Introduction
Embryogenesis is a complex process and is divided between pre-implantation, embryo, and fetal period. This process is highly susceptible to various external factors such as teratogenic drugs, alcohol, smoking, radiation, and even the lack of appropriate nutrition. Ionizing radiation way more than non-ionizing has known effects in developing fetus with fatal outcomes.
Malignancy is relatively uncommon during pregnancy, with a low incidence of 0.02 to 0.1%. The most common malignancies found are breast, skin including melanoma, gynecological (uterine, cervix, and ovarian), and hematological (Hodgkin and non-Hodgkin lymphoma (NHL)).[1] Generally, when rivaled with patients who received surgical monotherapy, survivors who underwent abdominopelvic radiation with or without surgery were more likely to have infants that were premature, low–birth weight, and even associated with perinatal mortality in few cases.[2] Various studies have demonstrated an increased risk of unfavorable pregnancy and neonatal outcomes with prior history of abdominopelvic irradiation, possibly due to radiation-induced uterine damage. Since high-dose uterine irradiation can restrict the pregnant uterus' growth and cause vascular changes that impair uterine blood flow, preterm birth, fetal growth restriction, and stillbirth are common.[3] Signorello et al. observed that infants of patients treated with high-dose radiotherapy (>5 Gy) to the uterus were at a heightened risk of preterm delivery, low birth weight, and small for gestational age when compared with offspring of patients who did not receive radiotherapy.[4] Green et al. observed that the incidence of fetal malposition, early or threatened labor, low birth weight, and prematurity were higher with elevated radiation doses.[5]
When compared to radiotherapy, chemotherapy does not appear to have harmful effects on the uterus.[6] Hence it generally has favorable pregnancy outcomes in patients treated only with chemotherapy. Those who conceived ≥one year after post-chemotherapy without radiation or ≥two years after chemotherapy with radiation displayed no elevated risks to pregnancy outcomes.[7]
Significant potential harmful effects of ionizing radiation can be summarised into four main categories:
- Pregnancy loss (miscarriage, stillbirth)
- Malformation
- Disturbances of growth or development
- Mutagenic and carcinogenic effects
While treating cancer in pregnant patients with radiotherapy, the goal is to improve the mother overall survival; however, specific considerations are vital to reduce the fetus's possible adverse implications. Earlier, the norm was to terminate the ongoing pregnancy, regardless of the trimesters. Fortunately, because of the advent of the latest developments of evidence and technology in the last two decades, we have steered away from this blanket policy. Since the 1990s, various technological and technical advancements in modern radiotherapies, such as 3D-conformal radiotherapy, intensity-modulated radiotherapy (IMRT), and volumetric modulated arc therapy, have made it possible to give high doses to the tumor while sparing the surrounding healthy tissues or organs in the vicinity, hence improving radiotherapy in terms of effectiveness and tolerability.[8] Furthermore, IMRT techniques using on-board cone-beam computed tomography have evolved to ensure a precise dose delivery.[9] The detrimental principle of all radiation is that it should be "as low as reasonably achievable" (ALARA) as the effects of radiation are linearly cumulative. In practice, even though the fetus is excluded from the direct radiation field, the fetus gets radiation leaking from the accelerator and collimator dispersions. To cut down this radiation, we use lead blocks and shields to achieve ALARA.
Childhood malignancy in the context of prenatal diagnostic and assessment X-ray was first reported by Giles et al. in 1956.[10] Their survey of childhood cancers established that the risk increased linearly with the number of films exposed. The relative risk of developing a childhood cancer-associated was significantly higher if the exposure was during the first trimester, about 2.5 times greater than the third trimester. This study became the working model of various radiation-induced teratogenesis studies. A defining study was by Kato et al., where they followed up the survivors of the Hiroshima and Nagasaki atomic bombs.[11] It was the most extensive cohort study of intrauterine radiation exposure; interestingly, only 2 cases had childhood cancer before the 14th birthday out of 1630 children exposed without a single case of leukemia.
Broadly, radiation effects are expressed as being either deterministic or stochastic.
- Deterministic effects have a cause and effect relationship such that below a certain threshold, the effect will not occur. However, once the threshold has been crossed, the effect of significance will increases linearly with every next dose. Deterministic effects on a fetus range from congenital malformations, lower intelligence quotient (IQ), mental retardation, microcephaly, various neurobehavioral dysfunctions leading to increased risk of seizures and growth retardation, fetal death, and increased cancer risk.[12] A threshold dose of 0.1Gy has been reported on several occasions. The risks are uncertain between 0.05 Gy to 0.1Gy and deemed negligible when below 0.05Gy. Pathologically, these effects occur when a large number of cells are irradiated during a critical developmental stage of organogenesis.
- The stochastic effect represents the radiation effects that may occur by chance, such as cancer induction. For this to occur, there is no threshold dose observed, and the risk manifolds in a linear-quadratic manner of the dose. Childhood cancers are primarily the result of the stochastic effect, as seen in the post-Chernobyl disaster with the increased thyroid cancer occurrence.
Ionizing radiation induces these effects by causing structural changes at the cellular and molecular levels. Non-ionizing radiation (which is not associated with medical imaging or radiotherapy) causes damage through heat transfer, such as microwave heating. Furthermore, by producing free radicals, ionizing radiation causes cellular damage by interfering with chemical bonds between molecules regulating critical cellular processes and events. This process generally leads to DNA mutation or cell death and sometimes causes damage to essential cellular enzymes. Susceptibility to radiation injury depends on the rate of cellular proliferation and differentiation of exposed tissues. Hence lymphoproliferative tissues with rapid cell turnover are the most susceptible, while nervous tissue with little or no cell turnover is the least affected.
Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Function
The American Association of Physicists in Medicine and the International Commission on Radiological Protection described guidelines for assessing the potential fetal radiation exposure during maternal radiotherapy. They recognized three possible radiation sources that need to be evaluated: first, the photon leakage from the machine head; second, the scatter and leakage from the collimators and beam modifiers; and lastly, scattered radiation emerging from the treatment beams of the volume treated within the patient. To reduce the leakage and scatter from the treatment head, beam modifiers, and collimators, lead shielding is placed on the pregnant mother's abdomen and pelvis. Shielding is possible earlier in the pregnancy, but as the gravid uterus grows, it is difficult for adequate shielding. Also, as the abdominal size increases, the distance between the field and fetus reduces, thus increasing the risk of exposure while treating supradiaphragmatic areas. In this circumstance, the fetus receives 10 to 15 times more radiation dose for the same treatment field.
The developing fetus is most sensitive to ionizing radiation harmful effects during the first 14 days post-conception. In this period, either the pregnancy withstands the radiation exposure unharmed or is resorbed, often termed as an "all or none" phenomenon.[13] However, significant consequential damage is seen when exposed during the period of organogenesis (approximately 2 to 8 weeks post-conception or 4 to 10 weeks after the last menstrual period). The embryo may sustain damage due to radiation-induced cell death leading to irregularities in cell migration and proliferation or mitotic delay. Significant sequelae of radiation-induced damage are fetal growth restriction and congenital malformations, particularly of the central nervous system seen as microcephaly and ocular abnormalities, often associated with intellectual disability. Microcephaly is the most frequently seen manifestation of radiation injury in utero.
