YS, Chang YJ. Using a motion-controlled game to teach four elementary school children with intellectual disabilities to improve hand hygiene. Journal of applied research in intellectual disabilities : JARID. 2019 Jul:32(4):942-951. doi: 10.1111/jar.12587. Epub 2019 Apr 2 [PubMed PMID: 30941883]
Le CD, Lehman EB, Nguyen TH, Craig TJ. Hand Hygiene Compliance Study at a Large Central Hospital in Vietnam. International journal of environmental research and public health. 2019 Feb 19:16(4):. doi: 10.3390/ijerph16040607. Epub 2019 Feb 19 [PubMed PMID: 30791457]
Korhonen A, Vuori A, Lukkari A, Laitinen A, Perälä M, Koskela T, Pölkki T. Increasing nursing students' knowledge of evidence-based hand-hygiene: A quasi-experimental study. Nurse education in practice. 2019 Feb:35():104-110. doi: 10.1016/j.nepr.2018.12.009. Epub 2019 Jan 2 [PubMed PMID: 30772734]
Yap M, Chau ML, Hartantyo SHP, Oh JQ, Aung KT, Gutiérrez RA, Ng LC. Microbial Quality and Safety of Sushi Prepared with Gloved or Bare Hands: Food Handlers' Impact on Retail Food Hygiene and Safety. Journal of food protection. 2019 Apr:82(4):615-622. doi: 10.4315/0362-028X.JFP-18-349. Epub [PubMed PMID: 30907665]
Level 2 (mid-level) evidenceMutters R, Warnes SL. The method used to dry washed hands affects the number and type of transient and residential bacteria remaining on the skin. The Journal of hospital infection. 2019 Apr:101(4):408-413. doi: 10.1016/j.jhin.2018.12.005. Epub 2018 Dec 8 [PubMed PMID: 30537524]
. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care. 2009:(): [PubMed PMID: 23805438]
Level 3 (low-level) evidenceAlothman A. Infection control and the immunocompromised host. Saudi journal of kidney diseases and transplantation : an official publication of the Saudi Center for Organ Transplantation, Saudi Arabia. 2005 Oct-Dec:16(4):547-55 [PubMed PMID: 18202509]
Level 3 (low-level) evidenceWidmer AF, Rotter M, Voss A, Nthumba P, Allegranzi B, Boyce J, Pittet D. Surgical hand preparation: state-of-the-art. The Journal of hospital infection. 2010 Feb:74(2):112-22. doi: 10.1016/j.jhin.2009.06.020. Epub 2009 Aug 28 [PubMed PMID: 19716627]
Level 3 (low-level) evidenceTanner J, Dumville JC, Norman G, Fortnam M. Surgical hand antisepsis to reduce surgical site infection. The Cochrane database of systematic reviews. 2016 Jan 22:2016(1):CD004288. doi: 10.1002/14651858.CD004288.pub3. Epub 2016 Jan 22 [PubMed PMID: 26799160]
Level 1 (high-level) evidenceSuen LKP, So ZYY, Yeung SKW, Lo KYK, Lam SC. Epidemiological investigation on hand hygiene knowledge and behaviour: a cross-sectional study on gender disparity. BMC public health. 2019 Apr 11:19(1):401. doi: 10.1186/s12889-019-6705-5. Epub 2019 Apr 11 [PubMed PMID: 30975130]
Level 2 (mid-level) evidenceGuo N, Ma H, Deng J, Ma Y, Huang L, Guo R, Zhang L. Effect of hand washing and personal hygiene on hand food mouth disease: A community intervention study. Medicine. 2018 Dec:97(51):e13144. doi: 10.1097/MD.0000000000013144. Epub [PubMed PMID: 30572426]
Gomez NJ. Hand Washing Adherence - Is That Really Our Goal? Nephrology nursing journal : journal of the American Nephrology Nurses' Association. 2018 Jul-Aug:45(4):393-394 [PubMed PMID: 30303649]