Introduction
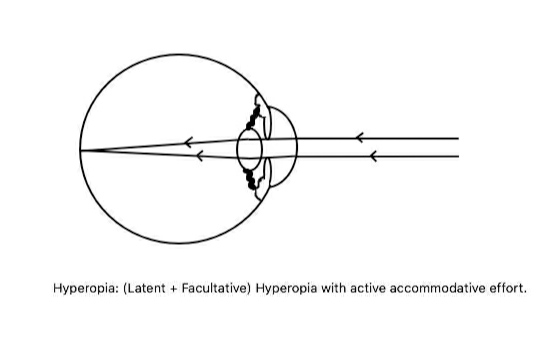
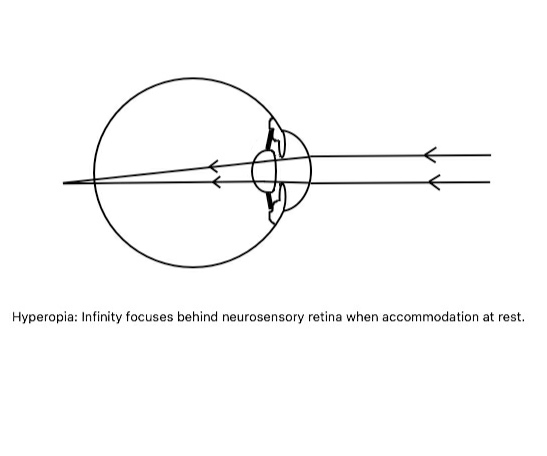
The most common refractive error in childhood is hyperopia.[1] The term hyperopia refers to the refractive condition of the eye where parallel light rays coming from the infinity are focussed behind the neurosensory retina (after refraction through the ocular media ) when accommodation is at rest. The spontaneous accommodative effort of the human eye, by increasing the anterior curvature and converging power of the crystalline lens, usually tries to overcome this situation. So, accommodative rest is mandatory to elicit total hyperopia, specifically in young individuals.[2]
By birth, human beings are predominantly hyperopic, and as the age progresses, hyperopic eyeballs grow to become emmetropic or even myopic.[3][4] Positive family history plays a crucial role in the development of hyperopia in the next generations.[5] If left untreated after diagnosis, sequelae such as amblyopia and tropia may develop.[6][7][6]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Conventionally the hyperopia is etiologically classified into:
Axial hyperopia (most common - simple hyperopia): It is due to anterior-posterior axial shortening of the eyeball. Genetic predisposition plays an important role. Retinal edema can cause a hyperopic shift. 1 mm decrease in axial length leads to 3 diopters of hyperopia.[8]
Curvature hyperopia: It is due to flattening of the cornea or the lens or both. A radius of curvature increase in 1 mm leads to 6 diopters of hyperopia.
Index hyperopia: It is due to the change in the refractive index of the crystalline lens, which occurs in old age or diabetics. The refractory index gradually increases from the center to the periphery.
Positional hyperopia or absence of the lens (aphakia) or ocular pathologic conditions: This condition occurs due to malposition or absence of the crystalline lens (congenital or acquired) or intraocular lens owing to the creation of an aphakic zone in refractive media. Post-traumatic or post-surgical aphakia is not an uncommon cause of hyperopia.
Few ocular pathologies, e.g., nanophthalmos, microphthalmos, aniridia, may cause hyperopia.
No unanimous causative factor is identified to date. Though sporadic, few genetic factors have been identified in association with hyperopia. Apart from genetic and environmental factors, few acquired conditions are also responsible, specifically in aged persons.[9] The following are a few identified conditions leading to hyperopia:
- 16p11.2 microdeletion[10]
- Myelin regulatory factor gene (MYRF) mutation[11]
- Family history of squint, and a history of maternal smoking during pregnancy[12]
- Cortical cataract (index hyperopia)
- Aphakia (congenital or acquired)[13]
- Hyperglycemia[14]
- Diabetes mellitus and after prompt control of hyperglycemia in diabetes mellitus[15][16]
- Prolonged space mission due to retina and optic nerve head edema[17]
- Peripapillary pachychoroid syndrome (PPS)[18]
- Heimler syndrome[19]
- Kenny syndrome[20]
- Accommodation loss due to complete CN III nerve palsy or internal ophthalmoplegia or paralysis by cycloplegic drops, lorazepam (functional hyperopia)[21][22][21]
- After silicone oil injection in phakic and pseudophakic eyes. In aphakic eyes, the amount of hyperopia reduces, but the eye remains hyperopic
- Loeys-Dietz syndrome, Larsen syndrome.[23]
- Leber congenital amaurosis
- X-linked retinoschisis and senile retinoschisis
Epidemiology
Axial hyperopia, being the commonest, is usually present from birth.[3] The prevalence of moderate hyperopia, i.e., ≥ +2 diopter at 6 and 12 years of age, is 13.2% and 5.0%, respectively, and it is more in White race individuals than in other ethnic groups.[24] The prevalence of hyperopia ≥+4 diopter was 3.2% in the worse eye, with both eyes involved in 64.4% of cases in a study.[12] For United States participants, non-Hispanic, and Hispanic White races have a significantly higher risk of hyperopia in 6 to 72 months of age group.[12]
In 15 years or less age group, and ≥30 years age group, hyperopia prevalence was higher in females.[25] A systematic review of refractive error revealed that the prevalence of hyperopia is 4% (less than myopia) in the population with more prevalence in school going boys than girls.[26] In the United States, for the ≥20 years age group, hyperopia is the least common refractive error while it was the most common refractive error with astigmatism in the ≥60 years age group.[27] In Polish immigrants in Chicago, a study found that hyperopia is a more common refractive error overall and in the >45 years age group.[28]
In the 6 to 15 years age group in Cameroon, hyperopia is the most common refractive error.[29] Hyperopia is unrelated to posterior subcapsular cataracts but is related to incident nuclear and cortical cataract.[30] The intelligence quotient score in hyperopic patients was lower than that of myopic in a study conducted in the United Kingdom.[31] A higher prevalence of hyperopia is seen in people living in rural areas compared to urban areas.[32] Hyperopia is more prevalent in families with a history of accommodative esotropia and hyperopia, and 20% of the hyperopic individuals in infancy develop strabismus.[5]
Pathophysiology
The axial shortening of the eyeball or decreased converging potential of the cornea or crystalline lens due to flattening are common responsible factors for simple hyperopia. Congenital or acquired absence of the crystalline lens resulting in loss of converging capacity leads to the pathological hyperopia. Senile changes in cortical lens fibers lead to change in the refractive index causing index hyperopia. Paralysis of accommodation (by cycloplegic drugs) and loss of accommodation due to complete third nerve palsy or internal ophthalmoplegia cause functional hyperopia.[22][21]
Accommodation is a dynamic factor in controlling the state of refraction, specifically in hyperopia. Depending on the accommodation, manifest hyperopia may subdivide into:
- Absolute hyperopia, which can not be overcome by accommodative effort
- When a patient can not see 20/20 without glasses, absolute hyperopia is denoted by the weakest plus lens with which the patient can see 20/20.
- Facultative hyperopia which can be overcome by accommodation
The manifest hyperopia is the sum of absolute and facultative hyperopia. Clinically, it is measured by the strongest plus (or convex) lens with which the patient can still maintain the maximum vision (20/20).
Latent hyperopia is due to the inherent ciliary muscle tone. Usually, the magnitude of latent hyperopia is 1D, but it is higher at an early age and gradually decreases as age progresses. Cycloplegic agents like atropine unmask this condition. This latent hyperopia causes asthenopic symptoms without dimness of distant vision. Cycloplegia is a must to elicit the amount of latent hyperopia in children.