Diagnostic radiology imaging is essential. It is noted that the risks to the pregnant woman of not having imaging or a particular procedure are far greater than the speculated potential harm to the fetus. The fetal radiation dose from various conventional radiograph examinations is below 0.01 Gy. For fluoroscopic examinations, the dose resulting from barium enema might exceed 0.01 Gy, which can be further reduced by proper pre-requisites of the procedure. For a computed tomographic (CT) scan of the pelvis and abdomen, the fetal radiation dose is typically about 0.01–0.04 Gy, well below the threshold, which never exposes the fetus to dangerous radiation levels. In general, the doses involved in diagnostic radiology are much lower than the threshold dose for deterministic effects and present no substantial risk of causing fetal death, malformation, or mental development impairment.
Effects of dose less than 0.05 Gy — Various diagnostic imaging studies typically expose the fetus to less than 0.05 Gy (50 mGy, 5 rads), which poses no evidence of an elevated risk of fetal anomalies, intellectual disability, growth retardation, or pregnancy loss.
Effects of dose more than 0.05 Gy — This is the threshold at which there is an increased risk of deterministic effects. Evidence suggests that the risk increases at doses above 0.10 Gy (100 mGy, 10 rads), significantly above 0.15 to 0.20 Gy (150 to 200 mGy, 15 to 20 rads).
Techniques for minimizing fetal exposure — A pre-imaging consultation with the radiologist to ensure that the imaging and associated data necessary for maternal diagnosis and management is accomplished at the lowest possible fetal radiation dose. Various techniques are suggested to safeguard the fetus:
- Non-abdominopelvic plain radiography – Wearing a lead apron can minimize fetal exposure from radiation scatter whenever non-abdominopelvic sites are being scanned. A combination of fast film/screen or digital radiography can be used to reduce cumulative radiation exposure. Fortunately, diagnostic radiographs of the head, neck, chest, and limbs (ones that exclude the fetus from the imaging field) produce almost no scatter to the fetus. Thus it won't adversely increase the risk of any adverse outcome.[14]
- Abdominopelvic plain radiography – When the fetus is directly in the field of view, these techniques can be employed to minimize fetal radiation exposure:
- Doing a posterior-anterior (PA) exposure reduces the fetal radiation dose by 0.02 to 0.04 mGy (0.00002 to 0.00004 Gy) when compared with the traditional anterior-posterior (AP) exposure, since the uterus is located in an anterior pelvic position.
- Shutters can be used to collimate the radiation beam to reduce scatter.
- Avoiding near uterus magnification and using grids decreases fetal exposure.
- Avoid repeat examinations
- Fluoroscopy and angiography – While doing fluoroscopic and angiographic imaging, radiation exposure can be reduced by modifying the exposure time, the number of images obtained, beam size, and imaging area.
- Nuclear medicine – Adequate maternal hydration and frequent urination reduce fetal exposure to radionuclides, which are eliminated via the urine accumulating in the maternal bladder, lying close to the gravid uterus. Most diagnostic nuclear medicine procedures use short-lived radionuclides such as technetium-99m that does not expose the fetus to large doses of radiation, keeping the exposure below 0.01 Gy.
- Computed tomography scan – When undergoing a CT scan, the estimation of fetal radiation exposure depends on several variables, such as the number, location, and thickness of slices. Doing a CT scan imaging during pregnancy while using narrow collimation and a wide pitch (i.e., the patient moves through the scanner at a faster rate) results in a slightly decreased image quality. Still, it provides a substantial reduction in radiation exposure.[14]
- Sentinel lymph node biopsy (SLNB):
- Gentilini et al. found that the dose to the affected breast was about 0.0022 Gy, to the other breast about 0.0009 Gy, and to the abdomen, about 0.00045 Gy, all far below the accepted threshold value.[15] They conclude that lymphoscintigraphy and sentinel lymph node biopsy are entirely safe during pregnancy. Even under the most adverse conditions in a phantom model study, the maximum-absorbed dose to the fetus from lymphoscintigraphy with 92.5 MBq of 99mTc sulfur colloid was 0.0043 Gy.[16] However, in a later study by Loibl et al., they recommended that sentinel lymph node biopsy be avoided because of the radioactive drug used for mapping.[17]
- NCCN (National comprehensive cancer network) May 2021 update also recommends USG, MRI, X-ray (Mammogram) with shielding and advises against PET-CT. [18]
- NCCN guidelines are unclear for SLNB as the evidence of fetal effects due to radiotracers is limited. It however recommends making individualized diagnostic decisions based on the patient's goals. [18]
Issues of Concern
Potential Consequences of Fetal Radiation
- Evidence for the harmful effects of radiation on fetal development emerges primarily from animal studies and nuclear accidents, like the Chernobyl disaster and the nuclear bombings of Hiroshima and Nagasaki. During the first 14 days post-conception, the developing embryo is at the highest risk, just before the implantation stage. A mere dose of 0.1Gy is enough to cause a pre-implantation death in mice in the zygotic stage. This occurs as an "all or none" phenomenon when a direct exposure of as little as 0.15-0.2 Gy at the pre-implantation stage can cause embryonic death. However, should the embryo survives, there is no increase in malformations, given that they are not exposed to more radiation later.
- As the embryo grows, its radiosensitivity decreases. Most malformations are observed during the brief period of organogenesis, which occurs at about the third to seventh-week post-implantation. This is when the fetus is at the highest risk of growth retardation. The brain develops between the 8th and 15th-week post-implantation. Any irradiation above the threshold during this period can result in mental impairment and impact cognitive functions. Doses below 0.1Gy are unlikely to cause cognitive impairment; however, doses higher than 0.3 Gy would affect higher functioning. Doses between 0.1Gy-0.49 Gy have been associated with a 6% incidence of mental retardation.
- The second trimester (16 to 25 weeks) has risks similar to those in the first trimester, such as malformations, growth and mental retardation, cataracts, sterility, and malignancy; however, the risk is much lower. Mental retardation was reportedly as low as 2%, even with a maximum dose of 0.49 Gy. Miller et al. reported microcephaly in 2 out of 30 children exposed to doses lower than 0.1 Gy, and 2 out of 44 children exposed to 0.1- 0.5 Gy, for pregnant mothers who had exposure post-atomic bombings during their second trimester of the period of gestation.[19]
- In the third trimester, there is the lowest risk of malformation and mental retardation. Miller reported microcephaly only in 3 out of 39 children exposed to a dose below 0.1 Gy and 1 out of 50 exposed to a dose in between 0.1 to 0.5 Gy.[19]
- There is conflicting evidence to suggest the risk of malignancy post-radiation exposure in utero. In 1975, Bithell and Stewart, in their study of childhood cancer, noticed an increase in all types of childhood malignancy post-radiation exposure in utero. They describe an increased risk of 6.4% for carcinogenesis per Gy of fetal radiation exposure.[20] Several other studies have not found such an association. However, a study investigating the sequelae of atomic bomb survivors found the risk of adult-onset malignancy was greater in children exposed to radiation than with fetal exposure.[21]
Potential Effects From Fetal Radiation Exposure
- Malformations
- The risk of malformations is higher in early pregnancy during the organogenesis period (2 to 8 weeks). For a fetus under 16 weeks of gestation, the threshold for possible prenatal radiation effects is approximately 0.10 to 0.20 Gy (100 to 200 mGy, 10 to 20 rads). This threshold is much higher after 16 weeks of gestation, at least 0.50 to 0.70 Gy (500 to 700 mGy, 50 to 70 rads). After approximately 20 to 25 weeks of gestation, which is about late in the second trimester, the fetus is relatively resistant to ionizing radiation's teratogenic effects.[22]
- Brent reported frequent malformations in neonates born to mothers who underwent abdominopelvic irradiation in which the dose exceeded 0.5 Gy.[23] Commonly occurring malformation was microcephaly with significant mental retardation. Since these studies were carried in Japan atomic bomb survivors, the neonatal malformations' curve might differ slightly in those receiving radiation in a standard clinical setting.
