Introduction
Fibrocystic breast disease is the most common benign type of breast disease, diagnosed in millions of women worldwide. Certain hormonal factors underpin the function, evaluation, and treatment of this disease. Benign breast disease is an umbrella term for various non-malignant lesions, such as tumors, trauma, mastalgia, and nipple discharge.[1]
The above-mentioned benign lesions are not associated with an increased risk for malignancy; however, it associates with an up to 50% risk of developing breast cancer under certain histopathological and clinical circumstances.[2] A palpable mass upon clinical evaluation is evident in both benign and malignant breast conditions. The clinical findings include symptoms such as dimpling of the skin (peau d'orange), thickening, pain, and nipple discharge.[3]
The most common investigative tools to assess for these clinical findings are mammograms and ultrasound.[4]
The main components of the breast are prone to fibrocystic changes during hormonal fluctuations. These components include the stroma, ducts, and lobules of the breast. During the reproductive age, glandular breast tissue has a direct relation to cyclical surges of plasma levels of estradiol and progesterone.[1]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of benign breast disease has demonstrated a strong clinical association with women receiving estrogen and anti-estrogen treatment. The prevalence of benign breast lesions in postmenopausal women receiving estrogens and progestins for over eight years is increased by 1.7 fold. During the Women’s Health Initiative study (WHI), the combined use of estrogen and progestin correlated with a 74% risk of benign breast disease. The use of anti-estrogens led to a 28% reduction in the prevalence of benign proliferative breast disease.[5]
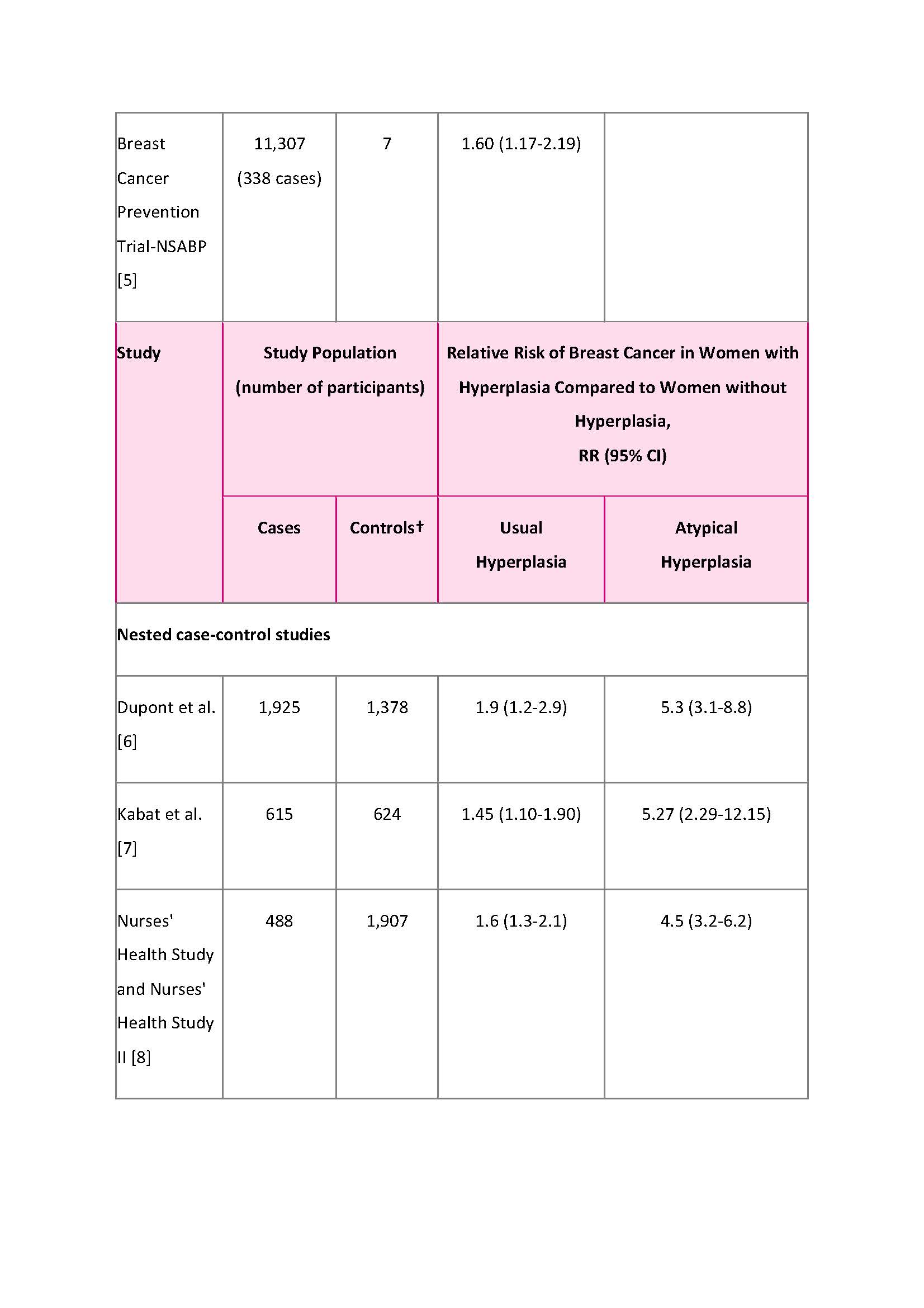
Study selection criteria
The analysis used prospective cohort and nested case-control studies of at least 300 cases and meta-analyses.