- Total hyperopia = Latent hyperopia + manifest hyperopia
- Manifest hyperopia = Absolute hyperopia + facultative hyperopia
History and Physical
Depending on the age of presentation and the degree of hyperopia, clinical presentation varies from no symptom to a wide range of complaints. Age is an important factor not only due to the ability to express but also the accommodative effort of the patient.
Asymptomatic: The patient's inherent ciliary muscle tone and accommodative effort can overcome some degree of hyperopia without creating any difficulty.
Symptomatic:
Deviation of eyes (noted by the parents)[33][34]: Parents sometimes note deviation of either or both eyes (simultaneous or alternative) in very young children with hyperopia. The commonest type is an inward deviation (esotropia).
Asthenopia: With total accommodative effort, the patient's hyperopia is corrected here. In these cases, asthenopia (i.e., varied amount of tiredness of eyes with localized frontal/frontotemporal headache) is a very common symptom due to prolonged accommodative effort. Sometimes it may be associated with photophobia and watering. Usually, asthenopia increases after near activity of long-duration.
Dimness of vision: There will be dimness of vision if existing hyperopia is not corrected with total accommodative effort. In hyperopia, infinity focuses beyond the neurosensory retina. So, nearer objects focus behind the retina. Characteristically the defective vision affects near vision more than distant vision. Thus, the objects appear more blurred as they come closer. This dimness may (small amount of hyperopia) or may not (a large amount of hyperopia or after 40 years of age when accommodation is lost) be associated with asthenopia. A significant difference in uncorrected hyperopia may predispose the worse eye to develop amblyopia. Uncorrected hyperopia of both the eyes may develop ametropic amblyopia bilaterally.
Sudden blurring of vision (intermittent)[35]: Due to prolonged accommodative effort (e.g., during reading), there may be an episode of accommodative spasm leading to a sudden blurring of vision, often termed as pseudomyopia. It is commonly found in teenagers with uncorrected hyperopia.
Recurrent Internal/External Hordeolum or Conjunctivitis: The exact mechanism of the recurrent eyelid or conjunctival inflammation is unrevealed. The proposed theory is the frequent rubbing of the eyes with unhygienic hands, which leads to recurrent inflammatory episodes. Proper treatment of recurrent inflammation helps to get good best-corrected visual acuity in the future and vice-versa.[36]
A sensation of Crossed Eye: Prolonged sustained accommodation is sometimes felt as a crossed eye. The patient may complain that the eyes are crossing each other (due to convergence) without any diplopia. Ignorance towards this symptom in the pre-school age group may lead to amblyopia in the future.[37]
Premature Presbyopia: As the age progresses, obvious receding of the near point becomes apparent. It occurs earlier (earlier than the 40s) in hyperope than emmetrope. The progressive accommodation loss with age is more frustrating to the patient as the near vision was already compromised earlier due to hyperopia.
Evaluation
A thorough clinical evaluation not only helps to diagnose hyperopia but also points out significant related events.
Visual Acuity: It depends on the age at presentation, degree of accommodation, and status of the crystalline lens and posterior segment. In children, the vision may not be affected due to a full accommodative effort to focus the image on the retina. As the status of the eye is usually not complicated by cataract and retinal diseases in children, distant vision may be affected with high hyperopia, which can not be corrected by the full range of accommodation. There may be a gross reduction of vision if amblyopia develops in unilateral or bilateral high hyperopia cases. Near vision may also be diminished in children with high hyperopia or in aged where accommodation is partially or fully lost. An age-related hyperopic shift can make near vision more difficult.
Diffuse light examination: Eyeball and cornea may appear smaller, especially in high hyperopia and in unilateral cases. Sometimes it may simulate enophthalmos. Anterior chamber (both central and peripheral) appears shallow, and the angle of the anterior chamber may appear narrow with a small pupil. Gonioscopy is indicated in all cases to rule out possible angle closure. Cortical cataracts may also be present in aged persons or young individuals with diabetes.
Fundoscopy: Fundoscopy reveals a small optic disc with a very small cup. Disc margins become blurred with overcrowding of blood vessels, sometimes termed as "pseudopapillitis" or "pseudo-papilledema" if bilateral. Choroidal folds may be present.[38][39] An increased reflex of retina named as "shot-silk appearance" is seen along with crowding of the nerve fiber layer.[40]
Examination of Latent / Manifest strabismus: In children having uncorrected hyperopia for a long duration, strabismus may be present: latent (-phoria) or manifest (-tropia). Extraocular movement is usually full in all directions of gazes.
Breaking the fusion by Alternate Cover-Uncover test with occluder and asking the patient to focus at a point light source may reveal latent strabismus, mainly in children and young. Alternate and sequential shifting of the occluder to cover either eye is done. The presence of latent strabismus is confirmed if the covered eye deviates, which is noted during refixation when uncovered.
In manifest strabismus, the deviated eye takes fixation after occlusion of the fellow orthophoric eye. Manifest strabismus must be examined by Hirschberg corneal reflex test (HCRT) and with a prism bar to note the degree of deviation. HCRT reveals the approximate degree of deviation i.e., corneal light reflex on the pupillary border and the corneal border corresponds to approximately 15 degrees and 45 degrees of deviation, respectively. Prisms can also serve to keep the apex towards the deviation to bring the corneal light reflex at the center and note that deviation in prism-diopter.
Retinoscopy/Refraction: In the modern era of automated refraction, retinoscopy has its importance while examining young children and bed-ridden patients. It's a good practice to evaluate a child with suspected any refractive error with cycloplegic retinoscopy[41] from a 1-meter distance as routine. Cycloplegia abolishes ciliary muscle tone and accommodation to reveal the actual status of refraction. With a streak retinoscope, under cycloplegia, different powered-spherical lenses are used to reach a neutralization point (full illumination of the fundus with no movement) both in the horizontal and vertical axis.
Existing refractive error (in horizontal/vertical axis) = Retinoscopic findings (in both axis) - the value of distance in meter (1 for 1 meter, 1.5 for 2/3rd meter) - tonus allowance for the particular cycloplegic drug (For atropine ointment 1% it is 1, cyclopentolate drops 1% it is 0.75, and for homatropine drops 2% it is 0.5)
If both the axis and the power (after deduction) are equal, then that is considered as the spherical refractive power of the eye. If it is unequal, then the extra power (in one axis) is denoted as the astigmatic power in the other axis.
Treatment / Management
Aim:
- Provide good rehabilitation with proper refractive correction
- Prevention of amblyopia
- Prevention of development of strabismus
- Prevention of recurrent eyelid infection and conjunctivitis
1. Optical correction: Biconvex lenses (plus) are recommended to converge the light rays on the neurosensory retina. Basic principles of prescribing glasses are:
- The amount of total hyperopia should always be elicited by cycloplegic retinoscopy, especially in children.
- Symptomatic patients and young children should always be treated with proper refractive correction.
- Young children should be prescribed full hyperopic correction gradual tapering during school age.
- The maximum accepted plus power with a clear vision (20/20) should be prescribed.
- A gradual increase in hyperopic correction from the comfortably accepted power in school-aged children may be necessary as full correction may produce blurring at distant. A short course of cycloplegic agents may improve the acceptance of hyperopic correction.
- Accommodative convergence should be treated with full hyperopic correction. Developing/developed amblyopia should undergo a thorough evaluation, and full hyperopic correction with occlusion therapy should be prescribed.
- Hyperopic children should have a reevaluation every 3 to 6 months.
American Academy of Ophthalmology (AAO) has given a guideline about when to prescribe glasses in hyperopia in young children.[42]
Dependent factors are
- Iso-metropia (similar refractive error in both eyes)
- Anisometropia (dis-similar errors of refraction between eyes)
- Presence/absence of strabismus.