- Growth restriction
- Follow-up data from atomic bomb survivors exhibited a permanent physical growth restriction with increasing radiation dose, significantly above 1 Gy. This was most obvious when the exposure occurred in the first trimester. A 3% to 4% decrease in height at age 18 occurred whenever the cumulative dose was higher than 1 Gy.
- Mental retardation
- As described earlier, studies demonstrated that the risk of mental retardation and microcephaly was most evident when the exposure occurred at 8 to 15 weeks post-conception. The abnormalities were associated with aberrant neuronal development, presumably due to radiation-induced irreversible cell injury, alteration in cellular differentiation, and impaired neuronal migration. No severe intellectual disability cases were seen in newborns of survivors exposed before 8 weeks or after 25 weeks post-conception. The risk emerged as a linear function of dose exposed, with a threshold of 0.12 Gy (120 mGy, 12 rads) at 8 to 15 weeks, and 0.21 Gy (210 mGy, 21 rads) at 16 to 25 weeks.[24]
- In terms of IQ parameters, the average IQ loss at 8 to 15 weeks is approximately 25 to 31 points per Gy above 0.1 Gy (100 mGy, 10 rads) with a 40% risk of developing severe intellectual disability per Gy above 0.1 Gy. In contrast, the average IQ loss at 16 to 25 weeks was approximately 13 to 21 points per Gy at doses above 0.7 Gy (700 mGy, 70 rads) with a small 9% risk of developing severe intellectual disability per Gy above 0.7 Gy.[24]
- Carcinogenesis
- Animal experiments suggest that carcinogenic effects are commonly seen during the late stages of fetal development. Risk of having childhood cancer, particularly leukemia, increases by a factor of 1.5 to 2 when exposed to 0.01 to 0.02 Gy (10 to 20 mGy; 1 to 2 rad) levels of radiation in utero.[25]
- Similarly, when newborns are exposed to radiation of 0.01 Gy (10 mGy, 1 rad), there is an increased risk of 0.3% to 0.7% for developing a childhood malignancy, particularly leukemia (non-exposed risk: 0.2% to 0.3%). However, the evidence of carcinogenic potential at low-level radiation is debatable since non-exposed siblings of exposed children also have a higher leukemia incidence. Furthermore, there was an insignificant increased rate of carcinogenicity in children exposed in utero during the bombings of Hiroshima and Nagasaki.[26]
- Genetic mutations
- Ionizing radiation may increase the frequency of naturally occurring genetic mutations; however, it is hard to detect such small mutations when the spontaneously occurring mutations are already high at approximately 10%.
- Incidence of radiation-induced mutagenesis has been primarily studied in animal and plant models; however, only limited human data is available apart from follow-up observations of atomic bomb survivors offsprings. In consensus, ionizing radiation-induced mutagenesis has not been demonstrated in any human population at any radiation dose.
- As for non-ionizing radiation from electromagnetic waves from computers, warming blankets, heating pads, microwave communication systems, microwave ovens, cellular phones, household appliances, power lines, and airport screening devices have minimal reproductive risk. The literature concludes that there is no significant evidence for an association between a woman's exposure to such sources and fetal loss or other adverse reproductive outcomes.[27]
Clinical Significance
An insight into the radiation effects on the developing fetus serves to deliver better care to the expecting mother who is concomitantly undergoing radiotherapy. It helps curate a pre-conceptional, gestational, and post-conceptional radiotherapy planning to provide maximum care to the pregnant mother malignancy while maintaining minimum risk to fetal life.
Pre-Conceptional Considerations
- No noticeable risks of transmitting radiation-induced abnormalities to offspring from either irradiated parent's gonads before conception have been identified. Studies involving the atomic bomb survivors' children and grandchildren have not described any heritable effects after parental radiation exposure. Recent studies involving childhood cancer survivors treated with radiation therapy have also not demonstrated transmittable genetic effects on their offspring. The offsprings of fathers who receive testicular radiation do not appear to be at increased risk of adverse outcomes.[28]
- The current recommendation is that women should refrain from becoming pregnant if planning to undergo radiotherapy sessions and several months after terminating the radiation therapy. These recommendations are inferred from mice experiments that showed that mature oocytes were more radiosensitive than immature oocytes. Some authors recommend that if a pre-conception ovarian dose of over 0.5 Gy (500 mGy, 50 rads) is received, pregnancy should be delayed for at least two months. It is noteworthy that most of this is theoretical discussion imparts little value in practical terms. Usually, most patients receiving such high doses have either bulky cancer or cancer-induced significant endocrine dysfunctions, making conception difficult. They are often asked by their physicians to delay possible pregnancy.
- Adolescent girls and young women who underwent pelvic radiation are at increased risk of developing abnormalities related to pelvic vasculature leading to decreased uteroplacental perfusion when pregnant. Various radiation-induced myometrial changes like fibrosis may reduce uterine elasticity, distensibility, and volume; endometrial injury may compromise normal decidualization.[29][30][31]
- A study involving female cancer survivors compared to those who did not receive flank and uterus radiotherapy of >5 Gy showed a significantly heightened risk of having a preterm birth (50.0 versus 19.6 percent), low birth weight babies (36.2 versus 7.6 percent), and having a small for gestational age infant (18.2 versus 7.8 percent).[4] Uterine and ovarian irradiation at doses greater than 10 Gy significantly raised the risk of stillbirth and neonatal death.[3] In another study, women who underwent flank radiation therapy as a treatment regimen for unilateral Wilms' tumor were at increased risk of adverse pregnancy outcomes such as pregnancy-induced hypertension, fetal malposition, and premature labor.[5]
- It is important to note that the heightened risk for these outcomes depends explicitly on the total radiation dose, site irradiated, and the woman's age at the time of irradiation; as described earlier, that prepubertal uterus is more vulnerable.[30] It appears that women who receive radiation therapy with concurrent pregnancy are at an increased risk for adverse pregnancy outcomes; therefore, it is advisable to have comprehensive prenatal care and screening. A sonogram at approximately 18 weeks of gestation is advised to precisely evaluate the placenta, fetus, and uterus/cervix in those patients receiving radiation.