See Table 1
* Relative risks estimated from standardized incidence ratios.
† Controls were women who had non-proliferative benign breast disease.[2]
Polycystic ovary syndrome (PCOS) typically presents with factors such as anovulation and hyperandrogenaemia, which is evident in 5 to10% of women within reproductive age.[6]
Previous studies have concluded that hyperestrogenism and anovulation are associated with benign breast conditions, as the growth of glandular breast tissue is affected by the levels of estrogen and progesterone in pathological processes.[7]
Epidemiology
There is varied literature, ranging from 30 to 60% of all women. It is most common in women between the ages of 30 to 50 years.[8]
One of the most common forms of benign breast disease is fibroadenomas, characterized by localized proliferation of breast ducts and stroma. This subtype accounts for 70 to 95% of all tumor benign type of breast disease. The incidence is mostly seen in the 17 to 20 year age group, extending to 2 years premenarche at 35.[3]
Pathophysiology
Mammary gland development, maturation, and differentiation act upon the hormonal and growth factor changes affecting the stromal and epithelial cells.[4]
During the late proliferative phase, glandular tissue evolves to hyperplastic stages such as sclerosing adenosis or lobular hyperplasia. This state of hyperplasia, if associated with a 2% prevalence of Ki67 cells, has a twofold increased incidence for the development of breast cancer.[9]
Various types of benign breast disease exist, such as hyperplasia, cysts, fibroadenomas, sclerosing adenosis, and mastitis.
Histopathology
There is a limited pathological consensus regarding the histopathological appearance of benign breast disease.
The main features are an extracellular matrix of collagen, peri canalicular patterns of stromal cells with the presence of florid epithelial hyperplasia.
During the menopausal phase, fibroadenomas involute, which affects dense collagen stroma and atrophic glands.[10]
Cystic changes derive from the terminal duct lobular unit (TDLU). Due to the expansion of the efferent ductules of the TDLU, cysts form as a result of fluid accumulation in these structures. The lining appears flat with a myoepithelial layer present.[5]
Image 3
Microscopic histology section of fibroadenosis
History and Physical
Benign cysts are typically mobile within the glandular breast tissue, chest wall, and skin and are rubber-like in texture. Except for inflammatory type cysts, discomfort and tenderness experienced by a patient are either absent or mild. Most patients present with multiple cysts upon further clinical and diagnostic evaluation.[11]
Various subtypes of cysts are known, including hyperplastic fibrous cysts, adenosis, and papillomatosis. These types of cysts are usually found in the upper outer quadrants of the breast, as well as in the central margins. The texture upon evaluation ranges from a firm texture to multiple subcentimeter cysts.[12]
Fibroadenomas present in varied sizes with a common oval-shaped, well-defined margin. As with cysts, fibroadenomas are mobile upon evaluation and are often multiple, occurring either simultaneously or over a specified period.[13]
Nipple discharge is associated with ductal ectasia, intraductal papilloma, or in rare instances, carcinoma.