Isoametropic eyes without tropia should be prescribed glasses if the hyperopia is at least:[42]
- Age under 1-year: +6D
- Age of 1-year to less than 2 years: +5D
- Age of 2-year to less than 3 years: +4.50D
- Age of 3-year to less than 4 years: +3.50D
Cases having hyperopic iso-metropia with esotropia need to be prescribed glasses when the minimum refraction is at least:
- Age less than 2 years: +2D
- Age of 2-year to less than 4 years: +1.50D
Hyperopic anisometropia without strabismus should be corrected if it is at least:[42]
- Age under 1-year: +2.50D
- Age of 1-year to less than 2 years: +2D
- Age of 2-year to less than 4 years: +1.50D
Glasses and contact lenses can be used as rehabilitation devices. Contact lenses are usually prescribed in cases of unilateral hyperopia or a large difference in hyperopia between eyes.
2. Surgical treatment: Preoperative stable refraction (cycloplegic and manifest)[43] is must at least in three successive checkups one year apart. Counseling and discussion about possible outcomes and side effects are very important. Before any surgical intervention, every patient should undergo
- Slit-lamp biomicroscopy: to rule out allergic blepharoconjunctivitis and dry eye syndromes[44]
- Refraction testing (cycloplegic and manual) both distant and near vision
- Corneal thickness and topography, wavefront analysis[45]
- Intraocular pressure
- Pupil size estimation in dark and mesopic conditions
- Fundoscopy (B2)
So, all the investigations are of utmost importance before any sort of kerato-refractive surgery.
- Incisional refractive procedure;
- Hexagonal keratotomy: It was done in the past to treat low to moderate degrees of hyperopia previously.[46] Now it is obsolete.
- Lamellar refractive procedure: hyperopic keratomileusis of Barraquer: It is of historical importance and basis of modern laser in-situ keratomileusis (LASIK) procedure.
- Laser-based refractive procedures:
- Thermal laser keratoplasty: Thallium-holmium-chromium (THC): yttrium aluminum garnet (YAG) laser is used to create a contraction of the collagen matrix of the stroma of the cornea in eight areas of the optical zone with pulse energies of 159-199 milli-joule.[47] This makes a mechanical constriction which steepens the cornea. This can also be done by creating 12 pairs of coagulation spots by Diode laser, which is also a safe procedure.[48] The diode laser is also used in associated presbyopia cases.[48] It is a good option in cases of iatrogenic hyperopia after LASIK in myopia and photorefractive keratectomy in myopia.[49][50] Compared to LASIK, it is slow in achieving stable refraction with less predictability to correct astigmatism.[51] Overcorrection may be present in the early postoperative period, but no significant surprise is noted in long term followups.[50]
(B2)
Currently, this procedure has approval for a temporary reduction of hyperopia of +0.75 to +2.50 diopters with ≤ +/- 0.75 diopters of astigmatism by the United States Food and Drug Administration (USFDA). The patients should be of at least 40 years of age. The refraction should be documented to be stable for the prior six months (change of ≤ 0.50D in spherical and cylindrical components of the manifest refraction).
- Hyperopic photorefractive keratectomy (PRK): It's a lengthy procedure by which a large burn is created with an excited dimer (excimer) laser. The cornea becomes dry and dehydrated, and epithelial healing is delayed.[52] Decentration is another significant problem. After initial encouraging results, regression may take place. It may be combined with phototherapeutic keratectomy(PTK) to counter hyperopic shift.[53] It has shown initial instability but no significant change in refractive power thereafter, with peripheral haze and Salzman-like changes without any ectatic changes.[54] It is equally efficacious compared to LASIK for hyperopia.[55] It is a safe procedure to correct mild to moderate degree of hyperopia.[56] It can give a reasonably good result in the treatment of presbyopia.[57] USFDA approved excimer (excited dimer) laser systems for this procedure.
- Hyperopic LASIK: Patient selection depends on stable preoperative refractions, corneal thickness, intraocular pressure, pupil size, fundoscopy, and corneal topography. It can correct up to 6 diopters of hyperopia. The procedure is performed under topical anesthesia, and it can also be performed with pilocarpine-induced miosis on same day cycloplegia.[58] Before the flap elevation by microkeratome, the cornea can be marked. This marking may have a risk of development of marker-pen induced chemical diffuse lamellar keratitis (DLK).[59] The creation of the flap can be by microkeratome or femtosecond laser (Femto laser). Femto laser is an infrared laser of 1053 nm wavelength. Femto laser has better predictability of flap thickness with the advantages of fewer postoperative higher-order aberrations, better contrast sensitivity, longer tear film breakup time.[60] Different USFDA approved machines for LASIK in hyperopia work with an excimer laser system. Manifest refraction spherical equivalent (MRSE) is calculated following the preoperative refraction of the patient. A large number of them are used to correct associated astigmatism also. Most importantly, hyperopia with myopic astigmatism is also taken care of by a few of the systems. Different LASIK machines can correct different ranges of hyperopia. Few of the machines are dedicated to those eyes with spherical power, less than cylindrical power. Argon-fluoride (193 nanometers) excimer laser is used to ablate the corneal bed after the elevation of the flap by microkeratome. Intraocular pressure is raised artificially to maintain the hold during the elevation of the epithelial flap. After ablation, the epithelial flap is repositioned. It is safe and also effective in all degrees of hyperopia, especially in high hyperopia.[61] Monofocal and varifocal LASIK: both can be safely used in presbyopia.[62] Epithelial remodeling is suspected to be responsible for masking the extra advantages of the varifocal laser.[62] Better predictability and lower regression are making the use of Mitomycin C 0.02% (MMC) essential though further long term followup studies are needed.[63] Femtosecond laser-assisted surgeries with MMC 0.02% gives better refractive outcomes and less number of re-treatments.[64] Compared to the pupil-centered procedure, vertex-centered gives better visual outcomes in temporally decentred pupil cases, though in other cases, it is equivalent.[57][65] Postoperative patching or dark glass, along with topical broadspectrum antibiotics are prescribed. (A1)
Contraindications include chronic eye or corneal diseases, systemic illness, unstable refraction, dry eyes, contact lens intolerance, chronic pain syndromes, pregnancy, and lactation.[66]
Complications of LASIK include refractive regression, postoperative dry eyes, halos during night driving, and diminished corneal sensations.[67][66] In high hyperopia cases and those with associated astigmatism, spherical aberrations, coma, and trefoil are significantly increased.[68] Flap striae, epithelial ingrowth especially in enhancement procedures, infectious (Pseudomonas, Mycobacterium chelonae) keratitis, noninfectious (diffuse lamellar) keratitis, and interface fluid are not uncommon.[69][70][71][72][59][73] DLK is treated with intensive topical steroids with successful results.[59] Diminished corneal sensations can have treatment with cyclosporine (0.05%) drops for 3-months.[74] (A1)
- Hyperopic laser subepithelial keratomileusis (LASEK): Here, with the help of 20% ethyl alcohol for 60 seconds, the epithelium of the cornea is loosened and separated. Then stromal ablation is performed by the excimer laser. Sometimes it is augmented by 0.02% mitomycin c after corneal ablation.[75] It may be helpful in children to correct hyperopia with or without amblyopia (off label use).[76] Though postoperative refraction status, contrast sensitivity, topography data shows better outcomes in lasek[77] along with complications such as aberrations, ectasia, flap related complications are less than LASIK, but more postoperative pain, slow recovery keep it a little bit behind from PRK and epiploic LASIK.[78]
- Hyperopic epiploic LASIK (EPI-LASIK): It is similar to LASEK, but here epikeratome is used to raise the epithelial flap, not alcohol. So, alcohol-related toxicities are negated.