Fertility Issues in Radiotherapy Patients
Cranial or head/neck radiation can damage the hypothalamic-pituitary axis affecting patient fertility since head and neck cancers require high doses in the 40 to 70 Gy range. Direct radiation to the ovaries can also cause early ovarian failure. As described earlier, pelvis radiation may cause structural changes such as reduced uterine volume, lack of endometrial response to estrogen, or impaired uterine artery blood flow, impeding successful embryonal implantation or development.[28]
Cancer-Specific Radiotherapy Management
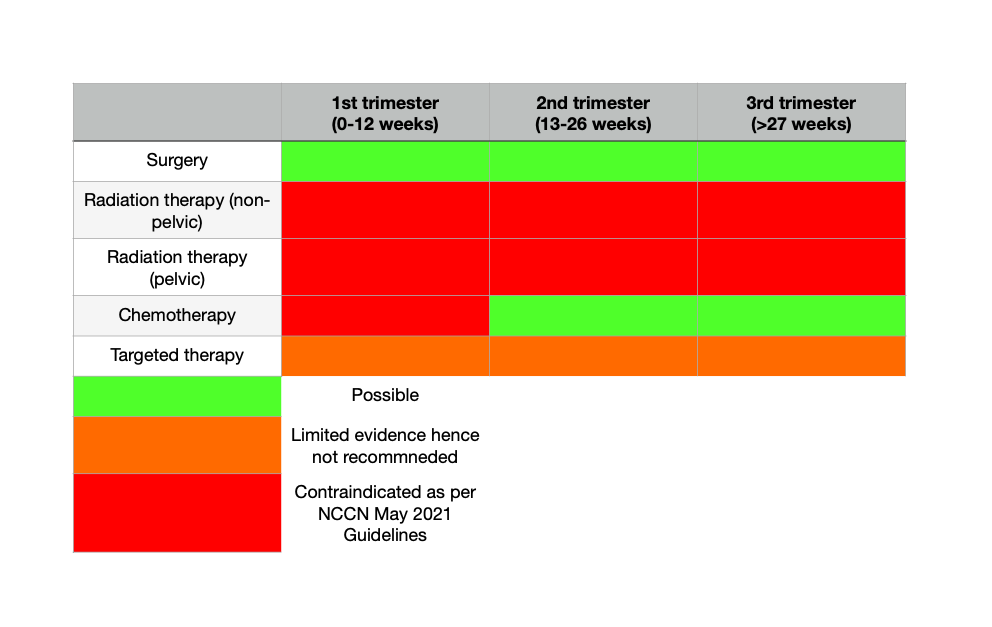
- Even though intrapartum radiation has been a longstanding issue of discussion. There is evidence from many studies as well see further demonstrating no significant fetal morbidity all while having similar patient outcomes as their non-pregnant peers. However from May 2021 updated guidelines explicitly advise against radiotherapy during pregnancy and recommends only post-partum planning for indicated radiation therapy. [18]
Breast Cancer
- The incidence of breast cancer is 1 in 10,000 pregnancies. With the women increasing age for the first pregnancy, incidence keeps rising. Increased incidence of nodal involvement is also seen with gestational breast cancer.[32]
- Primary investigations for breast cancer consist of a physical examination, mammography, breast ultrasonography (USG), and biopsy. Mammography is safe during pregnancy. Magnetic resonance imaging (MRI) can be done only if USG is non-satisfactory since there are concerns regarding using gadolinium contrast. A core biopsy is recommended over a fine needle aspiration since hormonal changes are frequent in pregnancy, so fine needle aspiration can lead to false-positive and false-negative breast tissue results.
- Investigation for staging should be limited to a chest X-ray (CXR) with appropriate shielding, USG liver, and a non-contrast skeletal MRI. A positron emission tomographic (PET) scan should be avoided.
- Delaying radical radiotherapy is commonly advocated by multidisciplinary teams until the end of the postpartum period; however, surgery and chemotherapy are invariably advised starting in the second trimester.
- When considered, adjuvant radiotherapy is usually administered as a hypofractionated dose of 40.5 Gy in 15 fractions to the whole breast and chest wall over three weeks. Radiotherapy is also administered to the supraclavicular fossa if there is a high risk of spread (for example, if metastatic deposits are found in 4 or more axillary lymph nodes).[18]
- A typical boost dose of 10–16 Gy in 4–8 fractions to the tumor bed is recommended if there is an elevated risk of recurrence.
- Palliative radiotherapy can be considered for controlling symptoms in cases where there is imminent skin involvement. There are various regimes; the most commonly used one is 36 Gy in 6 fractions, two fractions each week.
- During breast irradiation, the most critical factors determining the fetal dose are the field size and distance from the radiation field. Prominent studies outline pregnancy outcomes with ongoing radiotherapy:
- Kourinou et al. calculated the fetal exposure for breast cancer radiotherapy using anthropomorphic phantoms in pregnant patients during the first, second, and third trimester.[33] For every trimester, the dose was calculated at three different anatomical levels: upper, middle, and lower, to resemble the expanding pregnant uterus throughout the trimester. They found a total dose exposed throughout the entire pregnancy in between .039 Gy and .248 Gy. They also concluded that properly placed 3-5 cms thick lead shielding should be used, and the beam angles and modifiers should be regulated to ensure the lowest dose. The exposed dose barely exceeded .10 Gy at the upper level of the second trimester. Hence, exposure dose is of low risk, especially in the late second and third trimester, when the risk of malformations is far lower.
- Antypas et al., while treating a 45 yr-old patient with 46 Gy in 20 fractions with six megavolts tangential fields, found her to be pregnant during the second week of her treatment.[34] She was continually irradiated during the 2nd and 6th week of gestation. Fetal doses were estimated utilizing both in vivo and phantom set-up with thermoluminescence dosimeters and an ionization chamber. No shielding and no wedges or lead blocks were used for reducing scattered radiation. It was later estimated that the fetus was exposed to a dose of 0.39 Gy. A healthy baby was delivered at term through standard vaginal delivery without complications.
- The first trimester is unsafe due to known incidences of severe malformations and mental retardation. During the third trimester, the grown fetus in a growing gravid uterus is also at risk of increased dose due to the reduced distance between the treatment field and the gravid uterus. Hence the fetal exposure increases with the gestational stage as the distance between the radiation field edge and uterine fundus narrows by around a centimeter per week. Thus, it is recommended to evaluate the expected change during radiotherapy while calculating the fetal dose.[35] Also, note that using physical wedges during tangential breast irradiation can significantly escalate scattering and should therefore be avoided. Physical wedges are ordinarily used to improve dose uniformity to the target volume.
- Post-treatment breastfeeding should not be discouraged, except for from the irradiated breast. Most women who have had breast irradiation can produce milk from the affected breast. Still, the amount of milk produced may be less than that of the unaffected breast, especially if the lumpectomy site is in the vicinity of the areolar complex or if many ducts were transected.[36]
- Even if breast milk is produced, breastfeeding from the irradiated breast is not recommended because of fear of developing painful mastitis.
Gynecological Malignancies
- Managing gynecological malignancies superimposed with ongoing pregnancy is more complicated than breast cancer, especially if the disease has advanced to stages IIB-IVA. In non-pregnant patients, radiation therapy and simultaneous cisplatin chemotherapy are the recommended standards of care. Postponing definitive chemotherapy and radiotherapy with or without any pretreatment lymphadenectomy can severely affect overall cancer control and the mother's ultimate survival. Patients diagnosed earlier in pregnancy or if pregnancy occurred mid-treatment present a significant challenge. In practice, women diagnosed before attaining week 20 of gestation are recommended to terminate the pregnancy and undergo definitive cancer treatment. Pregnancy termination is a rather appropriate intervention before initiating radiotherapy for many reasons, principally for the patient psychological benefit.
Cervical Cancer
- The incidence of abnormal cervical cytology in pregnancy is fairly common, as seen in 1 to 5 women in every 100 pregnancies. However, the incidence of cervical cancer in pregnancy is low at 1 to 12 per 10,000 pregnancies.[37][38] Evaluating nodal status determined consequent treatment. Histological analysis can be tricky due to the hormonal fluctuations in pregnancy. Sometimes decidual cells can mimic atypia.
- For diagnosis, using colposcopy and biopsy is deemed safe during pregnancy. Staging is possible using a pelvic MRI without contrast. CXR and USG liver can also be utilized. PET scans are contraindicated.
