Subjective Refraction Technique: Duochrome Test
Subjective Refraction Technique: Duochrome Test
Introduction
At birth, the ocular structures are fully formed. The eys continuously develop as the neonate grows to reach full refractive status. The developmental process in which the ocular system of the child obtains the expected refractive status is known as emmetropization. Several factors, such as corneal curvature, anterior chamber depth, axial length, and lenticular thickness, are known to be the main determinants of the final refractive outcome.[1]
In early infancy, neonates are known to possess a large corneal curvature dioptric power, which is expected to regress to progressively reach emmetropia. These developmental changes of cornea curvature are usually rapid in the first two to four weeks of life and, subsequently, become slower after eight weeks.[2] As the neonate grows older, the lenticular dioptric power also reduces in a progressive fashion until the optimum lenticular dioptric power is attained.[3] Regardless of the regressive dioptric changes of the cornea curvature and lenticular dioptric power during emmetropization in the early stage of life, changes in the degree of axial length relative to the initial refractive status remain the most critical factor in reaching the required refractive status.[4]
Depending on genetic predisposition and environmental influence, the eye can be considered mostly hyperopic in the early stages of life. Changes in the refractive apparatus of the eye, as well as its axial length at this stage of life, significantly alter the initial refractive status.[5] The relationships between the initial refractive status, subsequent axial length changes, and the consequent change in the resulting refractive error are more consistent with the visual basis of emmetropization, regardless of the significant dioptric changes in the cornea curvature and lenticular dioptric power.[4][6]
Due to the prolate shape of the eye, the parallel light rays passing through the entrance pupil, when focused correctly on the macular, can exceed the retinal limit of the peripheral retinal, known as hyperopic defocus. The process of emmetropisation is theorized to be mostly controlled by the retina.[7][8]
Theoretically, the retina tends to elongate when parallel light rays from an object at infinity are focused behind the retina, which is done to achieve a clear focus. Defocus, therefore, serves as the principal stimulus and the medium in which the retinal exerts control over emmetropization. There is an increased risk of anisometropia when an inequality of increase in axial length occurs in both eyes during childhood development.
The prevalence of anisometropia increases from childhood to teenage years (ages between 5 and 15).[9] Homeostatic failure, described as a dysfunctional emmetropisation, in addition to other conditions (ie, high degree of refractive error at birth), are major risk factors in developing refractive errors.[10]
When determining the degree of optical correction needed to compensate for the refractive deficiency of an ocular system, it is of utmost importance to refine the final spherical dioptric power obtained from prior refractive procedures. The duochrome red-green test can be employed as a standard method of verifying the final refraction.[11] When utilizing this test in astigmatic errors, it is essential for the circle of least confusion to be on the retina to acquire maximum effectiveness.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
The healthcare professional examining patients must have a general background regarding the anatomy and functioning of the visual system, which will be briefly covered in this section. The ocular system is a special sense organ of sight. The ocular system has been designed to interface with rays of light, convert these rays forming images into chemical energy, and then transform these signals into electrical energy. The retinal signal is then transformed into neural information for vision, which is carried by the second-order neurons to the occipital cortex for interpretation.[12]
The visual system comprises various tissues that function together to yield vision, composed of the ocular system (eyeball) and the neural system (retina, optic nerve, frontal eye field, midbrain, thalamus, and visual cortex).
The ocular system is housed in a paired, transversely oval, pear-shaped bony cavity known as the orbit.[13] This structure is a square-shaped pyramid with four walls that measure 35 mm in height and approximately 40mm in width.[14] The superior oblique muscle, in particular, is anchored to the orbit.[15]
The eyelids are moveable folds that shut and open to protect, lubricate and preserve the integrity of the anterior globe.[16] It is lined anteriorly by a thin skin and posteriorly by the conjunctiva. The palpebral conjunctival slopes downwards and upwards across the superior and inferior conjunctival fornix, respectively, to become continuous as the bulbar conjunctival. These structures house the tarsal plate, tarsal glands, orbital septum, sebaceous gland, and lashes. The orifice of the sebaceous gland opens at the lid margin, which permits the excretion of contents into the conjunctival and lid margin.