The finding of an intraductal papilloma is associated with a single duct presenting a bloody, sudden discharge with a small palpable nodule in the retro areolar region. Multiple ducts presenting with nonspontaneous, green, yellow, clear discharges are a common feature with duct ectasia.[14]
Evaluation
Triple testing is a combination consisting of clinical examination, imaging, and excision biopsy. This is essential for all women with a clinical finding, such as a discrete palpable mass.
Nodularity in young women less than 30 years of age may have management with clinical surveillance and short-term follow-up examination in 2 to 3 months. An investigation may be necessary if the lump has changed on review or if, at the initial presentation, there is a new change in her breasts.[15] Nodularity or thickening that is asymmetric in women over the age of 30 years, further investigation utilizing mammography and ultrasound, is warranted.
Short-term follow-up is an important part of the management of nodularity so that the progression in size of a mass of nodularity or other associated findings (e.g., skin or nipple changes) is detected.
Mammography with ultrasound examination is required for all discrete palpable lesions in women over 35 to distinguish cysts from solid lesions. Complex cysts containing both fluid and solid matter require biopsy. For solid lesions, radiographically or ultrasonically directed core biopsy provides further information regarding the presence or absence of malignancy.
Core excision biopsy involves a cutting needle with a spring-loaded, automated biopsy instrument that allows sufficient specimen of tissue for histologic analysis.
FNA allows a cytopathologist to evaluate cellular material.[16] However, the amount of material retrieved during FNA procedures being sufficient for diagnosis is non-successful in 35 to 47% of non-palpable lesions. A core biopsy is then the recommendation.[17]
Cytology of nipple discharge has limited specificity and sensitivity to detect malignancy (35 to 47%). If the results of both clinical and diagnostic evaluations are benign, a 6 to 12-month clinical breast examination, ultrasound, and mammography are the suggested follow-up to confirm a stable appearance.
A study of 156 patients in Japan who had a benign breast biopsy showed that 13 percent required a subsequent biopsy within two years of having routine FNA procedures performed. In a retrospective study, 150 patients with benign histology after ultrasound-guided vacuum-assisted biopsy for complex cystic breast lesions (BI-RADS 4) were assessed.
This subset of patients underwent study in 6 monthly intervals. Of the 104 lesions, none led to the development of malignancy.[4]
Routine ultrasound screening in Japan was used with 10519 women to evaluate recall criteria. Researchers noted a cystic-type breast pattern in 6512 cases.
Only one of the patient cases reported malignancy the following year, related to a solid tumor with a cystic component, proven to be a micro-invasive cancer of less than 1 mm.
There was no cancer diagnosed in this subset of patients. Most of the study subjects were less than 40 years of age.[18]
Treatment / Management
Due to the role of estrogen and progesterone treatments, promoting fibrocystic changes in the breast, metformin has been suggested as a treatment method to reduce the excessive cell proliferation caused by associated hormones.[19](B2)
For patients presenting with mastalgia, the first-line options are lifestyle changes. Other suggestions are the use of a supportive bra, as well as altering the dose of hormone replacement therapy regimen.
There is no evidence that reducing caffeine improves fibrocystic breast disease or mastalgia.[20][21](B2)
Analgesics such as aspirin and ibuprofen are options.[22](A1)
Researchers have proposed that a deficiency in prostaglandin E and its precursor gamma-linolenic acid (GLA) increase the sensitivity of breasts during the luteal phase of the menstrual cycle. GLA is subsequently also the active component of evening primrose oil.
Despite not having proven efficacy in previous studies, the use of evening primrose oil is warranted as supportive measures if pain persists despite treatment and advice. A 3 to 6 month period is the suggested timeframe to observe the desired effect[23]
If breast pain is severe for more than six months and disrupts daily activities, other therapies such as tamoxifen, bromocriptine, or danazol can be options. Due to the recurrent nature and long duration of these symptoms, several months of treatment is necessary.
Fluid from cysts aspirated for symptomatic relief does not require cytological assessment. This evaluation is reserved for clinically evident lumps that resolve following the FNA procedure or where the cyst fluid appears macroscopically bloodstained.
Fluid from atypical cysts should have a cytological assessment.[24]
Surgery is indicated for cysts that repetitively, despite frequent FNA, which have an intra-cystic solid appearance on ultrasound or have atypical cells present upon cytopathological evaluation.[25]
Differential Diagnosis
Pertinent Studies and Ongoing Trials
- Thirty patients with fibrocystic breast disease received a clinical trial of danazol. Twenty-three patients had a 5 to 6-month treatment regime.