- Laparoscopic lymphadenectomy is safe until 20 weeks of gestation for assessing lymph node status. However, Alouini et al. demonstrated no maternal or fetal complications while performing laparoscopic lymphadenectomies on eight pregnant women between 12 and 32 weeks of gestation.[39] Favero et al. also did lymphadenectomies on 18 patients between 6 and 23 weeks of gestation without any complications such as switching procedure to laparotomy.[40]
- Treatment depends on the stage of the disease, lymph node involvement status, and histological subtype. Most cervical cancers are diagnosed during pregnancy at stage 1, where it is limited to the cervix. For stage 1a (depth of stromal invasion <5 mm and extension <7 mm), treatment choices include either postponing treatment until fetal maturity or radical trachelectomy (if there are no involved lymph nodes). Trachelectomy can be successfully carried out on tumors <2 cm, as seen in stage 1b1. The European guidelines recommend either trachelectomy or neoadjuvant chemotherapy for stage 1b1 tumors to limit tumor progression, while the French guidelines recommend delaying treatment but with close monitoring.[41][42]
- For locally advanced stages, including stage 1B2 tumors (tumors greater than 4 cm), recommended treatment involves radical radiotherapy for 5.5 weeks with 50.4 Gy in 28 fractions with simultaneous chemotherapy followed by intracavity brachytherapy. Such high radiation doses imply that therapeutic radiotherapy and pregnancy are incompatible.
- Some studies have reported neoadjuvant chemotherapy followed by delayed surgery or radiotherapy postpartum, but their implication in mainstream cancer management is debatable. The safest option is to terminate the pregnancy and proceed with definitive treatment. In a few instances where the tumor was too large and complicated to terminate the pregnancy surgically, radiotherapy was administered during the pregnancy, resulting in spontaneous pregnancy termination.[43]
Endometrial Cancer
- Endometrial cancer incidence in pregnancy is infrequent and is usually discovered at delivery or while doing evacuation of conception products after a spontaneous miscarriage.
- Diagnosis requires a pelvic MRI without contrast, abdominal USG, and CXR. Histological diagnosis is not feasible during pregnancy.
- Definitive treatment includes a total abdominal hysterectomy irrespective of adjuvant radiotherapy, making the treatment incompatible with pregnancy. Infrequently, primary radiotherapy is administered if the patient is unable to undergo surgery.
- Like in cervical cancer, high therapeutic dose radiotherapy would not be possible without inflicting harmful consequences to the fetus. Invariably, the patient and team would need to decide on postponing the treatment or terminating the pregnancy.
Vulvar Cancer
- Vulvar intraepithelial neoplasia is commonly known to occur during pregnancy. It can be treated with a few topical treatments and surgery.
- The role of radiotherapy is not defined. In a rare instance, if either a primary or adjuvant radiotherapy is required, it would not be feasible during pregnancy. It would need to be delayed until the delivery of the fetus.
Ovarian Cancer
- Ovarian tumor incidence in pregnancy is relatively low at 2.4 to 5.7%, and approximately 5% are malignant.[44]
- Diagnosis includes a serum cancer antigen 125 assay, a pelvic/lower abdomen USG, and a biopsy. For screening, an abdominopelvic MRI and CXR are indicated.
- The mainstay of the treatment involves chemotherapy and surgery with limited radiotherapy use if at all.
Lymphoma
- The introduction of newer and better effective systemic therapy and numerous clinical trials has shown promising results. Currently, the standard treatment of lymphoma comprises chemotherapy with or without involved field (smaller volume, lower dose) radiotherapy. Typical radiation doses in the adjuvant regimens range from 20 to 30 Gy.
- Only in selective stages, such as low grade I lymphomas or lymphocyte-predominant Hodgkin lymphoma, radiation monotherapy can be considered.
- Combination chemotherapy for lymphomas has been administered during pregnancy with reasonably safe and effective outcomes, especially when administered in the second and third trimesters.
- Consensus prevails that a delay of even a few weeks in definitive radiation therapy does not impact overall survival.
Non-Hodgkin Lymphoma
- NHL comprises approximately 5-6% of all cancers diagnosed during pregnancy.
- Radiation therapy has a pivotal role in treating NHL lymphomas, including stage I and II low grade, intermediate-grade, or indolent B-cell NHL, which happens to be particularly radiosensitive. In practice, standard treatment options are primary radiotherapy in combination with immunotherapy for lasting remissions.
- Interestingly, NHL diagnosed during pregnancy tends to be more aggressive.[45]
- Patients who either have aggressive NHL or with extensive disease burden present a therapeutic challenge as delaying therapy risks the patient while administering systemic therapy endangers the fetus. In such circumstances, depending on the gestation period, disease site, and staging, the pros of active treatment should be weighed against delaying treatment until post-partum. With low doses administered (25 to 30 Gy) and often in small fields, treatment may be possible with uneventful effects on the fetus.
- If fetal dose calculations are significant, avoiding radiotherapy during pregnancy is the most judicious decision.[46][47]
Hodgkin Lymphoma
- Hodgkin lymphoma incidence is 1 in 1,000 to 6,000 during pregnancy.[37]
- For establishing a diagnosis, clinical history and hematological, biochemical tests, and a neck/chest/abdominopelvic MRI are favored over a CT scan. A lymph node biopsy is confirmatory.
- Current evidence strongly suggests using radiotherapy in the supradiaphragmatic disease commonly in cervical and axillary lymphadenopathy in non-pregnant cases for better outcomes.
- As for pregnant patients, Mazonakis et al. demonstrated fetal radiation exposure while using a phantom to deliver radiotherapy of varying field sizes to the cervical lymph nodes, axilla, mediastinum, and the neck/mediastinum.[48] The doses were calculated while keeping three different variables. The reported amounts were all under the threshold of 0.1 Gy causative of any deterministic effects. With proper abdominal shielding and maneuvering of the field sizes and beam modifiers, exposure can be further altered.
- Nuyttens et al. delivered radiotherapy to a 26-year-old pregnant woman with stage IIa Hodgkin lymphoma with cervical lymphadenopathy and mediastinum.[49] During her 2nd trimester at 27 weeks, a standard anterior and posterior mantle field with six megavolts with 19 Gy in 12 fractions was administered over 2.5 weeks without shielding. The estimated fetal dose was between 0.15 to 0.53 Gy. A healthy child was born at term with no complications and did not develop any growth malformations or mental retardations noted in follow-up at eight years old.
- Cygler et al. also administered supradiaphragmatic radiotherapy of 35 Gy in 20 fractions with a standard mantle field to a 23-week pregnant patient.[50] The reported fetal exposure was lower than 0.1 Gy, and a healthy baby was born at term. Nisce et al. also reported similar results while treating seven pregnant patients with Hodgkin lymphoma, all in between the 2nd and 3rd trimester.[51]
- In summary, no significant differences between the babies born to women with Hodgkin compared to those born to healthier mothers compared birth weight, mean gestational age at birth, delivery method, neonatal complications, and resuscitation attempts. Administering radiotherapy in pregnant patients with HL and NHL seems feasible in most circumstances unless the cancer load is massive. Over the last decades, advanced chemotherapy and immunotherapy have decreased radiotherapy volumes, allowing decreased possible fetal exposure to ionizing radiation.
Melanoma
- Melanoma is one of the most commonly diagnosed cancers during pregnancy, with an incidence of 1:1000 pregnancies.[52] Approximately 35% of women diagnosed with melanoma are of childbearing age.
- Surgery is the primary treatment for non-metastatic melanoma. Adjuvant systemic therapy is indicated depending on risk factors such as depth of invasion and nodal status. Radiation therapy is indicated as an adjuvant in high-risk cases such as melanomas of the head and neck region with positive lymph nodes. Radiotherapy is used as an adjuvant or primary therapy for mucosal melanomas, which has an overall poor prognosis in treating brain metastases, or as a palliative treatment for recurrent/metastatic disease in sites other than the central nervous system.
- Because of the aggressive nature of melanomas, delaying radiotherapy until delivery is felt to be not in the best interest of the patient welfare. Thorough treatment planning to minimize radiotherapy to the fetus should be considered.