The inner contents of the eyeball are housed within the confines of the tough outer coat (cornea and sclera). The sclera is a strong, fibrous, opaque, relatively avascular coat of the eyeball. The cornea is a convex, transparent, absolute avascular ocular coat occupying the anterior one-sixth of the eyeball. It derives its nutrition from the tear film, limbal plexus, and aqueous humor. The iris (uvea) can be found posteriorly to the cornea, which acts as a diaphragm by controlling the pupillary aperture.
The intersection of the peripheral iris and cornea forms the anterior chamber angle (iridocorneal angle). The iridocorneal angle is of great interest in congenital mesodermal dysgenesis and glaucoma. The crystalline lens lies posterior to the iris, which is held in place at the equator by the zonular fibers from the ciliary muscle.
Just anterior to the equator, there is a 2 mm wide serrated structure known as the ora serrata. This marks the point of transition of the ciliary body to the retina. The ophthalmic artery provides blood supply. Venous drainage is via the vortex, pterygoid venous plexus veins. The superior and inferior ophthalmic veins also assist in this. Long and short postsynaptic sympathetic and parasympathetic nerves from the ciliary ganglion are carried along to the intrinsic muscles of the ciliary body and iris.
Indications
The duochrome or bichrome test is a refractive method used in refining the spherical endpoint. In routine clinical practice, it is usually performed at the end of the initial maximum-plus-to-maximum-visual acuity (MPMVA). It is also performed after the initial objective and subjective refraction have been achieved. The duochrome test can help achieve the best refractive visual acuity during subjective refraction.[17]
In emmetropia, the optical apparatus of the visual system refracts light rays so that an object's clear, comfortable image at infinity is obtained with active accommodation. In certain instances, however, these optical apparatuses fail to accurately bend light rays incident via the entrance pupil correctly, leading to refractive errors.[18]
During refractive procedures, the duochrome test is indicated for several reasons, which include:
- Balancing accommodation: The equalization of an accommodative response is an essential aspect of the final refractive procedure, which is usually done by equalizing the visual acuity in both eyes.[19] Accommodation equalization in both eyes aims to achieve the following conditions: eliminating every chance of aniseikonia, maintaining the comfort of binocular vision, and eliminating visual dissonance. Equalizing the visual acuity does not necessarily translate to an equalized accommodation due to certain factors such as anisometropia, eye dominance, antimetropia, and chronic noninfective ocular pathologies. A more realistic manner, such as the degree of chromatic focus, can provide the closest approximation of the clinical situation.
- Obtaining the best spherical equivalent: The duochrome test can determine the best spherical equivalent for a given ametropia.[20] This is usually done by assessing the color providing the most distinct image the patient perceives while the eye is fogged.[21] This can be done before or after the cylindrical component refinement.[11]
- Screening to determine the type of refractive error: The duochrome test can be used as a general subjective screening tool to assess if the is myopic, hypermetropic, or emmetropic.
Contraindications
Axial chromatic aberration is an optical phenomenon in which different colors (based on the respective dispersion properties and wavelengths) are focused at different distances due to imperfection of the optical device or refracting surface. The duochrome test thus greatly relies on chromatic aberration and the ability of an individual to perceive the various dispersion properties of light correctly.
Correctly recognizing the individual dispersion properties of light can be hampered in certain conditions, including acquired or congenital dyschromatopsia, rod-cone diseases, brunescent cataracts, and achromatopsia, and patients recovering from corneal transplants.[22][23] These conditions greatly limit the application of this method in obtaining the best spherical equivalent. The duochrome test has been reported to produce a modest amount of overcorrection (over-minus) for myopia and under-correction (under-plus) for hyperopia.[24]
When testing patients showing better monovision than binocular vision, it is essential to consider Fechner’s Paradox.[25] Duchrome testing in these patients may be challenging to assess. Fechner’s Paradox is thought to be caused by the magnification in high-powered lenses, which gives rise to a flawed perception akin to aniseikonia. Patients experiencing this will benefit from monovision training.