- Hyperopic customized-LASIK (C-LASIK): It is either topography or wavefront-guided ablation procedure to correct associated astigmatism and aberrations, with wavefront-guided procedures having better contrast sensitivity and less glare.[79] Quality of vision is improved compared to other procedures, but Snellen's visual acuity, the refractive status remain comparable.[80] (A1)
- Other refractive procedures:
- Conductive keratoplasty (CK): USFDA approved this for the treatment of mild-moderate hyperopia with minimal astigmatism for a temporary basis. After two years, it was approved for presbyopia with an endpoint of -1.00 to -2.00 diopters for the nondominant eye. It is a radiofrequency energy-based procedure to create shrinkage of stromal collagen. It increases the converging power of the cornea.[81] It is an excellent surgical option for hyperopia[82][83] and presbyopia[84]. A keratoplasty of 90-um diameter and 450-um length is used to produce ablation.[81] A variable number of ablations for 0.6-seconds each in 6-mm, 7-mm, and 8-mm circular zone in the cornea is done depending on the refractive error. It is a minimally invasive and safe procedure but not effective in high hyperopia. Recurrent corneal erosions, mild iritis, iris burn, endothelial cell loss[85], and rarely partial or full-thickness corneal injury can take place. Predictable and stable refractive status is achievable in low to moderate hyperopia.[86]
- Small incision lenticule extraction (SMILE): It is the recent advancement in the management of hyperopia. It was first performed in donor eyes where concave lenticule extraction was performed, and interlamellar concave gap air bubbles were noted.[87] It is a safe procedure for hyperopia, even in higher degrees.[88] It is comparable to LASIK for hyperopia in effectiveness and safety[89] with the induction of similar spherical aberration[90]. Intraoperative complications such as opaque bubble formation, suction loss are mainly related to less experience of the surgeon. Postoperative keratitis, ectasia, dry eye are not uncommon after SMILE.[91]
(B3)
- Intraocular Procedures: Phakic intraocular lenses[92], where a new intraocular lens is implanted anterior to the crystalline lens, is a good option. Due to the shallowness of intraocular spaces in hyperopia, pupillary block, oval pupil, and cataract formation is not uncommon.[93] The refractive lens exchange is another option for a high degree of hyperopia or where corneal procedures are contraindicated and associated with cataract cases.[94] Intraocular surgery has its own complications e.g., corneal decompensation, rhegmatogenous retinal detachment, hyphema, and uveitis.[95] (B2)
- Management of angle-closure related to hyperopia: Hyperopia is one of the risk factors of angle-closure disease.[96] Patients with symptomatic or suspected angle-closure or patients with a positive family history should undergo tonometry, gonioscopy, perimetry along with newer diagnostic modalities like Anterior Segment Optical Coherence Tomography (AS-OCT), Ultrasound Biomicroscopy, and OCT scan of optic nerve/retinal nerve fiber layer.[97] Laser peripheral iridotomy (LPI) is a safe procedure in every stage of the angle-closure disease.[98] Cataract surgery or clear lens extraction is also a very effective procedure and showed superiority to LPI in a study.[98]
Differential Diagnosis
Differential diagnosis of hyperopia includes:
- Nanophthalmos - Structurally normal, but the eye is smaller in size.[99]
- Microphthalmos - Smaller in size with structurally abnormal eye and sometimes associated with systemic involvement.[99]
- Posterior microphthalmos: Microphthalmos involves the posterior segment only. The dimensions of the anterior segment are normal.
- Micro-cornea, enophthalmos
- Partial ptosis simulating a small eyeball
- Papilledema
- Retinal edema or serous or exudative elevation of the retina
- Orbital tumors causing anterior displacement of the posterior part of the eyeball
- Hypoglycemia
- Presbyopia
Pertinent Studies and Ongoing Trials
SMILE in hyperopia is a promising area to explore. Compared to LASIK, LASEK, CK, and PRK, SMILE can be a better option for high hyperopic cases with stable postoperative refraction. Newer technologies of wavefront analysis and correction of aberrations and treatment of associated astigmatism will give better optical satisfaction to the patient. Preparation and correction of aberrations in a customized manner with C-LASIK is also an upcoming procedure to deal with aberrations. Refractive lens exchange and phakic intraocular lenses are other options for the management of hyperopia.
Staging
AR Augsburger, in his book, classified hyperopia into three stages or degrees, which the convention followed to date and also by the American Optometric Association (AOA).
- Low hyperopia i.e. +2.00 diopters (D) or less.
- Moderate hyperopia i.e.+2.25 to +5.00 D.
- High hyperopia i.e., +5.00 D.
Prognosis
Good Prognostic factors:
- The prognosis of hyperopia is good if early diagnosis and treatment are started. It is of utmost importance in the pre-school age group. Cycloplegic refraction, followed by post-cycloplegic refraction, is mandatory for them. In suspected amblyopia, proper amblyopia management carries a good prognosis. If not done early, it may lead to amblyopia and permanent visual decline.[100]
- Proper preoperative preparation and timely intervention carry a good prognosis.
Bad prognostic factor:
Complications
- Amblyopia: Stimulus deprivation or anisometropic amblyopia may take place if there is no timely correction.[100] Proper refractive correction, orthoptic exercises are needed to treat this amblyopia.
- Squint: Convergent strabismus[101] is not very uncommon in developing children with uncorrected hyperopia. The squinted eye becomes more stimulus deprived gradually.
- Angle-closure disease: Hyperopia is a predisposing condition to develop angle-closure disease.[96]
- Anterior ischaemic optic neuropathy (AION): Hyperopia is a risk factor of the development of AION (non-arteritic).[102]
- Retinal vein occlusion: Though few studies denied its association with hyperopia, branch retinal vein occlusion might be more likely to be associated with hyperopia than central vein occlusion.[103]
- Age-related macular degeneration (ARMD): ARMD may be associated with hyperopia.
- Central serous chorioretinopathy (CSCR): Hyperopic eyes may be more prone to develop CSCR.[104]
- Uveal effusion syndrome: Posterior microphthalmos with hyperopia predisposes the eye to develop uveal effusion.[105]
- Nanophthalmos/posterior microphthalmos: Serous retinal detachment, pre-retinal folds with macular cysts, macular folds, and thickening of the fovea and retinal pigment epithelium are common retinal features of nanophthalmos or posterior microphthalmos.[106]
Postoperative and Rehabilitation Care
Rehabilitation in the form of glasses or contact lenses is the most effective and cost-effective care for hyperopia. Constant use of glasses, along with amblyopia therapy (occlusion/orthoptic exercises), is the mainstay of management of developing refractive amblyopia. It can also prevent strabismus development.
Keratorefractive surgeries are one of the most important solutions for hyperopia. After laser or radiofrequency ablation based surgical procedures,
- Dark glasses (LASIK) or eye patching (CK) are given.
- Topical broad-spectrum antibiotics for 5 to 7 days or more if needed, along with artificial tear substitutes[107].
- Immediate postoperative rubbing to be avoided.
- Topical cyclosporine A after surgery can treat dry eyes.[108]
- Follow up at regular intervals to evaluate refraction, flap condition, and diagnose complications.
Consultations
A very good optometrist/ophthalmic assistant should be on the team for proper refractive rehabilitation and amblyopia therapy. For the assessment and treatment of associated anterior chamber and posterior segment complications, specialists should be consulted.
Deterrence and Patient Education
Patient and parental health education is most important to prevent complications.[109]
- Maternal smoking during pregnancy positively correlates with hyperopia in the child.[12]
- Parental education and counseling are very important, not only to early diagnosis and treatment of hyperopia but also to prevent strabismus and amblyopia development.
