Introduction
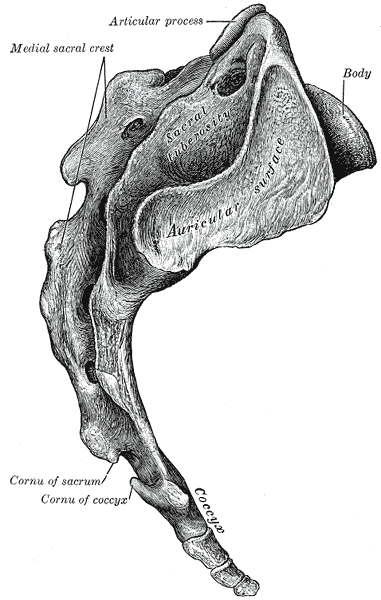
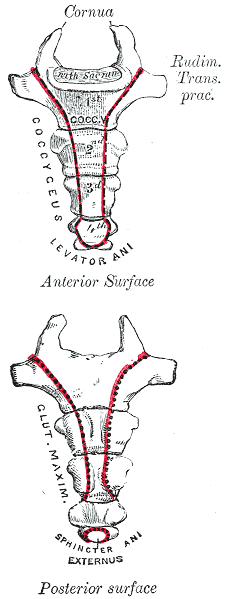
The human coccyx is the final portion of the vertebral column, typically comprised of three to five vertebral segments.[1] Its proximal vertebral segment articulates with the sacrum via a fibrocartilaginous joint; however, the fusion of the sacrum and coccyx has been a feature in many cases, with prevalence differing by age and sex.[2][3] Each inter-vertebral segment has also been shown to differ in the incidence of fusion with its superior and inferior counterparts. Distally, the coccyx maintains a concave-shaped curve and anteriorly angles into the pelvis. Though not readily visible, each coccygeal vertebrae does contain a transverse process and, when fused, forms what is known as the anterior and posterior transverse grooves of the coccyx.
However, the coccygeal vertebrae do not contain any pedicle, lamina, or spinous processes. The coccyx serves as the attachment site for multiple pelvic ligaments and tendons and contains an extensive plexus of coccygeal nerves. Damage to any one of these components can have implications in several clinical conditions.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
Conventional knowledge dictates that the coccyx is a single fused entity; however, magnetic resonance imaging (MRI) and computed tomogram (CT) based evaluations of coccygeal anatomy in different populations have shown that the coccyx contains anywhere from three to five separate bony segments, with the four segments being the most common.[4] Additionally, the fusion between the coccygeal vertebrae is predominantly present within the terminal articulation. The most proximal coccygeal vertebrae are typically the largest and contain processes referred to as coccygeal cornua, which articulate with the superiorly placed sacral cornua.[2]
Together the cornuae form the sacral foramen, allowing for the traversing of various nerves. As the coccygeal vertebra progress, the length and width of each bone decrease, and together form an overall triangular shape. Given its location, the coccyx plays a significant role in weight-bearing when in a seated position and forms a tripod of support along with the two ischial spines of the pelvis.[2] Via ligamentous connection, the coccyx also provides a support point for the anal sphincter.[5]
Embryology
During gastrulation of the human fetus, a trilaminar embryonic disk forms, containing three distinct germ layers (endoderm, mesoderm, ectoderm) along with a notochord, which is adjacent to the neural tube.[6] Between the fourth and fifth weeks of gestation, the mesodermal layer surrounding the notochord differentiates into more specialized paraxial, intermediate, and lateral mesoderm. The paraxial mesoderm then gives rise to about 44 different somites, which will further develop into the future bones of the head, vertebrae, and other bony structures of the human body. By the end of the fifth week, sclerotomes arise from the somites and, under the induction of cellular signals, migrate towards the notochord in a cranial to caudal fashion.