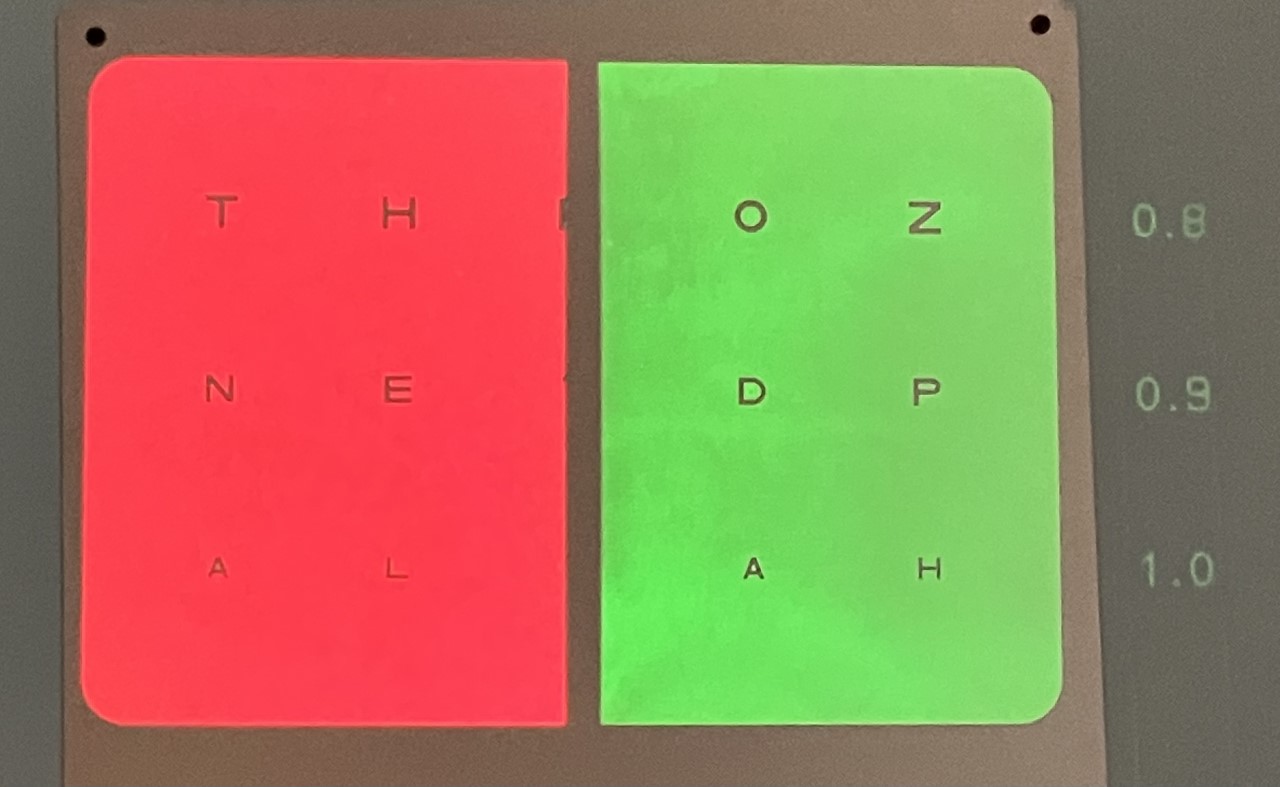
Equipment
The regular duochrome (bichrome) chart is a visual acuity chart projected on an equally divided red and green background. The arrangement may vary for manufacturers. For example, the letters, numbers, and symbols may be projected symmetrically on both backgrounds to yield the desired design. The duochrome test equipment is usually positioned six meters or twenty feet from the patient and is generally contained on the visual acuity chart.
