Anatomy, Head and Neck, Palatine Tonsil (Faucial Tonsils)
Anatomy, Head and Neck, Palatine Tonsil (Faucial Tonsils)
Introduction
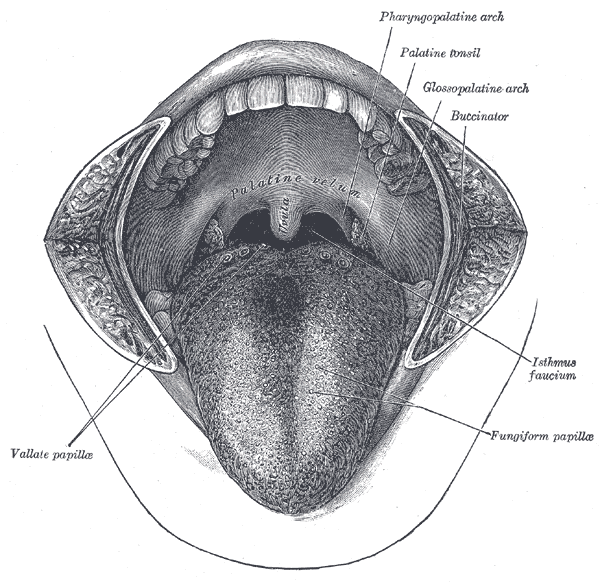
The palatine (or faucial) tonsils, commonly referred to as tonsils, are bundles of lymphatic tissue located in the lateral oropharynx. They sit in the isthmus of the fauces, bordered anteriorly by the palatoglossal arch and posteriorly by the palatopharyngeal arch. Both of these mucous membrane-enclosed anatomic borders are continuous with the roof of the oral cavity and are formed by the palatoglossus muscle and palatopharyngeus muscle, respectively. The palatine tonsils also serve as a component of Waldeyer's ring which in addition to the palatine tonsils consists of the adenoids, tubal tonsil, and lingual tonsil.[1] Typically, when inflammation and infection are absent, these structures have a pink color.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Located bilaterally on the lateral aspect of the oropharynx and near the entrance of the gastrointestinal and upper respiratory tracts, the palatine tonsils come into contact with various inhaled or ingested pathogens and other materials that may gain exposure to the body through the mouth. As a mucosa-associated lymphoid tissue, the palatine tonsils serve as the primary lymphatic tissue of the oropharynx.[2] This tissue houses B cells that can go through the maturation process and produce all isotypes of immunoglobulins (IgA, IgD, IgE, IgG, and IgM).[2] Recent reseacrh demonstrates that, like the thymus, the tonsils have been shown to express T cell developmental intermediates that resemble those found in the thymus and bone marrow.[3]
Palatine tonsils consist of approximately 15 crypts, which provide a large internal surface area. The follicular germinal center, mantle zones, extrafollicular area, and reticular crypt epithelium play a key role in the immunological regulation of this mucosa-associated lymphoid tissue.[4] Histologic analysis nhas demonstrated crypts lined with non-keratinized stratified squamous cells.
In humans, the initial portion known as the tonsillar epithelium gets exposed to the external (pharyngeal) environment. Due to their strategic location, this tissue frequently demands more blood to assist in immune responses to common illnesses like viral upper respiratory infections. Tonsils also have specialized surface antigen capture cells called M cells that allow for the uptake of antigens produced by pathogens.[5] The M cells transmit the information that a foreign pathogen is present and an immune cascade then begins.
Embryology
The development of the palatine tonsils begins during the fourteenth week of gestation.[6] Mononuclear wandering cells soon migrate into the mesenchyme. Crypts proliferate into the connective tissue and are infiltrated by T-lymphocytes at week 16.[6] The developing palatine tonsils are considered the first B-cell regions in fetal lymphoid tissue.[6] This series of developmental steps for the palatine tonsils arises from the 2nd pharyngeal pouch.
Blood Supply and Lymphatics
Vascular Supply
The blood supply of the palatine tonsils derives from vasculature that branches off several major vessels, all are primarily tributaries of the external carotid artery. The dorsal lingual artery, ascending palatine artery, the tonsillar branch of the facial artery, ascending pharyngeal artery, and lesser palatine artery all provide oxygen and other nutrients to the palatine tonsils.
Venous drainage of the palatine tonsils occurs by the peritonsillar plexus of veins. This plexus drains into the pharyngeal and lingual veins, and these veins ultimately drain into the internal jugular vein.
Lymphatics
The palatine tonsils drain to the jugulodigastric node, a node of the deep cervical lymph nodes, located inferior to the angle of the mandible.
Nerves
The innervation of the palatine tonsils is provided by the lesser palatine nerve which arises from the maxillary division of the trigeminal nerve and the tonsillar branches of the glossopharyngeal nerve.
Surgical Considerations
Tonsillectomy is a surgical procedure where the palatine tonsils are excised from the tonsillar fossa.