Head and Neck Cancer
- The incidence of head and neck cancers in pregnancy is significantly low.
- Diagnosis and staging can be safely made using nasal endoscopy and biopsy, MRI, and CXR. CT scans and PET scans are contraindicated.
- Radiotherapy is often given as a primary treatment option; however, depending on the stage, site, and histopathological appearance, it can be administered with either chemotherapy or given after surgery. The radiotherapy dose is usually high, about 60 to 70 Gy, delivered in fractions of 1.8-2 Gy daily over seven weeks. Because of the safe distance between the treatment site and gravid uterus, radiotherapy can be administered during the 2nd and 3rd trimester without compromising fetal outcomes.[53]
- Nuttyens et al. reported administering radiotherapy postoperatively to a patient at 24 weeks of gestation with 64 Gy over 6.5 weeks for her tongue cancer.[49] The estimated fetal dose was 0.027 to 0.086 Gy, and a healthy baby was delivered at term.
- Kourinou et al. demonstrated even lower fetal exposure while treating a patient with nasopharyngeal cancer with reported doses ranging between 0.004 to 0.0171 Gy throughout the three trimesters.[33]
- IMRT is now commonly used for head and neck cancers. This allows better alignment of high dose regions around the tumor; however, it results in large adjacent healthy tissue areas receiving lower but significant radiation doses. Josipovic et al. successfully utilized IMRT when treating a pregnant patient with head and neck cancer and using special shielding to reduce the fetal dose.[54]
Thyroid Cancer
- Thyroid cancer is another common cancer commonly seen in women of the reproductive age group.
- Surgery is the primary treatment for well-differentiated thyroid cancers. However, it is prudent to postpone surgery during pregnancy until after delivery and keep a watchful follow-up using ultrasound imaging and thyroid function tests unless progression is evident.
- Thyroid malignancies are not generally treated using external beam radiotherapy. Instead, radioactive iodine (131-I) is often used to ablate residual thyroid tissue after surgery in non-pregnant cases.
- Radioactive 131-I is contraindicated during pregnancy, and the Nuclear Regulatory Commission recommends not to breastfeed while being treated with radioactive iodine. For relatively rare occurrences of poorly differentiated or anaplastic thyroid cancer during pregnancy, aggressive therapy is warranted with the patient informed decision-making and constant communication within the multi-disciplinary team.
Other Issues
Managing Radiotherapy in Pregnancy
- The fetus is exposed to radiation from doses outside of the treated volume primarily due to photon leakage through the treatment head of the machine, radiation scattered from the collimators, and by beam modifiers such as blocks, multileaf collimators, wedges, and lastly by radiation scattered from treatment beams within the patient. Note that, for photons with energy higher than ten megavolts, there is a possibility of neutron production, which, although small in amount, has a higher bio-toxicity than photons or electrons.
- The most critical factor determining the fetal dose is the distance from the edge of the radiation field while administering external radiotherapy. The dose decreases exponentially with distance.
- Advanced techniques are seemingly counter-productive for dose reduction to healthy maternal and fetal tissue because of low dose bath by IMRT or radiotherapy-rotational methods. Additionally, image-guided radiotherapy is futile to reduce the dose to the pregnancy in utero. On-board cone-beam computed tomography might increase the radiation burden. Also, a significant radiation dose exposure to the fetus could occur from scattering.
- While pregnant, radiotherapy needs specific considerations, and it could only be used in selected cases of breast cancer and lymphomas. Since substantial clinical data is deficient, limiting the role of intensity-modulated radiotherapy and other modern techniques is recommended.
- Shielding:
- Commercially available breast shields reduce female breast dose by 40 to 61%.[17] Thyroid shields have been found to reduce radiation dose to the thyroid by 31 to 57%.
- Shielding of these radiosensitive organs may substantially decrease associated radiation-related risks, especially in children and young adults.
- Once it is decided to proceed with the treatment, fetal exposure can be curtailed by altering the radiation administration technique or combining additional shielding between the treatment machine and the patient. Since this involves carefully choosing beams, angle and beam modifiers, and treatment beam localization techniques, treatment demands a close interaction between radiation oncologists, medical physicists, and medical dosimetrist.
- Perform treatment planning as if the patient was not pregnant and estimate the fetal dose without considering shielding while using a phantom. Remember to incorporate and calculate doses from localization techniques, portal imaging, portal films, or cone beam imaging.
- Technical alterations to the treatment plan that would help minimize the fetal dose.
- Change field size and angle.
- Use photon energy below ten megavolts to evade any possible neutron production.
- Avoid double exposure portal images, mainly if fields are closer to the fetus.
- If fetal exposure is still deemed unacceptable, design, and assemble special shielding.
- Measure fetal doses using a phantom simulation with shielding in place.
- Strictly document the devised treatment plan, including special shielding or technique alterations such as modified portal imaging without double exposure, and thoroughly discuss this plan and tailored new setup with all relevant personnel involved in providing treatment.
- Thoroughly inspect all aspects of safety, including the weight-bearing limits of the couch, swift movement, and comfortable positing of the shields to ensure that there will be no treatment inflicted injury to either the patient or personnel. Photograph the setup of each field for documentation.
- Constantly monitor fetal growth parameters through the entirety of therapy using physical examination and abdominal ultrasound.
- At the end of the treatment, document the total dose received, including the estimate of fetal dose exposure.
- If appropriate equipment and personnel meant to estimate and reduce fetal dose are not available in the local clinical setting, consider referring the patient to another well-equipped institution.
Enhancing Healthcare Team Outcomes
Important considerations for team planning of radiotherapy in pregnant patients:
- Confirm pregnancy based on history (last menstrual period) and ultrasound diagnostics. Note the patient's age, prior obstetric history if present, and any previous surgeries or procedures such as a cesarean section, myomectomy, hysteroscopic probes, and dilation/curettage. If the patient is not presently pregnant, she should be counseled to avoid pregnancy until the end of treatment.
- If the patient is evaluated to be pregnant, the decisions subsequently need to be tailored as per the patient reproductive and treatment goals with strong participation of the patient and the husband, or another appropriate person, the treating oncologist, and additional team members (surgeons, obstetricians, and psychologists).
- Potential hormonal effects of pregnancy on the tumor
- Various therapeutic regimens and their length, efficacy, and complications
- Impact of delaying therapy
- Expected outcomes of maternal ill-health on the fetus
- Gestation period, chorionicity and amnionicity, gestational morbidities (diabetes, Rh incompatibility, oligo/poly-hydramnios)
- Fetal assessment and monitoring (bio-parameters)
- Delivery method: Normal or surgical
- Discussion if the pregnancy should be terminated
- Legal, ethical, and moral binding issues
Informed consent and understanding by the patient are pivotal components before proceeding with the treatment:
- The pregnant patient has a right to know the extent and type of potential radiation effects from in-utero exposure.
- Three significant points should be communicated: consent, role-related responsibility, and remedy/compensation since radiotherapy in a pregnant patient, not only the risks to the mother but the fetus as well. So in this setting, the mother has a role-related responsibility to care for her unborn child and make informed decisions about herself without counter influence.
- The level of disclosure should be related to the risk ascertained. In low dose exposure procedures such as a CXR, a verbal assurance suffices since the risk is significantly low. However, when fetal doses are at 0.001 Gy (1 mGy) and above, a more detailed explanation is essential.
- The oncologist should inform about potential radiation risks and alternative modalities and the potential risks from not having the procedure.
- Comply with any local or institutional laws and rules.