These charts can also be digitally installed in projectors and TV charts (See images of duochrome charts). Dim illumination is preferred when performing the test due to the effect of bright illumination on the pupils and accommodation. Some studies, however, suggest minimal ambient room illumination.[26]
Personnel
Eyecare practitioners, including optometrists and ophthalmologists, evaluate, examine, and manage ocular diseases. The duochrome test can refine the spherical endpoint in measuring spherical refractive errors. Worldwide, especially in underdeveloped countries, the global visual initiative has created an invaluable and productive medium of collaboration and cooperation between various healthcare professionals to eliminate needless blindness.[27]
The duochrome test can aid in achieving the optimum refractive correction when assessing a patient's refractive error. It can be used for screening purposes to determine if the individual has a refractive error (myopic or hypermetropic). Thus, it should be referred to an eye care professional for lens prescription.
Preparation
The refractive tissues of the eyeball are required to be in the best state of health for optimum functionality to be achieved.[28][29] Before any refractive procedure, the status of the ocular and the visual system is usually evaluated to assess if local or systemic pathologies can impact the final outcome of the refractive procedure.[30] Clinicians routinely use slit-lamp biomicroscopy when examining the eye.[31]
The cornea, which possesses two-thirds of the eye's refractive power, can be quickly assessed for defects with the sclerotic scatter technique using the slit lamp.[32] After the initial ocular and systemic health evaluation, the objective refractive status can be obtained using a retinoscope or an autorefractor.[33][34] Subjective refraction is carried out utilizing the maximum plus to maximum visual acuity.
Technique or Treatment
Refractive errors are among the most common treatable eye disorders.[35] Prompt evaluation, diagnosis, and adequate management of refractive errors are necessary to alleviate symptoms and provide the best obtainable corrected visual acuity. Before refining the final spherical equivalent when assessing visual acuity, ocular health status, intra-ocular pressure, and the visual system's objective and subjective refractive status are usually assessed. The objective refraction can be considered the starting point in a series of refractive procedures to obtain the best spherical equivalent for a given ametropia.[36][37] The duochrome test, usually done monocularly, can then be used to refine the final spherical equivalent.
The duochrome test technique involves several steps. The patient is first assessed with refraction and given the best correction. With the initial MPMVA or final refractive lens correction on the trial frame or phoropter in place, the duochrome chart can then be projected. Next, the patient is asked to identify the most distinct and focused letters by comparing them on the green versus the red background of the duochrome chart. If the patient reports the letters in the green background as most distinct, plus lenses are consecutively added using +0.25 DS steps until similar clarity from both backgrounds is achieved. If the patient reports the letters in the red background as most distinct, then minus lenses of -0.25 DS steps are consecutively added until similar clarity of letters in both backgrounds is achieved.
It is, however, commonly seen that most patients do not experience equality in clarity between the red and green halves of the charts. Most patients switch from seeing green as clearer to red and vice-versa. The rule of thumb in these cases is to leave younger patients one step into the green and older patients one step into the red. Pseudophakic patients should be left one step into the green.
A simplified version of the duochrome or bichrome test can also be used as a quick eye screening test to assess a person's global refractive error. This subjective screening method can determine if the individual is emmetropic, hyperopic, or myopic. This type of assessment can be helpful in a population-based setting to determine individuals needing further evaluation from an eye care professional for lens prescription. This type of screening does not provide information regarding the required correction or the severity of the refractive error and is thus not normally used in a routine clinical setting.
The test involves using two colored filters, usually red and green, and a standard eye chart with a white background. First, the patient sits 6 meters or 20 feet from the chart. A red or green filter is placed over one eye with the other occluded. The patient is then asked to read the letters on the eye chart out loud, starting from the top row and working their way down. The colored filter is then switched to green, and the patient rereads the chart with the other eye covered. This is repeated in the contralateral eye. The test results are compared to determine whether the patient is nearsighted, farsighted, or has no significant refractive error. If the patient reads more letters with the red filter, they are likely to be nearsighted (myopic), while if they read more letters with the green filter, they are likely to be farsighted (hyperopic).