Indications for Tonsillectomy
Infectious
Tonsillectomy should be considered in patients who[7][8][7]:
- Have had recurrent throat infections with seven documented cases in the last year
- A minimum of five documented throat infections in each of the previous 2 years
- A minimum of three documented throat infections in each of the last 3 years
- All patients who meet one of the above criteria must also have a temperature greater than 100.9°F (38.3°C), cervical adenopathy, tonsillar exudate, or a positive culture for group A beta-hemolytic streptococcus
- Recurrent or chronic pharyngotonsillitis, peritonsillar abscesses, tonsillar stones, and halitosis are other circumstances where tonsillectomy may be the recommended course of action
Hyperplastic/Neoplastic
Indications for tonsillectomy include a variety of hyperplastic and neoplastic processes. Some of these include hyperplasia of adenotonsillar tissue associated with obstructive sleep apnea, failure to thrive, or abnormal dentofacial growth.[8] Concern for a malignant process would be another indication for tonsillectomy.[8]
Potential Complications associated with Tonsillectomy
The most frequent complication of a tonsillectomy is post-operative hemorrhage, which is responsible for the majority of post-tonsillectomy fatalities. Significant risk factors for post-operative hemorrhage include older age, a history of chronic tonsillitis, excessive intraoperative blood loss and elevated mean arterial pressure.[9]
The glossopharyngeal nerve innervates the posterior one-third of the tongue and provides general sensation and taste. The nerve travels past the palatine tonsils and has the potential to be stretched or injured during a tonsillectomy. Consequences of this injury could manifest as a reduction or loss of general sensation or taste to the posterior third of the tongue.[10]
Clinical Significance
Due to their anatomic location near the entrances of the respiratory and gastrointestinal tracts, the palatine tonsils get exposed to a myriad of exogenous foreign materials. The function of this tissue as a secondary lymphoid organ seems to inherently provide a method of prolonged exposure to infectious material or other antigens. These two properties may have a role in the infection risk which the palatine tonsils seem predisposed. At this time, it is still unclear if tonsillar hypertrophy results from persistent infection.
Peritonsillar abscesses have been shown to be the leading cause of deep neck infections in the adult population.[11] This condition is found primarily in young adults and is made on a primarily clinical basis. Common symptoms of this condition include fever, sore throat, trismus, dysphagia, peritonsillar bulge, uvular deviation, and a "hot potato" voice. The treatment consists of incision and drainage, antibiotics, and supportive therapy. Corticosteroid use has assisted in reducing symptoms and decreasing healing time.[11] If a peritonsillar abscess is not diagnosed and treated promptly, complications such as aspiration, airway obstruction and extension into the retropharyngeal space can occur.[11]
Media
(Click Image to Enlarge)
References
Masieri S, Trabattoni D, Incorvaia C, De Luca MC, Dell'Albani I, Leo G, Frati F. A role for Waldeyer's ring in immunological response to allergens. Current medical research and opinion. 2014 Feb:30(2):203-5. doi: 10.1185/03007995.2013.855185. Epub 2013 Oct 31 [PubMed PMID: 24127824]
Level 3 (low-level) evidenceJović M, Avramović V, Vlahović P, Savić V, Veličkov A, Petrović V. Ultrastructure of the human palatine tonsil and its functional significance. Romanian journal of morphology and embryology = Revue roumaine de morphologie et embryologie. 2015:56(2):371-7 [PubMed PMID: 26193201]
McClory S,Hughes T,Freud AG,Briercheck EL,Martin C,Trimboli AJ,Yu J,Zhang X,Leone G,Nuovo G,Caligiuri MA, Evidence for a stepwise program of extrathymic T cell development within the human tonsil. The Journal of clinical investigation. 2012 Apr; [PubMed PMID: 22378041]
Tang X, Hori S, Osamura RY, Tsutsumi Y. Reticular crypt epithelium and intra-epithelial lymphoid cells in the hyperplastic human palatine tonsil: an immunohistochemical analysis. Pathology international. 1995 Jan:45(1):34-44 [PubMed PMID: 7704242]
Kato A, Hulse KE, Tan BK, Schleimer RP. B-lymphocyte lineage cells and the respiratory system. The Journal of allergy and clinical immunology. 2013 Apr:131(4):933-57; quiz 958. doi: 10.1016/j.jaci.2013.02.023. Epub [PubMed PMID: 23540615]
von Gaudecker B, Müller-Hermelink HK. The development of the human tonsilla palatina. Cell and tissue research. 1982:224(3):579-600 [PubMed PMID: 6981458]
Randel A. AAO-HNS Guidelines for Tonsillectomy in Children and Adolescents. American family physician. 2011 Sep 1:84(5):566-73 [PubMed PMID: 21888309]
Darrow DH, Siemens C. Indications for tonsillectomy and adenoidectomy. The Laryngoscope. 2002 Aug:112(8 Pt 2 Suppl 100):6-10 [PubMed PMID: 12172229]
Myssiorek D, Alvi A. Post-tonsillectomy hemorrhage: an assessment of risk factors. International journal of pediatric otorhinolaryngology. 1996 Sep:37(1):35-43 [PubMed PMID: 8884405]
Level 2 (mid-level) evidenceTrinidade A, Philpott CM. Bilateral glossopharyngeal nerve palsy following tonsillectomy: a very rare and difficult complication of a common procedure. The Journal of laryngology and otology. 2015 Apr:129(4):392-4. doi: 10.1017/S0022215115000080. Epub 2015 Feb 20 [PubMed PMID: 25697260]
Level 3 (low-level) evidenceGalioto NJ. Peritonsillar Abscess. American family physician. 2017 Apr 15:95(8):501-506 [PubMed PMID: 28409615]