- Proper use of glasses, along with patching and exercises for amblyopia treatment, requires the active involvement of the parents.
- Regular follow-ups with an eye examination and refraction testing are essential.
Pearls and Other Issues
No definite cause of hyperopia is identified to date. Genetic predisposition, along with family history, plays an important role. Asthenopic symptoms must be emphasized and evaluated in children. Hyperopic children are usually less intelligent compared to myopic. Their social, mental, and educational development depends upon their vision.
The commonest treatment option is rehabilitation with glasses. Regular follow-ups with cycloplegic refraction are mandatory. Adult hyperopic should be treated with glasses or cataract surgery if the cataract is the cause. Unilateral/bilateral aphakia should be treated with amblyopia therapy with glasses or contact lenses immediately followed by intraocular lens implantation.
Enhancing Healthcare Team Outcomes
Our main aim is to give good vision and optimal binocular vision to the patients. For children with refractive error only, proper refractive correction is indicated. If amblyopia development is suspected, orthoptic exercises and patching of eyes are used. Good interdepartmental coordination is necessary for regular followups and proper rehabilitation.
The development of the visual system is often affected by strabismus and amblyopia, which needs cycloplegic refraction and followups. After proper preparation and counseling, it can be corrected with refractive surgery. Adult with hyperopia needs refractive support along with complication evaluation by gonioscopy and fundoscopy.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Castagno VD,Fassa AG,Vilela MA,Meucci RD,Resende DP, Moderate hyperopia prevalence and associated factors among elementary school students. Ciencia [PubMed PMID: 26017947]
McCullough SJ,Doyle L,Saunders KJ, Intra- and inter- examiner repeatability of cycloplegic retinoscopy among young children. Ophthalmic [PubMed PMID: 28030881]
Semeraro F,Forbice E,Nascimbeni G,Cillino S,Bonfiglio VME,Filippelli ME,Bartollino S,Costagliola C, Ocular Refraction at Birth and Its Development During the First Year of Life in a Large Cohort of Babies in a Single Center in Northern Italy. Frontiers in pediatrics. 2019; [PubMed PMID: 32083036]
Yahya AN,Sharanjeet-Kaur S,Akhir SM, Distribution of Refractive Errors among Healthy Infants and Young Children between the Age of 6 to 36 Months in Kuala Lumpur, Malaysia-A Pilot Study. International journal of environmental research and public health. 2019 Nov 27; [PubMed PMID: 31783494]
Level 3 (low-level) evidenceTarczy-Hornoch K, The epidemiology of early childhood hyperopia. Optometry and vision science : official publication of the American Academy of Optometry. 2007 Feb; [PubMed PMID: 17299341]
Lin PW,Chang HW,Lai IC,Teng MC, Visual outcomes after spectacles treatment in children with bilateral high refractive amblyopia. Clinical [PubMed PMID: 27426739]
Laiginhas R,Figueiredo L,Rothwell R,Geraldes R,Chibante J,Ferreira CC, Long-term refractive outcomes in children with early diagnosis of moderate to high hyperopia. Strabismus. 2020 Apr 22; [PubMed PMID: 32316817]
Strang NC,Schmid KL,Carney LG, Hyperopia is predominantly axial in nature. Current eye research. 1998 Apr; [PubMed PMID: 9561829]
Harb EN,Wildsoet CF, Origins of Refractive Errors: Environmental and Genetic Factors. Annual review of vision science. 2019 Sep 15; [PubMed PMID: 31525141]
Stingl CS,Jackson-Cook C,Couser NL, Ocular Findings in the 16p11.2 Microdeletion Syndrome: A Case Report and Literature Review. Case reports in pediatrics. 2020; [PubMed PMID: 32373379]
Level 3 (low-level) evidenceXiao X,Sun W,Ouyang J,Li S,Jia X,Tan Z,Hejtmancik JF,Zhang Q, Novel truncation mutations in MYRF cause autosomal dominant high hyperopia mapped to 11p12-q13.3. Human genetics. 2019 Oct; [PubMed PMID: 31172260]
Jiang X,Tarczy-Hornoch K,Stram D,Katz J,Friedman DS,Tielsch JM,Matsumura S,Saw SM,Mitchell P,Rose KA,Cotter SA,Varma R, Prevalence, Characteristics, and Risk Factors of Moderate or High Hyperopia among Multiethnic Children 6 to 72 Months of Age: A Pooled Analysis of Individual Participant Data. Ophthalmology. 2019 Jul; [PubMed PMID: 30822446]
Borish IM, Aphakia: perceptual and refractive problems of spectacle correction. Journal of the American Optometric Association. 1983 Aug; [PubMed PMID: 6619475]
Wiemer NG,Eekhoff EM,Simsek S,Heine RJ,Ringens PJ,Polak BC,Dubbelman M, The effect of acute hyperglycemia on retinal thickness and ocular refraction in healthy subjects. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2008 May; [PubMed PMID: 18219490]
Kaštelan S,Gverović-Antunica A,Pelčić G,Gotovac M,Marković I,Kasun B, Refractive Changes Associated with Diabetes Mellitus. Seminars in ophthalmology. 2018; [PubMed PMID: 30199309]
Saito Y,Ohmi G,Kinoshita S,Nakamura Y,Ogawa K,Harino S,Okada M, Transient hyperopia with lens swelling at initial therapy in diabetes. The British journal of ophthalmology. 1993 Mar; [PubMed PMID: 8457504]
Level 3 (low-level) evidenceMarshall-Goebel K,Damani R,Bershad EM, Brain Physiological Response and Adaptation During Spaceflight. Neurosurgery. 2019 Nov 1; [PubMed PMID: 31215633]
Phasukkijwatana N,Freund KB,Dolz-Marco R,Al-Sheikh M,Keane PA,Egan CA,Randhawa S,Stewart JM,Liu Q,Hunyor AP,Kreiger A,Nagiel A,Lalane R,Rahimi M,Lee WK,Jampol LM,Sarraf D, PERIPAPILLARY PACHYCHOROID SYNDROME. Retina (Philadelphia, Pa.). 2018 Sep; [PubMed PMID: 29135799]
Gao FJ,Hu FY,Xu P,Qi YH,Li JK,Zhang YJ,Chen F,Chang Q,Song F,Shen SM,Xu GZ,Wu JH, Expanding the clinical and genetic spectrum of Heimler syndrome. Orphanet journal of rare diseases. 2019 Dec 12; [PubMed PMID: 31831025]
Level 2 (mid-level) evidenceBoynton JR,Pheasant TR,Johnson BL,Levin DB,Streeten BW, Ocular findings in Kenny's syndrome. Archives of ophthalmology (Chicago, Ill. : 1960). 1979 May; [PubMed PMID: 444124]
Level 3 (low-level) evidenceJung JJ,Baek SH,Kim US, A case of lorazepam (Ativan)-induced accommodation paresis. Eye (London, England). 2012 Apr; [PubMed PMID: 22193881]
Level 3 (low-level) evidenceHu YY,Wu JF,Lu TL,Wu H,Sun W,Wang XR,Bi HS,Jonas JB, Effect of cycloplegia on the refractive status of children: the Shandong children eye study. PloS one. 2015; [PubMed PMID: 25658329]