This version of the duochrome or bichrome test is a useful screening tool for detecting refractive errors, but it is not a substitute for a comprehensive eye exam. If the test indicates a possible refractive error, the patient should be referred to an eye care professional for further evaluation and treatment.
Complications
Poorly refined endpoint subjective refraction may result in the lead or lag of accommodation with consequent visual and ocular complaints and symptoms.[38][39] The lead of accommodation mostly results when excess minus lenses are prescribed to correct a given ametropia.[40]
The diverging effect of a concave lens ensures the further scattering of parallel light rays incident on it, resulting in a blur that serves as a stimulus for accommodation with a consequent increase in accommodative amplitude. This can present clinically as throbbing eye aches and headaches.
When parallel light rays pass through a convex lens, however, the refracted rays are converged to a point in front of the retinal thus, causing accommodation to relax to obtain a perceived clear image. This can present clinically as blurred vision and asthenopic complaints from repeated attempts to over-relax accommodation. Accurate refinement of endpoint subjective refraction is essential in providing an optimum optical correction.
Clinical Significance
The outcome of a well-managed refractive disorder is usually associated with diminished or complete elimination of symptoms and improved quality of life. Adequate correction is usually necessary for children to prevent amblyopia, loss of interest in studies, loss of educational opportunities, and increased dependency as adults.[41] In adults, optimum vision is vital to providing an enhanced quality of life.
Enhancing Healthcare Team Outcomes
The duochrome test is a valuable method to quickly and correctly ascertain the spherical value of an eye. The technique is simple, and results tend to be close to the eventual spherical endpoint. It is possible to train a member of the interprofessional healthcare team other than the clinician to carry out this test correctly. A properly trained healthcare team can assist the clinician in performing the test when managing patients, which can help to reduce waiting times in the clinic in addressing the refractive needs of the patients.
Media
References
Flitcroft DI. Emmetropisation and the aetiology of refractive errors. Eye (London, England). 2014 Feb:28(2):169-79. doi: 10.1038/eye.2013.276. Epub 2014 Jan 10 [PubMed PMID: 24406411]
Inagaki Y. The rapid change of corneal curvature in the neonatal period and infancy. Archives of ophthalmology (Chicago, Ill. : 1960). 1986 Jul:104(7):1026-7 [PubMed PMID: 3729771]
Gordon RA, Donzis PB. Refractive development of the human eye. Archives of ophthalmology (Chicago, Ill. : 1960). 1985 Jun:103(6):785-9 [PubMed PMID: 4004614]
Mutti DO, Mitchell GL, Jones LA, Friedman NE, Frane SL, Lin WK, Moeschberger ML, Zadnik K. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Investigative ophthalmology & visual science. 2005 Sep:46(9):3074-80 [PubMed PMID: 16123404]
Musa MJ, Zeppieri M. Spectacle Correction of Ametropias. StatPearls. 2023 Jan:(): [PubMed PMID: 36251812]
Groot ALW, Lissenberg-Witte BI, van Rijn LJ, Hartong DT. Meta-analysis of ocular axial length in newborns and infants up to 3 years of age. Survey of ophthalmology. 2022 Mar-Apr:67(2):342-352. doi: 10.1016/j.survophthal.2021.05.010. Epub 2021 Jun 9 [PubMed PMID: 34116120]