- Partial or complete relief of breast pain and nodularity for all patients included in the clinical trial.
- The researchers found malignancy in one patient following three months of therapy. There were limited reported side effects.
- Recurrence of symptoms occurred after discontinuation of the drug.[28]
- A study currently being performed in Japan will assess the efficacy and safety of the Xiaoru Sanjie capsule in the treatment of cyclo-mastopathy. The study will be a multicenter, randomized, open controlled clinical study.
Staging
There are not specific characterized stages of benign breast disease used as a standard method of diagnosis; however, fibrocystic type breast disease can be proliferative or non-proliferative types.
Non-proliferative types are not associated with unexpected cell growth. Common non-proliferative lesions would include:-
- Periductal fibrosis
- Nonsclerosing adenosis
- Cysts
- Epithelial-related calcifications
- Mild epithelial hyperplasia
- Papillary apocrine changes.
Non-proliferative lesions are the most common finding in breast cancer screening biopsies, seen in 70% of all cases.
Proliferative changes include factors such as Intraductal hyperplasia, sclerosing adenosis, radial scars, and papillomas.
Prognosis
Proliferative type lesions have a 1.3 to 1.9 times increased risk of malignancy for both breasts.
Any increase in pleomorphic calcifications on mammograms should qualify for a 6-month interval follow-up regime.
Complications
A random sampling of fibrocystic breast disease will often reveal fibrosis if fibrosis is detected using MR-guided sampling. Discordant results should be considered, with further evaluation warranted.[29]
Deterrence and Patient Education
Advice to be provided to patients for preventing and treating fibrocystic breast disease includes:
- Use over-the-counter pain relievers such as acetaminophen or ibuprofen.
- Apply warm or cool compresses to breasts when most painful.
- Wear a comfortable, supportive bra.
- Avoid large amounts of salt or fat in the diet, which some women find can worsen symptoms.
- Consider an oral contraceptive.
Check thyroid levels and suggest the use of iodine.
Consider vitamin E, evening primrose oil, and B vitamins.
Pearls and Other Issues
- A true lateral mammogram can be useful to distinguish benign calcifications from malignant calcifications, such as milk of calcium deposits.[30]
- Diffuse, scattered, similar bilateral findings favor a benign result.
- Focal pain is not a sign of malignancy though ultrasound can serve as a reassurance tool for patients.
- Thermoablation is currently under assessment as a treatment option for benign and malignant lesions.
- The American Society of Breast Surgeons has raised a warning in the assessment and has released a statement for the use of ablative treatment.
- The statement concludes that ablative techniques are currently investigational and should not be performed in the United States unless part of a clinical research trial.[31]
Enhancing Healthcare Team Outcomes
Communicating information about the diagnosis, treatment, and prognosis to patients with breast disease is important for all reported cases in a breast clinic. The best means to accomplish this is an interprofessional team consisting of primary care providers, general surgeons, radiologists, pharmacists, and specialty-trained breast care nurses.
Concerns of patients included the language of physicians, lack of consideration for patient autonomy, and promotion of decision-making power to patients.[32]
Pharmacists become involved when using medications to treat this condition. They counsel patients, review side effects, check for drug interactions, and stress the importance of compliance. Breast care nurses educate patients about the good prognosis and the importance of close follow-up initially. They can also chart progress in treatment, or lack thereof, and inform the lead clinician of any concerns that may arise. These examples of interprofessional collaboration show how the team approach can improve patient outcomes and minimize adverse events. [Level 5]
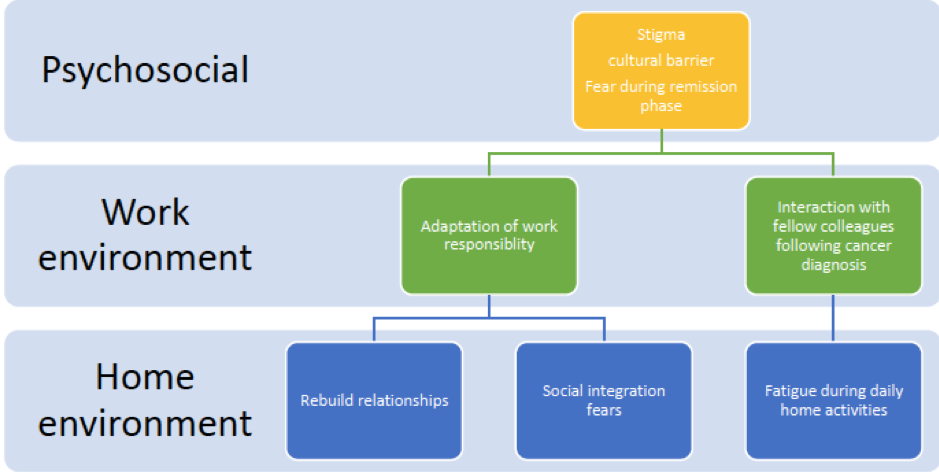
Image 4 and 5: Interprofessional care factors to consider during clinical evaluation of breast disease, both benign and malignant findings.