Each sclerotome then divides into a cranial area of loosely packed cells and a caudal area of densely packed cells, between which the intervertebral disk forms. This intervertebral disk separates sclerotomes at different levels and forces the cranial cells of one sclerotome to fuse with the caudal cells of the adjacent somite, thus giving rise to a complete vertebral body. Simultaneously, cells surrounding the neural tube will begin forming vertebral arches to form a protective canal for the future spinal cord. These arches create pedicles, laminae, spinous processes, transverse processes, and articular processes, which ultimately fuse with the developing vertebral bodies, giving rise to the bony spine. Typically during the eighth week of gestation, the sacral and coccygeal vertebrae appear.
Blood Supply and Lymphatics
There are a vast number of vessels that supply the structures of the pelvic region. At the level of L4, the abdominal aorta bifurcates into the internal and external iliac arteries. The internal iliac artery then divides into its anterior and posterior divisions while still located within the pelvis. In contrast, the external iliac continues towards the lower extremities as the femoral arteries.[7]
The posterior division of the internal iliac artery includes the iliolumbar artery, lateral sacral artery, and superior gluteal artery. Ultimately, the lateral sacral artery gives off spinal branches which supply both the sacrum and the coccyx. Additionally, directly from the aorta, median sacral arteries arise near the L4 bifurcation site.[8] These arteries develop anastomoses with the lateral sacral artery branches as well and provide more blood supply to the sacrum and coccyx.
Nerves
The coccygeal plexus primarily innervate the coccygeal vertebrae, a network of nerves originating from the ventral rami of S4, S5, and Co1 along with the dorsal rami of the sacral sympathetic trunk, converging in the area of the iliococcygeus muscle.[9] This plexus also includes anococcygeal nerves that innervate the subcutaneous tissue surrounding the coccygeal vertebrae. Along with the vertebrae and associated musculature, the coccygeal plexus also innervates the sacrospinous ligament, coccygeal ligaments, and periosteum.
Muscles
Anterior to the coccyx vertebrae lie the levator ani muscle along with the sacrococcygeal ligament.[2] The levator ani is a thin, broad muscle divided into the iliococcygeus and pubococcygeus.[10] The iliococcygeus muscle originates at the ischial spine as well as the pelvic fascia and inserts onto the inferior tip of the coccyx. The pubococcygeus, which originates at the pubis, also inserts onto the coccyx as well as the lower portion of the sacrum. Together the muscles constrict, as well as elevate/invert, the lower rectum, thus allowing for voluntary bowel control. Along the lateral edges of the coccyx, there are also insertion sites for the coccygeus muscle (which, along with the levator ani, constitutes the pelvic diaphragm), sacrospinous ligament, the sacrotuberous ligament, as well a the gluteus maximus muscle. Together, the ligaments that attach to the coccyx provide additional stability to the pelvic floor and provide further voluntary control of the bowels.
Clinical Significance
Avulsion injury of the levator ani muscle, specifically of the pubococcygeal segment, is common in postpartum women who have undergone a vaginal delivery.[10] Complications of the injury include pelvic organ prolapse, urinary incontinence, chronic pain, and persistent numbness. Risk factor for avulsion injury includes advanced maternal age, macrosomia, and premature voluntary contractions by the mother. Prospective studies conducted by Diets et al. indicated that 36% of women with vaginal delivery had had a diagnosis of a levator avulsion injury.[11]
Coccydynia refers to pain localized to the coccygeal region, without associated lower back pain or radiation/referral of pain. The condition affects individuals in all age groups; however, onset has typically been shown to be in the fourth decade, with a greater prevalence in women.[12] Patients presenting with the condition also tend to report pain with sitting and report an increased frequency of defecation. The diagnosis is typically clinical. The exact etiology of coccydynia varies; however, the majority of cases appear to be related to subluxated or hypermobile coccygeal structures leading to chronic inflammation. Maigne et al. describe traumatic events occurring one month before the onset of coccydynia as significantly increasing the chances of developing coccydynia.[13] Additionally, a greater body mass index has been shown to increase the risk of coccydynia, with the condition being three times greater in prevalence in obese populations.[14]