Level 3 (low-level) evidenceTroilo D. Neonatal eye growth and emmetropisation--a literature review. Eye (London, England). 1992:6 ( Pt 2)():154-60 [PubMed PMID: 1624037]
Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2004 Aug 19:43(4):447-68 [PubMed PMID: 15312645]
Level 3 (low-level) evidenceDeng L, Gwiazda JE. Anisometropia in children from infancy to 15 years. Investigative ophthalmology & visual science. 2012 Jun 20:53(7):3782-7. doi: 10.1167/iovs.11-8727. Epub 2012 Jun 20 [PubMed PMID: 22589429]
Flitcroft DI. Is myopia a failure of homeostasis? Experimental eye research. 2013 Sep:114():16-24. doi: 10.1016/j.exer.2013.02.008. Epub 2013 Feb 20 [PubMed PMID: 23454097]
Level 3 (low-level) evidenceGantz L, Schrader S, Ruben R, Zivotofsky AZ. Can the red-green duochrome test be used prior to correcting the refractive cylinder component? PloS one. 2015:10(3):e0118874. doi: 10.1371/journal.pone.0118874. Epub 2015 Mar 16 [PubMed PMID: 25775478]
Ungewiss J, Breuninger T, Milenkovic I, Ebenhoch R, Schiefer U. [Structure and function of the visual pathway]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2020 Nov:117(11):1062-1067. doi: 10.1007/s00347-020-01069-7. Epub [PubMed PMID: 32152751]
Lieber S, Fernandez-Miranda JC. Anatomy of the Orbit. Journal of neurological surgery. Part B, Skull base. 2020 Aug:81(4):319-332. doi: 10.1055/s-0040-1715096. Epub 2020 Sep 17 [PubMed PMID: 33072474]
Turvey TA, Golden BA. Orbital anatomy for the surgeon. Oral and maxillofacial surgery clinics of North America. 2012 Nov:24(4):525-36. doi: 10.1016/j.coms.2012.08.003. Epub [PubMed PMID: 23107426]
Maslehaty H, Schultheiss S, Scholz M, Petridis AK. Surgical Anatomy of the Orbit in Human Cadavers-An Endoscopic Pictorial Documentation. Journal of neurological surgery. Part B, Skull base. 2018 Apr:79(2):173-176. doi: 10.1055/s-0037-1606294. Epub 2017 Aug 28 [PubMed PMID: 29868323]
Dailey RA, Wobig JL. Eyelid anatomy. The Journal of dermatologic surgery and oncology. 1992 Dec:18(12):1023-7 [PubMed PMID: 1430562]
Colligon-Bradley P. Red-green duochrome test. Journal of ophthalmic nursing & technology. 1992 Sep-Oct:11(5):220-2 [PubMed PMID: 1469739]
Kaur K, Gurnani B. Subjective Refraction Techniques. StatPearls. 2023 Jan:(): [PubMed PMID: 35593807]
Momeni-Moghaddam H, Goss DA. Comparison of four different binocular balancing techniques. Clinical & experimental optometry. 2014 Sep:97(5):422-5. doi: 10.1111/cxo.12198. Epub [PubMed PMID: 25138746]
BRINKBO B. Duochrome test as an aid in determinations of refraction. Acta ophthalmologica. 1954:32(5):585-8 [PubMed PMID: 14387639]
Musa MJ, Zeppieri M. Principles And Technique Of Fogging During Subjective Refraction. StatPearls. 2023 Jan:(): [PubMed PMID: 36251830]
Musa M, Zeppieri M, Enaholo ES, Salati C, Parodi PC. Adipose Stem Cells in Modern-Day Ophthalmology. Clinics and practice. 2023 Feb 4:13(1):230-245. doi: 10.3390/clinpract13010021. Epub 2023 Feb 4 [PubMed PMID: 36826163]
Musa M, Zeppieri M, Enaholo ES, Chukwuyem E, Salati C. An Overview of Corneal Transplantation in the Past Decade. Clinics and practice. 2023 Feb 14:13(1):264-279. doi: 10.3390/clinpract13010024. Epub 2023 Feb 14 [PubMed PMID: 36826166]
Level 3 (low-level) evidenceSivak JG. The validity of the bichrome (Duochrome) test. American journal of optometry and physiological optics. 1975 Sep:52(9):604-6 [PubMed PMID: 1200132]