Psychosocial, home, and work environments require a stable structure to ensure both physical and mental wellbeing. Patients diagnosed with fibrocystic breast disease are also associated with fear and uncertainty due to a lack of education regarding their diagnoses.
Proper medical interaction and interprofessional coordination and communication are necessary to ensure a holistic patient output.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
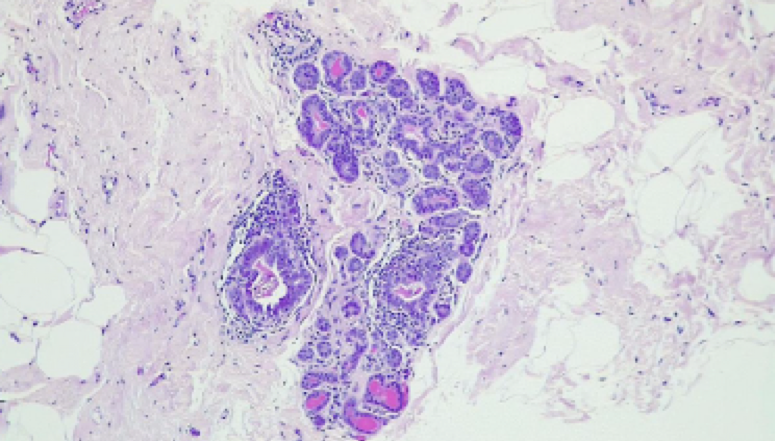
Histologic examination of the specimen submitted confirms female breast tissue with adenosis, epithelial hyperplasia, duct dilatation, chronic inflammation and dystrophic calcifications. There is no evidence of in-situ or invasive malignancy on the material examined. Fibroadenosis with dystrophic calcifications Used with permission and thanks to Lancet Pathology Laboratories, South Africa
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Ameen F, Reda SA, El-Shatoury SA, Riad EM, Enany ME, Alarfaj AA. Prevalence of antibiotic resistant mastitis pathogens in dairy cows in Egypt and potential biological control agents produced from plant endophytic actinobacteria. Saudi journal of biological sciences. 2019 Nov:26(7):1492-1498. doi: 10.1016/j.sjbs.2019.09.008. Epub 2019 Sep 14 [PubMed PMID: 31762615]
McMullen ER, Zoumberos NA, Kleer CG. Metaplastic Breast Carcinoma: Update on Histopathology and Molecular Alterations. Archives of pathology & laboratory medicine. 2019 Dec:143(12):1492-1496. doi: 10.5858/arpa.2019-0396-RA. Epub [PubMed PMID: 31765246]
Danino MA, El Khatib AM, Doucet O, Dao L, Efanov JI, Bou-Merhi JS, Iliescu-Nelea M. Preliminary Results Supporting the Bacterial Hypothesis in Red Breast Syndrome following Postmastectomy Acellular Dermal Matrix- and Implant-Based Reconstructions. Plastic and reconstructive surgery. 2019 Dec:144(6):988e-992e. doi: 10.1097/PRS.0000000000006227. Epub [PubMed PMID: 31764635]
Schünemann HJ, Lerda D, Quinn C, Follmann M, Alonso-Coello P, Rossi PG, Lebeau A, Nyström L, Broeders M, Ioannidou-Mouzaka L, Duffy SW, Borisch B, Fitzpatrick P, Hofvind S, Castells X, Giordano L, Canelo-Aybar C, Warman S, Mansel R, Sardanelli F, Parmelli E, Gräwingholt A, Saz-Parkinson Z, European Commission Initiative on Breast Cancer (ECIBC) Contributor Group. Breast Cancer Screening and Diagnosis: A Synopsis of the European Breast Guidelines. Annals of internal medicine. 2020 Jan 7:172(1):46-56. doi: 10.7326/M19-2125. Epub 2019 Nov 26 [PubMed PMID: 31766052]
Kour A, Sharma S, Sambyal V, Guleria K, Singh NR, Uppal MS, Manjari M, Sudan M, Kukreja S. Risk Factor Analysis for Breast Cancer in Premenopausal and Postmenopausal Women of Punjab, India. Asian Pacific journal of cancer prevention : APJCP. 2019 Nov 1:20(11):3299-3304. doi: 10.31557/APJCP.2019.20.11.3299. Epub 2019 Nov 1 [PubMed PMID: 31759352]