Media
(Click Image to Enlarge)
References
Donegan WL, Cancer and pregnancy. CA: a cancer journal for clinicians. 1983 Jul-Aug; [PubMed PMID: 6407725]
Chiarelli AM,Marrett LD,Darlington GA, Pregnancy outcomes in females after treatment for childhood cancer. Epidemiology (Cambridge, Mass.). 2000 Mar; [PubMed PMID: 11021613]
Level 2 (mid-level) evidenceSignorello LB,Mulvihill JJ,Green DM,Munro HM,Stovall M,Weathers RE,Mertens AC,Whitton JA,Robison LL,Boice JD Jr, Stillbirth and neonatal death in relation to radiation exposure before conception: a retrospective cohort study. Lancet (London, England). 2010 Aug 21; [PubMed PMID: 20655585]
Level 2 (mid-level) evidenceSignorello LB,Cohen SS,Bosetti C,Stovall M,Kasper CE,Weathers RE,Whitton JA,Green DM,Donaldson SS,Mertens AC,Robison LL,Boice JD Jr, Female survivors of childhood cancer: preterm birth and low birth weight among their children. Journal of the National Cancer Institute. 2006 Oct 18; [PubMed PMID: 17047194]
Level 2 (mid-level) evidenceGreen DM,Lange JM,Peabody EM,Grigorieva NN,Peterson SM,Kalapurakal JA,Breslow NE, Pregnancy outcome after treatment for Wilms tumor: a report from the national Wilms tumor long-term follow-up study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010 Jun 10; [PubMed PMID: 20458053]
Critchley HO,Wallace WH, Impact of cancer treatment on uterine function. Journal of the National Cancer Institute. Monographs. 2005; [PubMed PMID: 15784827]
Hartnett KP,Mertens AC,Kramer MR,Lash TL,Spencer JB,Ward KC,Howards PP, Pregnancy after cancer: Does timing of conception affect infant health? Cancer. 2018 Nov 15; [PubMed PMID: 30403424]
Nutting CM,Morden JP,Harrington KJ,Urbano TG,Bhide SA,Clark C,Miles EA,Miah AB,Newbold K,Tanay M,Adab F,Jefferies SJ,Scrase C,Yap BK,A'Hern RP,Sydenham MA,Emson M,Hall E, Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. The Lancet. Oncology. 2011 Feb; [PubMed PMID: 21236730]
Level 1 (high-level) evidenceDawson LA,Sharpe MB, Image-guided radiotherapy: rationale, benefits, and limitations. The Lancet. Oncology. 2006 Oct; [PubMed PMID: 17012047]
GILES D,HEWITT D,STEWART A,WEBB J, Malignant disease in childhood and diagnostic irradiation in utero. Lancet (London, England). 1956 Sep 1; [PubMed PMID: 13358242]
Kato H,Yoshimoto Y,Schull WJ, Risk of cancer among children exposed to atomic bomb radiation in utero: a review. IARC scientific publications. 1989; [PubMed PMID: 2680953]
Brent RL, Protection of the gametes embryo/fetus from prenatal radiation exposure. Health physics. 2015 Feb; [PubMed PMID: 25551507]
De Santis M,Cesari E,Nobili E,Straface G,Cavaliere AF,Caruso A, Radiation effects on development. Birth defects research. Part C, Embryo today : reviews. 2007 Sep; [PubMed PMID: 17963274]
Level 3 (low-level) evidenceToppenberg KS,Hill DA,Miller DP, Safety of radiographic imaging during pregnancy. American family physician. 1999 Apr 1; [PubMed PMID: 10208701]
Gentilini O,Cremonesi M,Trifirò G,Ferrari M,Baio SM,Caracciolo M,Rossi A,Smeets A,Galimberti V,Luini A,Tosi G,Paganelli G, Safety of sentinel node biopsy in pregnant patients with breast cancer. Annals of oncology : official journal of the European Society for Medical Oncology. 2004 Sep; [PubMed PMID: 15319240]
Keleher A,Wendt R 3rd,Delpassand E,Stachowiak AM,Kuerer HM, The safety of lymphatic mapping in pregnant breast cancer patients using Tc-99m sulfur colloid. The breast journal. 2004 Nov-Dec; [PubMed PMID: 15569204]
Loibl S,von Minckwitz G,Gwyn K,Ellis P,Blohmer JU,Schlegelberger B,Keller M,Harder S,Theriault RL,Crivellari D,Klingebiel T,Louwen F,Kaufmann M, Breast carcinoma during pregnancy. International recommendations from an expert meeting. Cancer. 2006 Jan 15; [PubMed PMID: 16342247]
Gradishar WJ,Moran MS,Abraham J,Aft R,Agnese D,Allison KH,Blair SL,Burstein HJ,Dang C,Elias AD,Giordano SH,Goetz MP,Goldstein LJ,Hurvitz SA,Isakoff SJ,Jankowitz RC,Javid SH,Krishnamurthy J,Leitch M,Lyons J,Matro J,Mayer IA,Mortimer J,O'Regan RM,Patel SA,Pierce LJ,Rugo HS,Sitapati A,Smith KL,Smith ML,Soliman H,Stringer-Reasor EM,Telli ML,Ward JH,Wisinski KB,Young JS,Burns JL,Kumar R, NCCN Guidelines® Insights: Breast Cancer, Version 4.2021. Journal of the National Comprehensive Cancer Network : JNCCN. 2021 May 1 [PubMed PMID: 34030128]
Miller RW, Effects of prenatal exposure to ionizing radiation. Health physics. 1990 Jul; [PubMed PMID: 2358359]
Bithell JF,Stewart AM, Pre-natal irradiation and childhood malignancy: a review of British data from the Oxford Survey. British journal of cancer. 1975 Mar; [PubMed PMID: 1156514]
Level 2 (mid-level) evidenceWakeford R,Little MP, Risk coefficients for childhood cancer after intrauterine irradiation: a review. International journal of radiation biology. 2003 May; [PubMed PMID: 12943238]
Level 2 (mid-level) evidenceDe Santis M,Di Gianantonio E,Straface G,Cavaliere AF,Caruso A,Schiavon F,Berletti R,Clementi M, Ionizing radiations in pregnancy and teratogenesis: a review of literature. Reproductive toxicology (Elmsford, N.Y.). 2005 Sep-Oct; [PubMed PMID: 15925481]
Level 3 (low-level) evidenceBrent RL, The effects of embryonic and fetal exposure to X-ray, microwaves, and ultrasound. Clinical obstetrics and gynecology. 1983 Jun; [PubMed PMID: 6851296]
Level 3 (low-level) evidenceOtake M,Schull WJ,Yoshimaru H, A review of forty-five years study of Hiroshima and Nagasaki atomic bomb survivors. Brain damage among the prenatally exposed. Journal of radiation research. 1991 Mar; [PubMed PMID: 1762113]
Committee Opinion No. 723: Guidelines for Diagnostic Imaging During Pregnancy and Lactation. Obstetrics and gynecology. 2017 Oct; [PubMed PMID: 28937575]
Level 3 (low-level) evidenceKato H, Mortality in children exposed to the A-bombs while in utero, 1945-1969. American journal of epidemiology. 1971 Jun; [PubMed PMID: 5562716]
Robert E, Intrauterine effects of electromagnetic fields--(low frequency, mid-frequency RF, and microwave): review of epidemiologic studies. Teratology. 1999 Apr; [PubMed PMID: 10331531]
Wo JY,Viswanathan AN, Impact of radiotherapy on fertility, pregnancy, and neonatal outcomes in female cancer patients. International journal of radiation oncology, biology, physics. 2009 Apr 1; [PubMed PMID: 19306747]