Level 2 (mid-level) evidenceRiise N,Lindberg BR,Kulseth MA,Fredwall SO,Lundby R,Estensen ME,Drolsum L,Merckoll E,Krohg-Sørensen K,Paus B, Clinical diagnosis of Larsen syndrome, Stickler syndrome and Loeys-Dietz syndrome in a 19-year old male: a case report. BMC medical genetics. 2018 Aug 31; [PubMed PMID: 30170566]
Level 3 (low-level) evidenceIp JM,Robaei D,Kifley A,Wang JJ,Rose KA,Mitchell P, Prevalence of hyperopia and associations with eye findings in 6- and 12-year-olds. Ophthalmology. 2008 Apr; [PubMed PMID: 17664011]
Level 2 (mid-level) evidenceDandona R,Dandona L,Naduvilath TJ,Srinivas M,McCarty CA,Rao GN, Refractive errors in an urban population in Southern India: the Andhra Pradesh Eye Disease Study. Investigative ophthalmology [PubMed PMID: 10549640]
Sheeladevi S,Seelam B,Nukella PB,Modi A,Ali R,Keay L, Prevalence of refractive errors in children in India: a systematic review. Clinical [PubMed PMID: 29682791]
Level 1 (high-level) evidenceVitale S,Ellwein L,Cotch MF,Ferris FL 3rd,Sperduto R, Prevalence of refractive error in the United States, 1999-2004. Archives of ophthalmology (Chicago, Ill. : 1960). 2008 Aug; [PubMed PMID: 18695106]
Allison CL, Proportion of refractive errors in a Polish immigrant population in Chicago. Optometry and vision science : official publication of the American Academy of Optometry. 2010 Aug; [PubMed PMID: 20526223]
Eballe AO,Bella LA,Owono D,Mbome S,Mvogo CE, [Eye disease in children aged 6 to 15 years: a hospital-based study in Yaounde]. Sante (Montrouge, France). 2009 Apr-Jun; [PubMed PMID: 20031512]
Wong TY,Klein BE,Klein R,Tomany SC,Lee KE, Refractive errors and incident cataracts: the Beaver Dam Eye Study. Investigative ophthalmology [PubMed PMID: 11381046]
Level 2 (mid-level) evidenceWilliams C,Miller LL,Gazzard G,Saw SM, A comparison of measures of reading and intelligence as risk factors for the development of myopia in a UK cohort of children. The British journal of ophthalmology. 2008 Aug; [PubMed PMID: 18567647]
Padhye AS,Khandekar R,Dharmadhikari S,Dole K,Gogate P,Deshpande M, Prevalence of uncorrected refractive error and other eye problems among urban and rural school children. Middle East African journal of ophthalmology. 2009 Apr; [PubMed PMID: 20142964]
Lembo A,Serafino M,Strologo MD,Saunders RA,Trivedi RH,Villani E,Nucci P, Accommodative esotropia: the state of the art. International ophthalmology. 2019 Feb; [PubMed PMID: 29332227]
Cho YA,Yi S,Kim SW, Clinical evaluation of cessation of hyperopia in 123 children with accommodative esotropia treated with glasses for best corrected vision. Acta ophthalmologica. 2009 Aug; [PubMed PMID: 18759801]
Level 2 (mid-level) evidenceRutstein RP,Marsh-Tootle W, Acquired unilateral visual loss attributed to an accommodative spasm. Optometry and vision science : official publication of the American Academy of Optometry. 2001 Jul; [PubMed PMID: 11503937]
Level 3 (low-level) evidenceJones SM,Weinstein JM,Cumberland P,Klein N,Nischal KK, Visual outcome and corneal changes in children with chronic blepharokeratoconjunctivitis. Ophthalmology. 2007 Dec [PubMed PMID: 18054641]
Level 2 (mid-level) evidenceZimmerman DR,Ben-Eli H,Moore B,Toledano M,Stein-Zamir C,Gordon-Shaag A, Evidence-based preschool-age vision screening: health policy considerations. Israel journal of health policy research. 2019 Sep 12 [PubMed PMID: 31514739]
Fried M,Meyer-Schwickerath G,Koch A, Excessive hypermetropia: review and case report documented by echography. Annals of ophthalmology. 1982 Jan; [PubMed PMID: 7125435]
Level 3 (low-level) evidenceGutteridge IF, Optic nerve drusen and pseudopapilledema. American journal of optometry and physiological optics. 1981 Aug; [PubMed PMID: 6169281]
Level 3 (low-level) evidenceWatson WS, Note on a Hitherto Undescribed Appearance of the Retina, or [PubMed PMID: 20750790]
Saini V,Raina UK,Gupta A,Goyal JL,Anjum R,Saini P,Gupta SK,Sharma P, Comparison of Plusoptix S12R photoscreener with cycloplegic retinoscopy and autorefraction in pediatric age group. Indian journal of ophthalmology. 2019 Oct; [PubMed PMID: 31546479]
Wallace DK,Morse CL,Melia M,Sprunger DT,Repka MX,Lee KA,Christiansen SP, Pediatric Eye Evaluations Preferred Practice Pattern®: I. Vision Screening in the Primary Care and Community Setting; II. Comprehensive Ophthalmic Examination. Ophthalmology. 2018 Jan [PubMed PMID: 29108745]
Frings A,Steinberg J,Druchkiv V,Linke SJ,Katz T, Role of preoperative cycloplegic refraction in LASIK treatment of hyperopia. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2016 Jul; [PubMed PMID: 26935202]
Yanchenko SV,Malyshev AV,Sakhnov SN,Fedotova NV,Orekhova OY, [Eye lid hygiene in chronic allergic blepharoconjunctivitis patients before laser refractive surgery]. Vestnik oftalmologii. 2016; [PubMed PMID: 27911432]
Stonecipher K,Parrish J,Stonecipher M, Comparing wavefront-optimized, wavefront-guided and topography-guided laser vision correction: clinical outcomes using an objective decision tree. Current opinion in ophthalmology. 2018 Jul; [PubMed PMID: 29787391]
Level 2 (mid-level) evidence[Study on improved utilization of the maternal health record]., Noda Y,Kajikuri Y,Ashimura K,Sakaetani N,Inoue K,, Josanpu zasshi = The Japanese journal for midwife, 1979 Jan [PubMed PMID: 8871863]
Level 2 (mid-level) evidenceKoch DD,Abarca A,Villarreal R,Menefee R,Kohnen T,Vassiliadis A,Berry M, Hyperopia correction by noncontact holmium:YAG laser thermal keratoplasty. Clinical study with two-year follow-up. Ophthalmology. 1996 May; [PubMed PMID: 8637681]
Rehany U,Landa E, Diode laser thermal keratoplasty to correct hyperopia. Journal of refractive surgery (Thorofare, N.J. : 1995). 2004 Jan-Feb; [PubMed PMID: 14763472]
Gozum N,Ayoglu B,Gezer A,Goker S,Gucukoglu A, Holmium laser thermal keratoplasty for hyperopia in eyes overcorrected with laser in situ keratomileusis for myopia. Journal of refractive surgery (Thorofare, N.J. : 1995). 2004 May-Jun; [PubMed PMID: 15188903]
Eggink CA,Meurs P,Bardak Y,Deutman AF, Holmium laser thermal keratoplasty for hyperopia and astigmatism after photorefractive keratectomy. Journal of refractive surgery (Thorofare, N.J. : 1995). 2000 May-Jun; [PubMed PMID: 10832980]
Hill JC, Treatment of simple hyperopia: comparison of laser in situ keratomileusis and laser thermal keratoplasty. Journal of cataract and refractive surgery. 2003 May; [PubMed PMID: 12781275]