Carvalho MJ, Subtil S, Rodrigues Â, Oliveira J, Figueiredo-Dias M. Controversial association between polycystic ovary syndrome and breast cancer. European journal of obstetrics, gynecology, and reproductive biology. 2019 Dec:243():125-132. doi: 10.1016/j.ejogrb.2019.10.011. Epub 2019 Oct 15 [PubMed PMID: 31693949]
Lundberg FE, Iliadou AN, Rodriguez-Wallberg K, Gemzell-Danielsson K, Johansson ALV. The risk of breast and gynecological cancer in women with a diagnosis of infertility: a nationwide population-based study. European journal of epidemiology. 2019 May:34(5):499-507. doi: 10.1007/s10654-018-0474-9. Epub 2019 Jan 9 [PubMed PMID: 30623293]
Level 2 (mid-level) evidenceGopalani SV, Janitz AE, Martinez SA, Gutman P, Khan S, Campbell JE. Trends in Cancer Incidence Among American Indians and Alaska Natives and Non-Hispanic Whites in the United States, 1999-2015. Epidemiology (Cambridge, Mass.). 2020 Mar:31(2):205-213. doi: 10.1097/EDE.0000000000001140. Epub [PubMed PMID: 31764279]
Rosa M, Agosto-Arroyo E. Core needle biopsy of benign, borderline and in-situ problematic lesions of the breast: Diagnosis, differential diagnosis and immunohistochemistry. Annals of diagnostic pathology. 2019 Dec:43():151407. doi: 10.1016/j.anndiagpath.2019.151407. Epub 2019 Sep 3 [PubMed PMID: 31634810]
Mullooly M, Nyante SJ, Pfeiffer RM, Cora R, Butcher D, Sternberg L, Aiello Bowles EJ, Fan S, Figueroa JD, Weinmann S, Hoover RN, Brinton LA, Berrington de Gonzalez A, Glass A, Sherman ME, Gierach GL. Involution of Breast Lobules, Mammographic Breast Density and Prognosis Among Tamoxifen-Treated Estrogen Receptor-Positive Breast Cancer Patients. Journal of clinical medicine. 2019 Nov 4:8(11):. doi: 10.3390/jcm8111868. Epub 2019 Nov 4 [PubMed PMID: 31689948]
Li YR, Tang YX, Qiu CX, Lin QY, Xie CJ, Zhou MY, Liu YM. [Analysis of common gynecological diseases in 1142 married female workers]. Zhonghua lao dong wei sheng zhi ye bing za zhi = Zhonghua laodong weisheng zhiyebing zazhi = Chinese journal of industrial hygiene and occupational diseases. 2019 Oct 20:37(10):785-788. doi: 10.3760/cma.j.issn.1001-9391.2019.10.015. Epub [PubMed PMID: 31726513]
Level 2 (mid-level) evidenceAutenshlyus AI, Studenikina AA, Bernado AV, Mikhailova ES, Proskura AV, Sidorov SV, Varaksin NA, Lyakhovich VV. [Assessment of the cytokine-producing resource of tumor biopsy samples from patients with invasive carcinoma of no special type and with non-malignant breast diseases]. Biomeditsinskaia khimiia. 2019 Aug:65(5):418-423. doi: 10.18097/PBMC20196505418. Epub [PubMed PMID: 31666415]
Cloete DJ, Minne C, Schoub PK, Becker JHR. Magnetic resonance imaging of fibroadenoma-like lesions and correlation with Breast Imaging-Reporting and Data System and Kaiser scoring system. SA journal of radiology. 2018:22(2):1532. doi: 10.4102/sajr.v22i2.1532. Epub 2018 Nov 7 [PubMed PMID: 31754520]
Li TT, Kang CS, Li HZ, Xue JP, Yang QM, Lyu J. [Value of shear wave elastrography image classification in the diagnosis of breast masses]. Zhonghua zhong liu za zhi [Chinese journal of oncology]. 2019 Jul 23:41(7):540-545. doi: 10.3760/cma.j.issn.0253-3766.2019.07.011. Epub [PubMed PMID: 31357843]