Pridjian G,Rich NE,Montag AG, Pregnancy hemoperitoneum and placenta percreta in a patient with previous pelvic irradiation and ovarian failure. American journal of obstetrics and gynecology. 1990 May; [PubMed PMID: 2339720]
Level 3 (low-level) evidenceLarsen EC,Schmiegelow K,Rechnitzer C,Loft A,Müller J,Andersen AN, Radiotherapy at a young age reduces uterine volume of childhood cancer survivors. Acta obstetricia et gynecologica Scandinavica. 2004 Jan; [PubMed PMID: 14678092]
Level 2 (mid-level) evidenceCritchley HO,Bath LE,Wallace WH, Radiation damage to the uterus -- review of the effects of treatment of childhood cancer. Human fertility (Cambridge, England). 2002 May; [PubMed PMID: 12082209]
Amant F,Loibl S,Neven P,Van Calsteren K, Breast cancer in pregnancy. Lancet (London, England). 2012 Feb 11; [PubMed PMID: 22325662]
Kourinou KM,Mazonakis M,Lyraraki E,Damilakis J, Photon-beam radiotherapy in pregnant patients: can the fetal dose be limited to 10 cGy or less? Physica medica : PM : an international journal devoted to the applications of physics to medicine and biology : official journal of the Italian Association of Biomedical Physics (AIFB). 2015 Feb; [PubMed PMID: 25455441]
Antypas C,Sandilos P,Kouvaris J,Balafouta E,Karinou E,Kollaros N,Vlahos L, Fetal dose evaluation during breast cancer radiotherapy. International journal of radiation oncology, biology, physics. 1998 Mar 1; [PubMed PMID: 9531386]
Level 3 (low-level) evidenceMazonakis M,Varveris H,Damilakis J,Theoharopoulos N,Gourtsoyiannis N, Radiation dose to conceptus resulting from tangential breast irradiation. International journal of radiation oncology, biology, physics. 2003 Feb 1; [PubMed PMID: 12527052]
Wobbes T, Effect of a breast saving procedure on lactation. The European journal of surgery = Acta chirurgica. 1996 May; [PubMed PMID: 8781927]
Level 3 (low-level) evidencePavlidis NA, Coexistence of pregnancy and malignancy. The oncologist. 2002; [PubMed PMID: 12185292]
Hunter MI,Tewari K,Monk BJ, Cervical neoplasia in pregnancy. Part 2: current treatment of invasive disease. American journal of obstetrics and gynecology. 2008 Jul; [PubMed PMID: 18585521]
Alouini S, Rida K, Mathevet P. Cervical cancer complicating pregnancy: implications of laparoscopic lymphadenectomy. Gynecologic oncology. 2008 Mar:108(3):472-7. doi: 10.1016/j.ygyno.2007.12.006. Epub 2008 Jan 16 [PubMed PMID: 18201752]
Level 2 (mid-level) evidenceFavero G,Chiantera V,Oleszczuk A,Gallotta V,Hertel H,Herrmann J,Marnitz S,Köhler C,Schneider A, Invasive cervical cancer during pregnancy: laparoscopic nodal evaluation before oncologic treatment delay. Gynecologic oncology. 2010 Aug 1; [PubMed PMID: 20460189]
Level 2 (mid-level) evidenceAmant F, Berveiller P, Boere IA, Cardonick E, Fruscio R, Fumagalli M, Halaska MJ, Hasenburg A, Johansson ALV, Lambertini M, Lok CAR, Maggen C, Morice P, Peccatori F, Poortmans P, Van Calsteren K, Vandenbroucke T, van Gerwen M, van den Heuvel-Eibrink M, Zagouri F, Zapardiel I. Gynecologic cancers in pregnancy: guidelines based on a third international consensus meeting. Annals of oncology : official journal of the European Society for Medical Oncology. 2019 Oct 1:30(10):1601-1612. doi: 10.1093/annonc/mdz228. Epub [PubMed PMID: 31435648]
Level 3 (low-level) evidenceMorice P,Narducci F,Mathevet P,Marret H,Darai E,Querleu D, French recommendations on the management of invasive cervical cancer during pregnancy. International journal of gynecological cancer : official journal of the International Gynecological Cancer Society. 2009 Dec; [PubMed PMID: 19955951]
Level 2 (mid-level) evidenceBenhaim Y,Pautier P,Bensaid C,Lhommé C,Haie-Meder C,Morice P, Neoadjuvant chemotherapy for advanced stage cervical cancer in a pregnant patient: report of one case with rapid tumor progression. European journal of obstetrics, gynecology, and reproductive biology. 2008 Feb; [PubMed PMID: 17157432]
Level 3 (low-level) evidenceFarahmand SM,Marchetti DL,Asirwatham JE,Dewey MR, Ovarian endodermal sinus tumor associated with pregnancy: review of the literature. Gynecologic oncology. 1991 May; [PubMed PMID: 2050306]
Level 3 (low-level) evidenceHodby K,Fields PA, Management of lymphoma in pregnancy. Obstetric medicine. 2009 Jun; [PubMed PMID: 27582811]
Pinnix CC,Andraos TY,Milgrom S,Fanale MA, The Management of Lymphoma in the Setting of Pregnancy. Current hematologic malignancy reports. 2017 Jun; [PubMed PMID: 28470380]
Amant F,Vandenbroucke T,Verheecke M,Fumagalli M,Halaska MJ,Boere I,Han S,Gziri MM,Peccatori F,Rob L,Lok C,Witteveen P,Voigt JU,Naulaers G,Vallaeys L,Van den Heuvel F,Lagae L,Mertens L,Claes L,Van Calsteren K, Pediatric Outcome after Maternal Cancer Diagnosed during Pregnancy. The New England journal of medicine. 2015 Nov 5; [PubMed PMID: 26415085]
Mazonakis M,Lyraraki E,Varveris C,Samara E,Zourari K,Damilakis J, Conceptus dose from involved-field radiotherapy for Hodgkin's lymphoma on a linear accelerator equipped with MLCs. Strahlentherapie und Onkologie : Organ der Deutschen Rontgengesellschaft ... [et al]. 2009 Jun; [PubMed PMID: 19506818]
Nuyttens JJ,Prado KL,Jenrette JM,Williams TE, Fetal dose during radiotherapy: clinical implementation and review of the literature. Cancer radiotherapie : journal de la Societe francaise de radiotherapie oncologique. 2002 Dec; [PubMed PMID: 12504772]
Level 3 (low-level) evidenceCygler J,Ding GX,Kendal W,Cross P, Fetal dose for a patient undergoing mantle field irradiation for Hodgkin's disease. Medical dosimetry : official journal of the American Association of Medical Dosimetrists. 1997 Summer; [PubMed PMID: 9243468]
Nisce LZ,Tome MA,He S,Lee BJ 3rd,Kutcher GJ, Management of coexisting Hodgkin's disease and pregnancy. American journal of clinical oncology. 1986 Apr; [PubMed PMID: 3717081]
Still R,Brennecke S, Melanoma in pregnancy. Obstetric medicine. 2017 Sep; [PubMed PMID: 29051777]
Yeh SA, Radiotherapy for head and neck cancer. Seminars in plastic surgery. 2010 May; [PubMed PMID: 22550433]
Josipović M,Nyström H,Kjaer-Kristoffersen F, IMRT in a pregnant patient: how to reduce the fetal dose? Medical dosimetry : official journal of the American Association of Medical Dosimetrists. 2009 Winter; [PubMed PMID: 19854389]
Level 3 (low-level) evidence