Treatment of coccydynia relies on the use of non-steroidal anti-inflammatory drugs (NSAIDs), decreased time spent sitting, sitting modifications (such as "donut" shaped gel pads), as well as physical therapy. Local injections may also be options. Surgical management is typically for patients who have persistent pain despite non-operative management. Excision of any mobile coccygeal segments, coccygectomy, may be utilized; however, post-operative complications such as infection as well as continued pain and neurovascular complications are not uncommon.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Tague RG. Fusion of coccyx to sacrum in humans: prevalence, correlates, and effect on pelvic size, with obstetrical and evolutionary implications. American journal of physical anthropology. 2011 Jul:145(3):426-37. doi: 10.1002/ajpa.21518. Epub 2011 May 3 [PubMed PMID: 21541925]
Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner journal. 2014 Spring:14(1):84-7 [PubMed PMID: 24688338]
Level 3 (low-level) evidenceWoon JT, Perumal V, Maigne JY, Stringer MD. CT morphology and morphometry of the normal adult coccyx. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2013 Apr:22(4):863-70. doi: 10.1007/s00586-012-2595-2. Epub 2012 Nov 29 [PubMed PMID: 23192732]
Level 2 (mid-level) evidenceTetiker H, Koşar MI, Çullu N, Canbek U, Otağ I, Taştemur Y. MRI-based detailed evaluation of the anatomy of the human coccyx among Turkish adults. Nigerian journal of clinical practice. 2017 Feb:20(2):136-142. doi: 10.4103/1119-3077.198313. Epub [PubMed PMID: 28091426]
Nathan ST, Fisher BE, Roberts CS. Coccydynia: a review of pathoanatomy, aetiology, treatment and outcome. The Journal of bone and joint surgery. British volume. 2010 Dec:92(12):1622-7. doi: 10.1302/0301-620X.92B12.25486. Epub [PubMed PMID: 21119164]
Kaplan KM, Spivak JM, Bendo JA. Embryology of the spine and associated congenital abnormalities. The spine journal : official journal of the North American Spine Society. 2005 Sep-Oct:5(5):564-76 [PubMed PMID: 16153587]
de Assis AM, Moreira AM, de Paula Rodrigues VC, Harward SH, Antunes AA, Srougi M, Carnevale FC. Pelvic Arterial Anatomy Relevant to Prostatic Artery Embolisation and Proposal for Angiographic Classification. Cardiovascular and interventional radiology. 2015 Aug:38(4):855-61. doi: 10.1007/s00270-015-1114-3. Epub 2015 May 12 [PubMed PMID: 25962991]
Chenin L, Tandabany S, Foulon P, Havet E, Peltier J. A median sacral artery anterior to the iliocaval junction: a case report-anatomical considerations and clinical relevance for spine surgery. Surgical and radiologic anatomy : SRA. 2018 Jan:40(1):115-117. doi: 10.1007/s00276-017-1917-9. Epub 2017 Sep 5 [PubMed PMID: 28875294]
Level 3 (low-level) evidenceWoon JT, Stringer MD. Redefining the coccygeal plexus. Clinical anatomy (New York, N.Y.). 2014 Mar:27(2):254-60. doi: 10.1002/ca.22242. Epub 2013 Apr 1 [PubMed PMID: 23554024]
Epstein MD, Chew FS. Avulsion of the Levator Ani in a Young Adult Male by Blunt Trauma. Radiology case reports. 2008:3(4):248. doi: 10.2484/rcr.v3i4.248. Epub 2015 Dec 7 [PubMed PMID: 27303567]
Level 3 (low-level) evidenceDietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstetrics and gynecology. 2005 Oct:106(4):707-12 [PubMed PMID: 16199625]
Patel R, Appannagari A, Whang PG. Coccydynia. Current reviews in musculoskeletal medicine. 2008 Dec:1(3-4):223-6. doi: 10.1007/s12178-008-9028-1. Epub [PubMed PMID: 19468909]
Maigne JY, Doursounian L, Chatellier G. Causes and mechanisms of common coccydynia: role of body mass index and coccygeal trauma. Spine. 2000 Dec 1:25(23):3072-9 [PubMed PMID: 11145819]
Fogel GR, Cunningham PY 3rd, Esses SI. Coccygodynia: evaluation and management. The Journal of the American Academy of Orthopaedic Surgeons. 2004 Jan-Feb:12(1):49-54 [PubMed PMID: 14753797]