Jafarian AH, Kooshkiforooshani M, Farzad F, Mohamadian Roshan N. The Relationship Between Fibroblastic Growth Factor Receptor-1 (FGFR1) Gene Amplification in Triple Negative Breast Carcinomas and Clinicopathological Prognostic Factors. Iranian journal of pathology. 2019 Fall:14(4):299-304. doi: 10.30699/ijp.2019.96713.1952. Epub 2019 Sep 22 [PubMed PMID: 31754359]
Zhang SC, Hu ZQ, Long JH, Zhu GM, Wang Y, Jia Y, Zhou J, Ouyang Y, Zeng Z. Clinical Implications of Tumor-Infiltrating Immune Cells in Breast Cancer. Journal of Cancer. 2019:10(24):6175-6184. doi: 10.7150/jca.35901. Epub 2019 Oct 15 [PubMed PMID: 31762828]
Huang P, Yao J, Liu X, Luo B. Individualized intervention to improve rates of exclusive breastfeeding: A randomised controlled trial. Medicine. 2019 Nov:98(47):e17822. doi: 10.1097/MD.0000000000017822. Epub [PubMed PMID: 31764775]
Level 1 (high-level) evidenceSawano T, Kambe T, Seno Y, Konoe R, Nishikawa Y, Ozaki A, Shimada Y, Morita T, Saito H, Tsubokura M. High internal radiation exposure associated with low socio-economic status six years after the Fukushima nuclear disaster: A case report. Medicine. 2019 Nov:98(47):e17989. doi: 10.1097/MD.0000000000017989. Epub [PubMed PMID: 31764810]
Level 3 (low-level) evidenceTu C, Ren X, He J, Zhang C, Chen R, Wang W, Li Z. The Value of LncRNA BCAR4 as a Prognostic Biomarker on Clinical Outcomes in Human Cancers. Journal of Cancer. 2019:10(24):5992-6002. doi: 10.7150/jca.35113. Epub 2019 Oct 15 [PubMed PMID: 31762809]
Level 2 (mid-level) evidenceİdiz C, Çakır C, Ulusoy Aİ, İdiz UO. The Role of Nutrition in Women with Benign Cyclic Mastalgia: A Case-Control Study. European journal of breast health. 2018 Jul:14(3):156-159. doi: 10.5152/ejbh.2018.3827. Epub 2018 Jul 1 [PubMed PMID: 30123881]
Level 2 (mid-level) evidenceHorner NK, Lampe JW. Potential mechanisms of diet therapy for fibrocystic breast conditions show inadequate evidence of effectiveness. Journal of the American Dietetic Association. 2000 Nov:100(11):1368-80 [PubMed PMID: 11103660]
Ahiskalioglu A, Yayik AM, Demir U, Ahiskalioglu EO, Celik EC, Ekinci M, Celik M, Cinal H, Tan O, Aydin ME. Preemptive Analgesic Efficacy of the Ultrasound-Guided Bilateral Superficial Serratus Plane Block on Postoperative Pain in Breast Reduction Surgery: A Prospective Randomized Controlled Study. Aesthetic plastic surgery. 2020 Feb:44(1):37-44. doi: 10.1007/s00266-019-01542-y. Epub 2019 Nov 18 [PubMed PMID: 31741068]
Level 1 (high-level) evidenceHaynes BP, Ginsburg O, Gao Q, Folkerd E, Afentakis M, Buus R, Quang LH, Thi Han P, Khoa PH, Dinh NV, To TV, Clemons M, Holcombe C, Osborne C, Evans A, Skene A, Sibbering M, Rogers C, Laws S, Noor L, Smith IE, Dowsett M. Menstrual cycle associated changes in hormone-related gene expression in oestrogen receptor positive breast cancer. NPJ breast cancer. 2019:5():42. doi: 10.1038/s41523-019-0138-2. Epub 2019 Nov 15 [PubMed PMID: 31754627]