Level 2 (mid-level) evidence[Establishment of professional practice in midwifery. Specialization of delivery]., Fujisawa Y,, Josanpu zasshi = The Japanese journal for midwife, 1979 Jan [PubMed PMID: 21926568]
Level 2 (mid-level) evidenceAmano S,Kashiwabuchi K,Sakisaka T,Inoue K,Toda I,Tsubota K, Efficacy of Hyperopic Photorefractive Keratectomy Simultaneously Performed With Phototherapeutic Keratectomy for Decreasing Hyperopic Shift. Cornea. 2016 Aug; [PubMed PMID: 27158808]
Wagh VK,Dave R,O'Brart DP,Lim WS,Patel P,Tam C,Lee J,Marshall J, Eighteen-year follow-up of hyperopic photorefractive keratectomy. Journal of cataract and refractive surgery. 2016 Feb; [PubMed PMID: 27026451]
Settas G,Settas C,Minos E,Yeung IY, Photorefractive keratectomy (PRK) versus laser assisted in situ keratomileusis (LASIK) for hyperopia correction. The Cochrane database of systematic reviews. 2012 Jun 13; [PubMed PMID: 22696365]
Level 1 (high-level) evidenceKim TI,Alió Del Barrio JL,Wilkins M,Cochener B,Ang M, Refractive surgery. Lancet (London, England). 2019 May 18; [PubMed PMID: 31106754]
Vinciguerra P,Nizzola GM,Bailo G,Nizzola F,Ascari A,Epstein D, Excimer laser photorefractive keratectomy for presbyopia: 24-month follow-up in three eyes. Journal of refractive surgery (Thorofare, N.J. : 1995). 1998 Jan-Feb; [PubMed PMID: 9531083]
Ozulken K,Yuksel E,Uzel MM, Effect of topical pilocarpine on refractive surgery outcomes. International ophthalmology. 2020 Mar; [PubMed PMID: 31758508]
Rosman M,Chua WH,Tseng PS,Wee TL,Chan WK, Diffuse lamellar keratitis after laser in situ keratomileusis associated with surgical marker pens. Journal of cataract and refractive surgery. 2008 Jun; [PubMed PMID: 18499004]
[Education and activities of midwifery practice in England and the United States. Midwifery education in the United States. (1)]., Shindo Y,, Josanpu zasshi = The Japanese journal for midwife, 1979 Jan [PubMed PMID: 26309880]
Demir G,Sucu ME,Yıldırım Y,Tülü B,Özveren M,Kepez Yıldız B,Yaşa D,Karaağaç Günaydın Z,Demirok A, Long-term assessment of visual and refractive outcomes of laser in situ keratomileusis for hyperopia using the AMARIS{sup}®{/sup} 750S Excimer laser. Journal francais d'ophtalmologie. 2019 Sep; [PubMed PMID: 31130390]
Taneri S,Kiessler S,Rost A,Verma S,Arba-Mosquera S,Dick HB, Varifocal Versus Monofocal LASIK in Presbyopic Hyperopic Eyes. Journal of refractive surgery (Thorofare, N.J. : 1995). 2019 Jul 1; [PubMed PMID: 31298726]
Moawad EM,Abd Elghany AA,Gab-Alla AA,Elbassiouny OM,Badawy MS, LASIK-induced corneal changes after correction of hyperopia with and without application of Mitomycin-C. BMC ophthalmology. 2019 Apr 23; [PubMed PMID: 31014283]
Garcia-Gonzalez M,Iglesias-Iglesias M,Drake Rodriguez-Casanova P,Gros-Otero J,Teus MA, Femtosecond Laser-Assisted LASIK With and Without the Adjuvant Use of Mitomycin C to Correct Hyperopia. Journal of refractive surgery (Thorofare, N.J. : 1995). 2018 Jan 1; [PubMed PMID: 29315438]
Soler V,Benito A,Soler P,Triozon C,Arné JL,Madariaga V,Artal P,Malecaze F, A randomized comparison of pupil-centered versus vertex-centered ablation in LASIK correction of hyperopia. American journal of ophthalmology. 2011 Oct; [PubMed PMID: 21726847]
Level 1 (high-level) evidenceWilkinson JM,Cozine EW,Kahn AR, Refractive Eye Surgery: Helping Patients Make Informed Decisions About LASIK. American family physician. 2017 May 15; [PubMed PMID: 28671403]
Yan MK,Chang JS,Chan TC, Refractive regression after laser in situ keratomileusis. Clinical [PubMed PMID: 29700964]
Biscevic A,Pidro A,Pjano MA,Grisevic S,Ziga N,Bohac M, Lasik as a Solution for High Hypermetropia. Medical archives (Sarajevo, Bosnia and Herzegovina). 2019 Jun; [PubMed PMID: 31402804]
Mohamed TA,Hoffman RS,Fine IH,Packer M, Post-laser assisted in situ keratomileusis epithelial ingrowth and its relation to pretreatment refractive error. Cornea. 2011 May; [PubMed PMID: 21598428]
Level 2 (mid-level) evidenceWallerstein A,Gauvin M,Adiguzel E,Singh H,Gupta V,Harissi-Dagher M,Cohen M, Clinically significant laser in situ keratomileusis flap striae. Journal of cataract and refractive surgery. 2017 Dec; [PubMed PMID: 29335096]
Ferrer C,Rodriguez-Prats JL,Abad JL,Claramonte P,Alió JL,Signes-Soler I, Pseudomonas keratitis 4 years after laser in situ keratomileusis. Optometry and vision science : official publication of the American Academy of Optometry. 2011 Oct; [PubMed PMID: 21666521]
Level 3 (low-level) evidenceKohnen T,Schöpfer D,Bühren J,Hunfeld KP, [Flap Amputation in Mycobacterium chelonae Keratitis after Laser-in-situ Keratomileusis (LASIK)]. Klinische Monatsblatter fur Augenheilkunde. 2003 Sep; [PubMed PMID: 14533063]
Level 3 (low-level) evidenceLyle WA,Jin GJ,Jin Y, Interface fluid after laser in situ keratomileusis. Journal of refractive surgery (Thorofare, N.J. : 1995). 2003 Jul-Aug; [PubMed PMID: 12899478]
Level 3 (low-level) evidencePeyman GA,Sanders DR,Batlle JF,Féliz R,Cabrera G, Cyclosporine 0.05% ophthalmic preparation to aid recovery from loss of corneal sensitivity after LASIK. Journal of refractive surgery (Thorofare, N.J. : 1995). 2008 Apr; [PubMed PMID: 18500081]
Level 1 (high-level) evidenceArranz-Marquez E,Katsanos A,Kozobolis VP,Konstas AGP,Teus MA, A Critical Overview of the Biological Effects of Mitomycin C Application on the Cornea Following Refractive Surgery. Advances in therapy. 2019 Apr; [PubMed PMID: 30859502]
Level 3 (low-level) evidenceAstle WF,Huang PT,Ereifej I,Paszuk A, Laser-assisted subepithelial keratectomy for bilateral hyperopia and hyperopic anisometropic amblyopia in children: one-year outcomes. Journal of cataract and refractive surgery. 2010 Feb; [PubMed PMID: 20152607]
Level 2 (mid-level) evidenceScerrati E, Laser in situ keratomileusis vs. laser epithelial keratomileusis (LASIK vs. LASEK). Journal of refractive surgery (Thorofare, N.J. : 1995). 2001 Mar-Apr; [PubMed PMID: 11316025]
Reilly CD,Panday V,Lazos V,Mittelstaedt BR, PRK vs LASEK vs Epi-LASIK: a comparison of corneal haze, postoperative pain and visual recovery in moderate to high myopia. Nepalese journal of ophthalmology : a biannual peer-reviewed academic journal of the Nepal Ophthalmic Society : NEPJOPH. 2010 Jul-Dec; [PubMed PMID: 21505525]