Qiu SX, Caldwell CL, You JY, Mendola JD. Binocular rivalry from luminance and contrast. Vision research. 2020 Oct:175():41-50. doi: 10.1016/j.visres.2020.06.006. Epub 2020 Jul 18 [PubMed PMID: 32693182]
Level 2 (mid-level) evidenceRosenfield M, Aggarwala KR, Raul C, Ciuffreda KJ. Do changes in pupil size and ambient illumination affect the duochrome test? Journal of the American Optometric Association. 1995 Feb:66(2):87-90 [PubMed PMID: 7714317]
. The role of optometry in vision 2020. Community eye health. 2002:15(43):33-6 [PubMed PMID: 17491876]
Liu W, Huang D, Guo R, Ji J. Pathological Changes of the Anterior Lens Capsule. Journal of ophthalmology. 2021:2021():9951032. doi: 10.1155/2021/9951032. Epub 2021 May 4 [PubMed PMID: 34055399]
Cosar CB, Sridhar MS. Clinical signs in cornea and ocular surface. Indian journal of ophthalmology. 2018 Feb:66(2):202-206. doi: 10.4103/ijo.IJO_716_17. Epub [PubMed PMID: 29380758]
Ursea R, Silverman RH. Anterior-segment imaging for assessment of glaucoma. Expert review of ophthalmology. 2010 Feb 1:5(1):59-74 [PubMed PMID: 20305726]
Kampik A. Imaging in ophthalmology and need for slit-lamp and ophthalmoscopy examinations. Oman journal of ophthalmology. 2016 May-Aug:9(2):79. doi: 10.4103/0974-620X.184508. Epub [PubMed PMID: 27433032]
Denion E, Béraud G, Marshall ML, Denion G, Lux AL. Sclerotic scatter. Journal francais d'ophtalmologie. 2018 Jan:41(1):62-77. doi: 10.1016/j.jfo.2017.08.003. Epub 2017 Dec 13 [PubMed PMID: 29246385]
Hallak J. Reflections on retinoscopy. American journal of optometry and physiological optics. 1976 May:53(5):224-8 [PubMed PMID: 937499]
Bullimore MA, Fusaro RE, Adams CW. The repeatability of automated and clinician refraction. Optometry and vision science : official publication of the American Academy of Optometry. 1998 Aug:75(8):617-22 [PubMed PMID: 9734807]
Level 1 (high-level) evidenceSchiefer U, Kraus C, Baumbach P, Ungewiß J, Michels R. Refractive errors. Deutsches Arzteblatt international. 2016 Oct 14:113(41):693-702. doi: 10.3238/arztebl.2016.0693. Epub [PubMed PMID: 27839543]
Hastings GD, Marsack JD, Nguyen LC, Cheng H, Applegate RA. Is an objective refraction optimised using the visual Strehl ratio better than a subjective refraction? Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2017 May:37(3):317-325. doi: 10.1111/opo.12363. Epub 2017 Mar 30 [PubMed PMID: 28370389]
Rossato M, Nart A, Messina G, Favro F, Rossato V, Rrutja E, Biancalana V. The Refraction Assessment and the Electronic Trial Frame Measurement during Standing or Sitting Position Can Affect Postural Stability. International journal of environmental research and public health. 2022 Jan 29:19(3):. doi: 10.3390/ijerph19031558. Epub 2022 Jan 29 [PubMed PMID: 35162580]
Labhishetty V, Cholewiak SA, Roorda A, Banks MS. Lags and leads of accommodation in humans: Fact or fiction? Journal of vision. 2021 Mar 1:21(3):21. doi: 10.1167/jov.21.3.21. Epub [PubMed PMID: 33764384]
Enaholo ES, Musa MJ, Zeppieri M. Accommodative Insufficiency. StatPearls. 2023 Jan:(): [PubMed PMID: 36508537]
Momeni-Moghaddam H, Ng JS, Cesana BM, Yekta AA, Sedaghat MR. Accommodative amplitude using the minus lens at different near distances. Indian journal of ophthalmology. 2017 Mar:65(3):223-227. doi: 10.4103/ijo.IJO_545_16. Epub [PubMed PMID: 28440251]
Chukwuyem EC, Musa MJ, Zeppieri M. Prescribing Glasses For Children. StatPearls. 2023 Jan:(): [PubMed PMID: 36256752]