Miner N, Meng K. Mammographic architectural distortion caused by cyst aspiration. Acta radiologica open. 2019 Jun:8(6):2058460119859353. doi: 10.1177/2058460119859353. Epub 2019 Jun 28 [PubMed PMID: 31285852]
Youlden DR, Baade PD, Walker R, Pyke CM, Roder DM, Aitken JF. Breast Cancer Incidence and Survival Among Young Females in Queensland, Australia. Journal of adolescent and young adult oncology. 2020 Jun:9(3):402-409. doi: 10.1089/jayao.2019.0119. Epub 2019 Dec 12 [PubMed PMID: 31765264]
Banuelos J, Sabbagh MD, Roh SG, Nguyen MT, Lemaine V, Tran NV, Jacobson SR, Boughey JC, Jakub JW, Hieken TJ, Degnim AC, Mandrekar J, Berbari E, Sharaf B. Infections following Immediate Implant-Based Breast Reconstruction: A Case-Control Study over 11 Years. Plastic and reconstructive surgery. 2019 Dec:144(6):1270-1277. doi: 10.1097/PRS.0000000000006202. Epub [PubMed PMID: 31764629]
Level 2 (mid-level) evidenceFu LM, Sun XJ, Lyu H, Shui RH, Xu XL, Yang WT. [Low grade adenosquamous carcinoma arising from sclerosing adenosis of the breast: report of a case]. Zhonghua bing li xue za zhi = Chinese journal of pathology. 2019 May 8:48(5):415-417. doi: 10.3760/cma.j.issn.0529-5807.2019.05.021. Epub [PubMed PMID: 31104690]
Level 3 (low-level) evidenceBofill Rodriguez M, Lethaby A, Farquhar C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. The Cochrane database of systematic reviews. 2019 Sep 19:9(9):CD000400. doi: 10.1002/14651858.CD000400.pub4. Epub 2019 Sep 19 [PubMed PMID: 31535715]
Level 1 (high-level) evidenceMeattini I, Poortmans P, Kirova Y, Saieva C, Visani L, Salvestrini V, Kim J, Jung W, Olmetto E, Mariotti M, Desideri I, Fourquet A, Livi L, Kim K. Hypofractionated whole breast irradiation after conservative surgery for patients aged less than 60 years: a multi-centre comparative study. Acta oncologica (Stockholm, Sweden). 2020 Feb:59(2):188-195. doi: 10.1080/0284186X.2019.1695061. Epub 2019 Nov 25 [PubMed PMID: 31760849]
Level 2 (mid-level) evidenceUrano M, Nishikawa H, Goto T, Shiraki N, Matsuo M, Denewar FA, Kondo N, Toyama T, Shibamoto Y. Digital Mammographic Features of Breast Cancer Recurrences and Benign Lesions Mimicking Malignancy Following Breast-Conserving Surgery and Radiation Therapy. The Kurume medical journal. 2020 Jan 23:65(4):113-121. doi: 10.2739/kurumemedj.MS654005. Epub 2019 Nov 13 [PubMed PMID: 31723078]
Copelan A, Hartman J, Chehab M, Venkatesan AM. High-Intensity Focused Ultrasound: Current Status for Image-Guided Therapy. Seminars in interventional radiology. 2015 Dec:32(4):398-415. doi: 10.1055/s-0035-1564793. Epub [PubMed PMID: 26622104]
Ghaemi SZ, Keshavarz Z, Tahmasebi S, Akrami M, Heydari ST. Explaining Perceived Priorities in Women with Breast Cancer: A Qualitative Study. Asian Pacific journal of cancer prevention : APJCP. 2019 Nov 1:20(11):3311-3319. doi: 10.31557/APJCP.2019.20.11.3311. Epub 2019 Nov 1 [PubMed PMID: 31759354]
Level 2 (mid-level) evidence