Level 2 (mid-level) evidenceToda I,Ide T,Fukumoto T,Tsubota K, Visual Outcomes After LASIK Using Topography-Guided vs Wavefront-Guided Customized Ablation Systems. Journal of refractive surgery (Thorofare, N.J. : 1995). 2016 Nov 1; [PubMed PMID: 27824375]
Kim TI,Yang SJ,Tchah H, Bilateral comparison of wavefront-guided versus conventional laser in situ keratomileusis with Bausch and Lomb Zyoptix. Journal of refractive surgery (Thorofare, N.J. : 1995). 2004 Sep-Oct; [PubMed PMID: 15523953]
Level 1 (high-level) evidenceMcDonald MB, Conductive keratoplasty: a radiofrequency-based technique for the correction of hyperopia. Transactions of the American Ophthalmological Society. 2005; [PubMed PMID: 17057816]
Alió JL,Ramzy MI,Galal A,Claramonte PJ, Conductive keratoplasty for the correction of residual hyperopia after LASIK. Journal of refractive surgery (Thorofare, N.J. : 1995). 2005 Nov-Dec; [PubMed PMID: 16329361]
Pallikaris lG,Naoumidi TL,Panagopoulou SI,Alegakis AK,Astyrakakis NI, Conductive keratoplasty for low to moderate hyperopia: 1-year results. Journal of refractive surgery (Thorofare, N.J. : 1995). 2003 Sep-Oct; [PubMed PMID: 14518738]
Stahl JE, Conductive keratoplasty for presbyopia: 1-year results. Journal of refractive surgery (Thorofare, N.J. : 1995). 2006 Feb; [PubMed PMID: 16523831]
Çakir H,Genç S,Güler E, 360-Degree Iris Burns Following Conductive Keratoplasty. Journal of refractive surgery (Thorofare, N.J. : 1995). 2016 Nov 1; [PubMed PMID: 27824383]
Pallikaris IG,Naoumidi TL,Astyrakakis NI, Long-term results of conductive keratoplasty for low to moderate hyperopia. Journal of cataract and refractive surgery. 2005 Aug; [PubMed PMID: 16129286]
Zhao J,Miao H,Han T,Shen Y,Zhao Y,Sun L,Zhou X, A Pilot Study of SMILE for Hyperopia: Corneal Morphology and Surface Characteristics of Concave Lenticules in Human Donor Eyes. Journal of refractive surgery (Thorofare, N.J. : 1995). 2016 Oct 1; [PubMed PMID: 27722761]
Level 3 (low-level) evidencePradhan KR,Reinstein DZ,Carp GI,Archer TJ,Dhungana P, Small Incision Lenticule Extraction (SMILE) for Hyperopia: 12-Month Refractive and Visual Outcomes. Journal of refractive surgery (Thorofare, N.J. : 1995). 2019 Jul 1; [PubMed PMID: 31298724]
Moshirfar M,Bruner CD,Skanchy DF,Shah T, Hyperopic small-incision lenticule extraction. Current opinion in ophthalmology. 2019 Jul; [PubMed PMID: 31033739]
Level 3 (low-level) evidenceReinstein DZ,Pradhan KR,Carp GI,Archer TJ,Gobbe M,Sekundo W,Khan R,Dhungana P, Small Incision Lenticule Extraction (SMILE) for Hyperopia: Optical Zone Diameter and Spherical Aberration Induction. Journal of refractive surgery (Thorofare, N.J. : 1995). 2017 Jun 1; [PubMed PMID: 28586496]
Krueger RR,Meister CS, A review of small incision lenticule extraction complications. Current opinion in ophthalmology. 2018 Jul; [PubMed PMID: 29782336]
Level 3 (low-level) evidenceKocová H,Vlková E,Michalcová L,Motyka O, Implantation of posterior chamber phakic intraocular lens for myopia and hyperopia - long-term clinical outcomes. Journal francais d'ophtalmologie. 2017 Mar; [PubMed PMID: 28291554]
Level 2 (mid-level) evidenceLeccisotti A, Angle-supported phakic intraocular lenses in hyperopia. Journal of cataract and refractive surgery. 2005 Aug [PubMed PMID: 16129298]
Alió JL,Grzybowski A,Romaniuk D, Refractive lens exchange in modern practice: when and when not to do it? Eye and vision (London, England). 2014; [PubMed PMID: 26605356]
Sayman Muslubas IB,Kandemir B,Aydin Oral AY,Kugu S,Dastan M, Long-term vision-threatening complications of phakic intraocular lens implantation for high myopia. International journal of ophthalmology. 2014 [PubMed PMID: 24790887]
Jonas JB,Aung T,Bourne RR,Bron AM,Ritch R,Panda-Jonas S, Glaucoma. Lancet (London, England). 2017 Nov 11; [PubMed PMID: 28577860]
Kwon J,Sung KR,Han S,Moon YJ,Shin JW, Subclassification of Primary Angle Closure Using Anterior Segment Optical Coherence Tomography and Ultrasound Biomicroscopic Parameters. Ophthalmology. 2017 Jul [PubMed PMID: 28385302]
[Professionally speaking: a plan for a health center and the role of the midwife]., Yamanishi M,, Josanpu zasshi = The Japanese journal for midwife, 1979 Feb [PubMed PMID: 29482864]
[Education and activities of widwives in the United Sates and England. Education of widwives in the United States]., Shindo Y,, Josanpu zasshi = The Japanese journal for midwife, 1979 Feb [PubMed PMID: 29862063]
Ahmed N,Fashner J, Eye Conditions in Infants and Children: Amblyopia and Strabismus. FP essentials. 2019 Sep; [PubMed PMID: 31454213]
Fashner J. Eye Conditions in Infants and Children: Myopia and Hyperopia. FP essentials. 2019 Sep:484():23-27 [PubMed PMID: 31454214]
Pahor D,Gracner B, [Hyperopia as a risk factor in patients with non-arteritic anterior ischaemic optic neuropathy]. Klinische Monatsblatter fur Augenheilkunde. 2008 Dec; [PubMed PMID: 19085788]
Level 2 (mid-level) evidenceAppiah AP,Trempe CL, Differences in contributory factors among hemicentral, central, and branch retinal vein occlusions. Ophthalmology. 1989 Mar; [PubMed PMID: 2710528]
Level 2 (mid-level) evidence[Topics on technics of resuscitation of newborn infants]., Shimada N,, Josanpu zasshi = The Japanese journal for midwife, 1979 Feb [PubMed PMID: 26949648]
Zor KR,Küçük E,Günaydın NT,Önder F, Ocular findings in posterior microphthalmos. Saudi journal of ophthalmology : official journal of the Saudi Ophthalmological Society. 2019 Jan-Mar [PubMed PMID: 30930662]
Xiao H,Liu X,Zhong YM,Guo XX,Mi L,Li M, [Fundus features of nanophthalmos analyzed by optical coherence tomography]. [Zhonghua yan ke za zhi] Chinese journal of ophthalmology. 2013 Dec [PubMed PMID: 24499692]
Level 2 (mid-level) evidenceAlbietz JM,McLennan SG,Lenton LM, Ocular surface management of photorefractive keratectomy and laser in situ keratomileusis. Journal of refractive surgery (Thorofare, N.J. : 1995). 2003 Nov-Dec; [PubMed PMID: 14640428]
Level 2 (mid-level) evidenceTorricelli AA,Santhiago MR,Wilson SE, Topical cyclosporine a treatment in corneal refractive surgery and patients with dry eye. Journal of refractive surgery (Thorofare, N.J. : 1995). 2014 Aug; [PubMed PMID: 25325897]
Level 2 (mid-level) evidenceMocanu V,Horhat R, Prevalence and Risk Factors of Amblyopia among Refractive Errors in an Eastern European Population. Medicina (Kaunas, Lithuania). 2018 Mar 20 [PubMed PMID: 30344237]